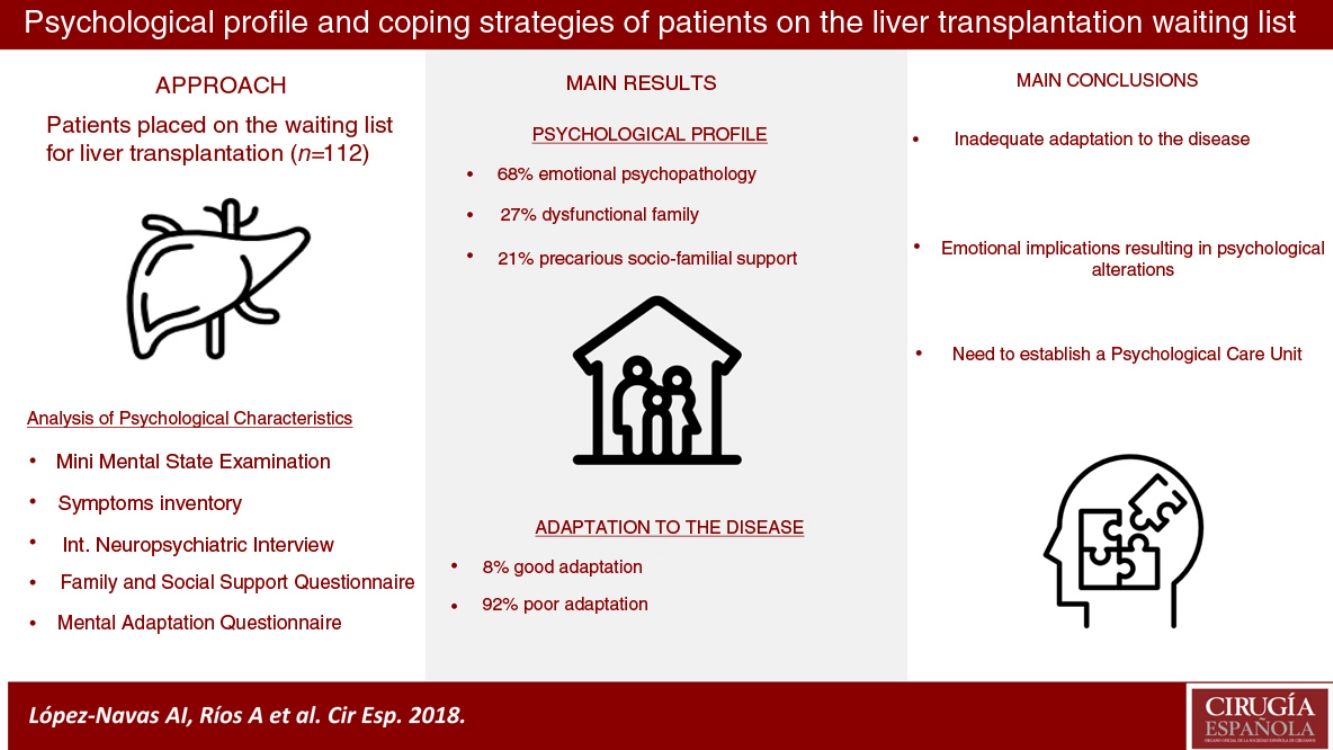
To determine the psychological characteristics of patients on the liver transplant waiting list; to analyze the implications of the patient's psychological profile on coping with the disease.
Material and methodsStudy population: patients on the liver transplant waiting list. Psychological-profile: Socio-personal history; Mini Mental State Examination; Brief-Symptom Inventory of psychopathological problems; International Neuropsychiatric Interview; Family APGAR questionnaire; Social Support Questionnaire. Coping with the disease: A questionnaire about mental adaptation to the disease. Patients were recruited for the study at the time when they were included on the waiting list.
ResultsThe patients (n=112) had the following characteristics: 68% of the patients had symptoms of emotional psychopathology, with 48% being of a depressive, anxious and obsessive–compulsive type, respectively. In terms of social and family support, 27% had the perception of being in a dysfunctional family (slight – 23%; serious – 4%). What is more, according to the Global Support Index, 21% had non-functional social and family support. Coping with the disease: 8% were well-adapted to the disease, the remaining 92% were poorly adapted; of which, 79% had a weaker fighting spirit, 51% expressed anxiety and concern about coping with the disease, 34% found they resorted to fatalism, 29% were in denial and 27% felt helpless.
ConclusionsOnce liver patients are included on the transplant waiting list, they poorly adapt to the disease, with important emotional implications that result in psychological alterations.
Determinar las características psicológicas de los pacientes en lista de espera para trasplante de hígado y analizar las estrategias de afrontamiento de la enfermedad.
MétodosPoblación del estudio: pacientes en lista de espera para trasplante hepático, incluidos consecutivamente en 24 meses. Perfil psicológico: historia socio-personal; Mini Mental State Examination; Inventario breve de síntomas psicopatológicos; Entrevista Neuropsiquiátrica Internacional; Cuestionario familiar APGAR; Cuestionario de Apoyo Social. Hacer frente a la enfermedad: un cuestionario sobre la adaptación mental a la enfermedad. Los pacientes fueron reclutados en el momento en que fueron incluidos en la lista de espera.
ResultadosLos pacientes (n=112) tenían las siguientes características. El 68% de los pacientes tenían síntomas de psicopatología emocional y el 48% eran de tipo depresivo, ansioso y obsesivo-compulsivo, respectivamente. En términos de apoyo social y familiar, el 27% tenía la percepción de estar en una familia disfuncional (leve-23%; grave-4%). Además, según el Índice de soporte global, el 21% no obtenía un funcional apoyo social y familiar. Afrontando la enfermedad: el 8% se encontraba bien adaptado a la enfermedad, el 92% restante estaba mal adaptado; de los cuales, el 79% tenía un espíritu de lucha más débil, el 51% se englobaba en un contexto de ansiedad y preocupación por hacer frente a la enfermedad, el 34% recurría al fatalismo, el 29% mostraba negación y el 27% impotencia.
ConclusionesLos pacientes que son incluidos en lista de espera para un trasplante de hígado presentan dificultades de adaptación a la situación, por lo que desarrollan complicaciones psicológicas relevantes de tipo emocional.
In recent years, significant medical and surgical advances have been made in the transplantation process. Nevertheless, patients on the transplant waiting list experiences stressors, such as the continual wait for the arrival of ‘their’ organ, uncertainties associated with the surgical intervention and postoperative treatment, and changes in lifestyle, all of which can cause psychological alterations.1,2 Furthermore, transplantation usually generates more stress and anxiety than conventional surgery. In transplant patients, psychological complications have been described (mood disorders, anxiety, delirium, fantasies about the donor, and body image dissatisfaction) as well as adaptive disorders (somatic and nutritional).3,4
In a meta-analysis about the psychopathology of transplant patients, Dew et al.5 revealed that 65% have symptoms of depression or anxiety, which are a cause of increased mortality and graft loss. These results raise concern, especially since the World Health Organization has reported that between 8% and 10% of the general population suffer from depression, while between 4% and 6% experience anxiety.6 However, these high percentages are undervalued in clinical practice, even though they lead to morbidity and mortality. In addition, it should be noted that untreated psychiatric comorbidities lead to worsened post-transplantation quality of life. Therefore, detection and treatment are important.
In patients with terminal chronic liver disease, liver transplantation has become the only therapeutic option to increase survival and improve quality of life.7–10 Transplantation is high-risk surgery, where it is necessary to take into account how the patient faces the illness. At present, the average waiting time for a liver graft for transplantation is several months, which favors the development of psychological alterations in the period prior to transplantation.
Despite the growing number of studies on psychological aspects in transplant patients, it is important to point out that there are very few studies on the pre-transplantation phase and specifically in liver transplant recipients.11 Most studies focus on kidney transplant patients.5 Therefore, and to improve the results of transplantation, it is important to study the psychological characteristics of patients on the liver transplant waiting list and to analyze how these are involved in the evolution of the disease. In this way, it will be possible to develop a more comprehensive intervention program, with specific clinical, scientific and social objectives.
The objectives of this study were: (1) to determine the psychological characteristics of patients on the waiting list for liver transplantation; and (2) to analyze the implications of the patients’ psychological profiles in coping with the disease process.
MethodsStudy PopulationThe study population consisted of patients on the waiting list for liver transplantation at a tertiary care hospital with a liver transplant program. Patients who met the following inclusion criteria were included:
- a.
On the waiting list for a liver transplant
- b.
Over the age of 18
- c.
Explicit written informed consent to participate in the study
The exclusion criteria were the following:
- a.
A score of less than 24 on the Mini Mental State Examination (MMSE) cognitive evaluation questionnaire, excluding patients with cognitive abnormalities typical of hepatic encephalopathy higher than grade I
- b.
Under the age of 18
The following assessment tools were applied to study the patients’ psychological characteristics:
Tools to Determine Psychological Profile- 1.
Social and personal background: age, sex, marital status, children, level of education, work experience before and after the illness, address, family support, family history and previous abuse of toxic substances. Clinical history: medical history, date of inclusion on the waiting list, etiology of liver disease, evolution of the disease and other data of interest.
- 2.
MMSE: evaluates the cognitive deterioration of a person using 45 items, in a Spanish version adapted by Lobo et al.12 The reference scores are: 27 or more, normal cognition; 24 or less, suspicion of illness; from 12 to 24, cognitive impairment; and from 9 to 12, possible dementia. This selection tool was part of the exclusion criteria of the study.
- 3.
Symptom Assessment-45 Questionnaire (SA-45): assesses psychopathological symptoms (Spanish version adapted by Sandín13). The questionnaire evaluates 9 basic psychopathological dimensions using 9 scales: somatization disorder, obsessive–compulsive disorder, interpersonal sensitivity, depression, anxiety, hostility, phobic anxiety, paranoid ideation and psychoticism. It is comprised of 45 elements, with Likert-type response options.
- 4.
Mini-International Neuropsychiatric Interview (MINI): uses the clinical diagnosis to establish psychiatric disorders, adapted for the Spanish population by Ferrando et al.14
- 5.
Social Support Survey of the Medical Outcomes Study (MOS): evaluates the size of a person's social network using 4 dimensions of support: (a) emotional support; (b) tangible or instrumental support; (c) positive social interaction (relationships linked to leisure and hobbies); and (d) affectionate support. It consists of 19 items. The questionnaire establishes 3 levels of support according to the Overall Support Index: minimum, average and maximum level. To interpret the results of this study, the term “functional support” has been used when the score is equal to or greater than the mean score, and “non-functional support” when it is lower than the mean score in each of the dimensions. All this is in accordance with the Spanish adaptation by Costa Requena et al.15
- 6.
APGAR family questionnaire: evaluates the perception of the family function of the person interviewed. It consists of 5 items and classifies people according to whether they have a normally functioning family, a slightly dysfunctional family or a severely dysfunctional family. For this purpose, a Spanish adaptation of the questionnaire by Bellón et al.16 was used.
The coping strategies questionnaire of the Mental Adjustment to Cancer (MAC) scale, adapted to Spanish by Ferrero et al.,17 was used because there is no specific questionnaire available for patients of this type. It is a self-report inventory, although in this case it was administered by a professional psychologist due to the clinical characteristics of the patients.
This instrument, which is based on the model by Moorey and Greer18,19 about the types of adaptation to disease, consists of 40 elements with 4 response options: two negative and two positive. Five coping types were identified: fighting spirit, helplessness, anxious preoccupation, hopelessness and denial.
- 1.
Fighting spirit: consists of 16 elements. The minimum score is 16 and the maximum 64, with a cut-off point of 47. A good fighting spirit is reflected by confrontational responses. A poor fighting spirit (score below 47) is determined by the patient's attitude based on her/his difficulty to accept the diagnosis and disease. The emotional reflex is negative, with a tendency toward anxiety and depression.
- 2.
Helplessness: consists of 6 items. The minimum score is 6, the maximum is 24, and the cut-off point is 12. Helplessness (a score of more than 12) usually causes emotional depressive-type alterations in patients. There is a total absence of active fighting strategies.
- 3.
Anxious preoccupation: consists of 9 items. The minimum score is 9, the maximum score is 36, and the cut-off point is 27. As a negative coping strategy, anxious preoccupation (a score higher than 27) is associated with emotional alterations, mainly anxiety-related. In terms of behavior, the answer is based on the compulsive pursuit of calmness.
- 4.
Hopelessness: consists of 8 items. The minimum score is 8, the maximum is 32, and the cut-off point is 24. As an inadequate strategy to cope with the disease (score above 24), hopelessness is based on passive strategies together with serene emotions, which become motivational deficiencies, and negative expectations that can lead to maladaptive behavior patterns.
- 5.
Denial (avoidance): consists of one element in addition to an open question, “What is your disease called?” The minimum score is 2, the maximum score is 8, and the cut-off point is 6. Patients whose coping strategy is negation do not feel threatened by the disease, since denial minimizes the actual diagnosis. Such an inadequate strategy is accompanied by a calm emotional state in the short term, although there are medium- and long-term consequences that are toxic for the management of the disease.
The study had a retrospective single-group ex post facto design. As the patients were added to the transplant waiting list, they were recruited for the study. They were scheduled for an appointment that coincided with their medical check-ups prior to transplantation. The interviews were conducted in the first weeks after being placed on the waiting list. In the consultation, their consent was requested for inclusion in the study, and the MMSE was applied. If the score on this test was greater than 24, the rest of the psychological tests would be applied in the following order: (1) socio-personal background; (2) a brief inventory of psychopathological symptoms; (3) the Mini-International Neuropsychological Interview; (4) the Social and Family Support Questionnaire; (5) the Family APGAR Questionnaire; and (6) the coping strategy questionnaire.
Variables AnalyzedThe study included the following analysis of variables and data:
- a.
Psychological profile: social and personal history; brief inventory of psychopathological symptoms; the MINI; the Social and Family Support Questionnaire; the Family APGAR Questionnaire.
- b.
Variables for coping strategies: fighting spirit; impotence; anxious worry; fatalism; negation.
- c.
Analysis of coping strategies and psychopathology: coping strategies were analyzed as in section b, and the following scales were used to analyze the psychopathological symptoms: somatization disorders; obsessive–compulsive disorders; interpersonal sensitivity; depression; anxiety; hostility; phobic anxiety; paranoid ideation, and psychoticism.
- d.
Evaluation of social and family support, and coping strategies: social and family support was analyzed according to various variables, including emotional, material and instrumental support; social relations associated with leisure and hobbies; affectionate support, love and caring; in addition to the patient's social network and according to the Overall Support Index. The perception of family support could be normally functioning, slightly dysfunctional or severely dysfunctional. As for coping strategies, these have been described in section b above.
A descriptive statistical analysis was carried out and, to compare the different variables, both the Student's t test and the chi-squared test were applied, together with a residual analysis. To determine and evaluate the multiple risks, a logistic regression analysis was performed using the variables that were significantly associated in the bivariate analysis. A P value less than .05 was considered statistically significant.
ResultsPatients Included in the StudyThe study was carried out over 24 months. In this period, 130 patients aged 18 or older were put on the waiting list for deceased donor liver transplantation, 122 of whom met the study inclusion criteria and agreed to participate. The completion rate was 92% (n=112). The reasons why 10 patients did not complete the study were: death before the appointment in 5 patients, frequent hospital admissions that led to cancelation of the interview in 4 patients and the development of grade III hepatic encephalopathy in one patient. Out of the total number of patients (n=112), 28.6% (n=32) presented hepatocellular carcinoma and 71.4% (n=80) cirrhosis.
Psychosocial Profile- 1.
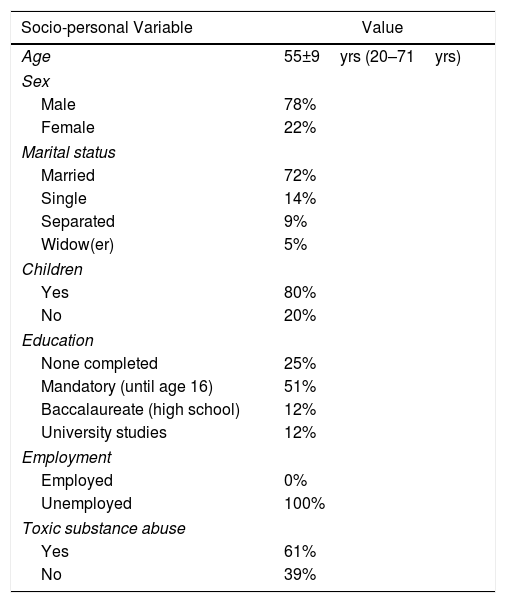
Socio-personal history: The mean age of the respondents was 55±9.1 years; 78% were male and 72% were married. Regarding the level of studies, it is noteworthy that 25% had no formal education and 51% only the minimum requirement. None of the patients were actively working, and 61% indicated problems related to the abuse of toxic substances (Table 1).
Table 1.Description of Socio-personal Characteristics of Patients on the Waiting List for Liver Transplantation.
Socio-personal Variable Value Age 55±9yrs (20–71yrs) Sex Male 78% Female 22% Marital status Married 72% Single 14% Separated 9% Widow(er) 5% Children Yes 80% No 20% Education None completed 25% Mandatory (until age 16) 51% Baccalaureate (high school) 12% University studies 12% Employment Employed 0% Unemployed 100% Toxic substance abuse Yes 61% No 39% - 2.
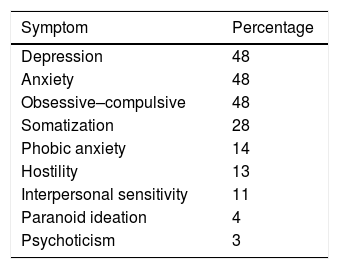
Inventory of psychological and psychopathological symptoms: 68% of the patients evaluated had some type of emotional psychopathological symptom. According to the scales evaluated, 48% of the patients had emotional symptoms of the relevant depressive type, 48% anxiety and 48% obsessive–compulsive symptoms (Table 2).
- 3.
International neuropsychiatric interview: 10% (n=11) of patients presented some type of psychiatric disorder before the liver disease. Of these, 7% (n=8) had mood disorders, 5% of which were major depression, while 1% presented dysthymia and 1% bipolar disorder. The remaining 3% (n=3) presented generalized anxiety disorder.
- 4.
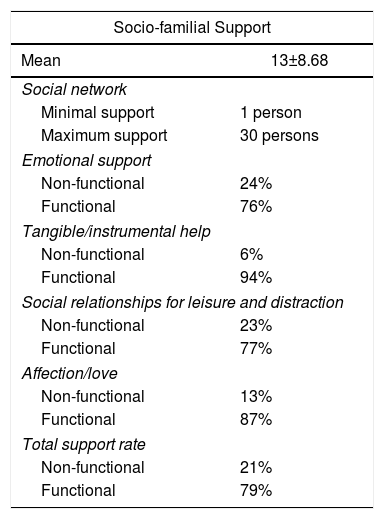
Social and Family Support Questionnaire: The average size of the social network was 13±8.676. According to the Overall Support Index, 21% of the patients evaluated received non-functional social or family support (score <56). The results in the four dimensions were: (a) emotional support: 24% of the patients evaluated had non-functional support in this dimension (score <23); (b) material or instrumental support: 6% had non-functional support in this dimension (score <11); (c) leisure and hobbies related to social relationships: 23% were not functional in this area (score <11); and (d) affective support linked to expressions of love and care: 13% of patients did not have functional support (score <8) (Table 3).
Table 3.Socio-familial Support of Patients on the Waiting List for Liver Transplantation.
Socio-familial Support Mean 13±8.68 Social network Minimal support 1 person Maximum support 30 persons Emotional support Non-functional 24% Functional 76% Tangible/instrumental help Non-functional 6% Functional 94% Social relationships for leisure and distraction Non-functional 23% Functional 77% Affection/love Non-functional 13% Functional 87% Total support rate Non-functional 21% Functional 79% - 5.
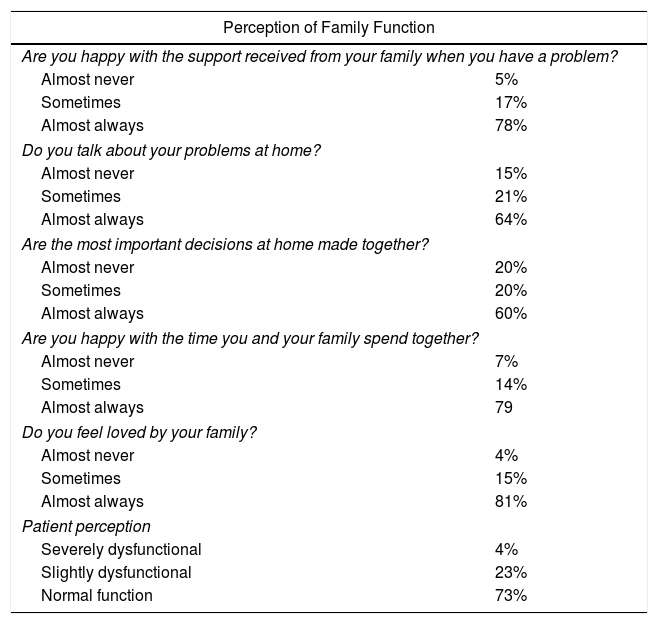
Socio-familial perception questionnaire: 27% of patients had the perception of having a dysfunctional family, 23% of which were slightly dysfunctional and 4% severely dysfunctional. The remaining 73% reported having a normally functioning family (Table 4).
Table 4.Perception of the Family Function in Patients in the Waiting List for Liver Transplantation.
Perception of Family Function Are you happy with the support received from your family when you have a problem? Almost never 5% Sometimes 17% Almost always 78% Do you talk about your problems at home? Almost never 15% Sometimes 21% Almost always 64% Are the most important decisions at home made together? Almost never 20% Sometimes 20% Almost always 60% Are you happy with the time you and your family spend together? Almost never 7% Sometimes 14% Almost always 79 Do you feel loved by your family? Almost never 4% Sometimes 15% Almost always 81% Patient perception Severely dysfunctional 4% Slightly dysfunctional 23% Normal function 73%
Only 8% were well adapted to the disease. Of the remaining 92%, 79% reported less of a fighting spirit, 51% used anxious preoccupation as a coping strategy, 34% used hopelessness, 29% denial and 27% helplessness.
- 1.
Fighting spirit: 79% (n=88) of those evaluated had inadequate fighting spirit to cope with the disease. Of these, 89% also used some type of maladaptive strategy: 53% anxious preoccupation, 39% hopelessness, 31% helplessness and 27% denial.
- 2.
Helplessness: 27% (n=30) used this type of coping strategy, which also showing signs of other patterns of maladaptation: 93% with a lower fighting spirit, 57% anxious preoccupation, 53% hopelessness and 17% denial.
- 3.
Anxious preoccupation: 51% (n=57) reported this pattern. In addition, other strategies were associated with this way of coping, such as a poor fighting spirit (84%), helplessness (30%), hopelessness (28%) and denial (25%).
- 4.
Hopelessness: 34% (n=38) of those evaluated presented this poor adaptation behavior. In addition, 90% used an inadequate fighting spirit, 42% helplessness and anxious preoccupation and 29% denial.
- 5.
Denial: 29% (n=32) reported having this pattern. Of these, 10% used this as their only strategy. The remaining 90% associated it with other inadequate adaptation strategies, such as poor fighting spirit in 77% of cases, anxious preoccupation in 45%, hopelessness in 36% and helplessness in 16%.
- –
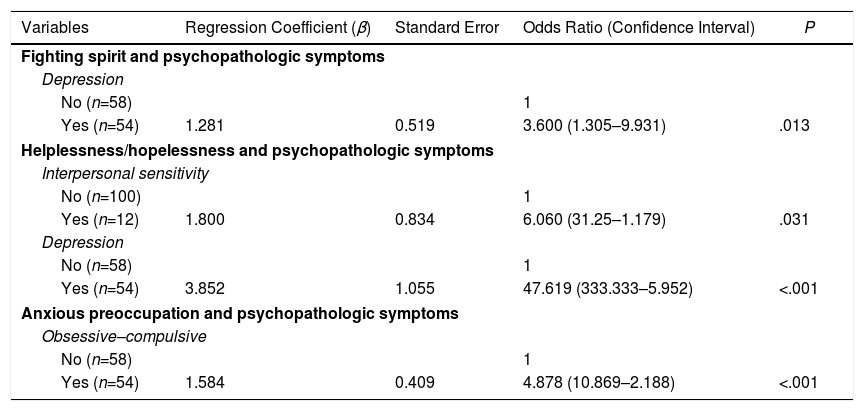
Fighting spirit: Regarding the relationship between different coping strategies and psychopathological symptoms, patients with an inadequate fighting spirit turned out to be those who had a higher rate of depression symptoms (89% vs 69%, P=.010). In the multivariate analysis, a correlation was observed between the “fighting spirit” coping strategy and the presence of psychopathological symptoms of depression, with an OR of 3.600 (P=.013) (Table 5).
Table 5.Factors Influencing Disease-coping Strategies and the Presence of Psychopathologic Symptoms in Patients on the Waiting List for Liver Transplantation; a Multivariate Analysis.
Variables Regression Coefficient (β) Standard Error Odds Ratio (Confidence Interval) P Fighting spirit and psychopathologic symptoms Depression No (n=58) 1 Yes (n=54) 1.281 0.519 3.600 (1.305–9.931) .013 Helplessness/hopelessness and psychopathologic symptoms Interpersonal sensitivity No (n=100) 1 Yes (n=12) 1.800 0.834 6.060 (31.25–1.179) .031 Depression No (n=58) 1 Yes (n=54) 3.852 1.055 47.619 (333.333–5.952) <.001 Anxious preoccupation and psychopathologic symptoms Obsessive–compulsive No (n=58) 1 Yes (n=54) 1.584 0.409 4.878 (10.869–2.188) <.001 - –
Helplessness or despair: Four psychopathological dimensions were associated with the coping type based on helplessness or despair: somatization disorders (45% vs 18%; P=.004); interpersonal sensitivity (83% vs 19%; P<.001); depression (54% vs 0%; P<.001); and anxiety (43% vs 10%, P<.001). In the multivariate analysis, the association between interpersonal sensitivity (OR=6.060; P=.031) and depression (OR=47.619; P<.001) was maintained (Table 5).
- –
Anxious preoccupation: This strategy was associated with obsessive–compulsive symptoms (70% vs 31%; P<.001), depression (61% vs 39%; P=.037) and anxiety (63% vs 38%; P=.008). In the multivariate analysis, the association with obsessive–compulsive symptoms was maintained (OR=4.878; P<.001) (Table 3).
- –
Hopelessness and coping strategies based on denial did not demonstrate relevant associations with the psychopathological dimensions evaluated.
Upon analyzing the correlation between coping strategies and social and family relationships, the following aspects were significant:
- –
Patients with less of a fighting spirit had greater non-functional/dysfunctional social and family support, with significant differences in emotional support (93% vs 74%; P=.042) and in affectionate support related with expressions of love and care (100% vs 75%; P=.030).
- –
Patients who used helplessness or despair as a disease-coping strategy presented the following characteristics at a higher rate: dysfunction in the different areas of social and family support; emotional support (59% vs 16%; P<.001); tangible and instrumental support (86% vs 23%, P<.001); social relationships involving leisure and hobbies (58% vs 17%; P<.001); and affectionate support, love and care (73% vs 20%; P<.001). The overall rate maintained this difference: 58% non-functional versus 18% functional (P<.001). In the multivariate analysis, the results showed a maintained relationship between the patients with “helplessness/despair” and the non-functional emotional support, with an OR of 3.623 (P=.049).
- –
As for anxious preoccupation, hopelessness and denial, the patients who reported having these disease-coping strategies did not obtain relevant differences in the functionality in any type of social and family support (P<.05).
- –
In reference to the patient's perception of family function, it is noteworthy that, among the patients who had an inadequate fighting spirit, 93% perceived family support as dysfunctional, compared to 73% who perceived it as functional (P=.021). In the case of helplessness, family dysfunction was 57% (16% normal functional; P<.001). No statistically significant results were observed for the other types of coping strategies evaluated.
As psychiatric comorbidity is a factor for poor prognosis in disease, more and more medical services are including a psychologist in their protocols. Thus, areas such as Oncology, Palliative Care, Pain Management and Spinal Cord Injuries include psychological care in their multidisciplinary patient management. Other departments are initiating its implementation, such as Cardiology, Dermatology (especially for patients with psoriasis), Emergency Care and Rheumatology.20 However, despite the increasingly significant scientific evidence, the presence of psychological alterations among patients continues to be underestimated in clinical practice.
In the transplantation process, there is a growing awareness of the need for psychosocial assessment of patients who are on waiting lists11,21–23 in order to detect risk factors for a poor prognosis. In patients with terminal chronic liver disease who are candidates for liver transplantation, the clinical circumstances associated with liver disease, along with transplantation waiting times, have an effect on several personal aspects of patients. These are biological and physical in nature, yet there are also psychological and social consequences. Faced with all these changes, patient strategies for coping with the disease are essential and defined as “constantly changing cognitive and behavioral efforts to manage specific internal and/or external demands that are appraised as taxing or exceeding the resources of the person.”24 Most studies on the psychological characteristics of transplantation have been conducted post-transplantation and mainly in kidney recipients. In contrast, it should be noted that our study was performed in patients awaiting liver transplantation.
In the initial design of the present study, patients were evaluated between one and three weeks after being placed on the waiting list. We believe that scheduling patients within the initial days would favor homogeneous psychological responses.
Strategies for coping with disease are crucial, since they reflect the cognitive scheme of the patient for dealing with the diagnosis, control of the disease and expectations in terms of disease progression and prognosis.11,18,25 In addition, the disease-coping style determines the patient's psychological morbidity, and psychopathological reactions can lead to changes in behavior.18,24,26
Research groups that have studied the influence of different strategies to cope with disease26–29 indicate that active coping strategies are more beneficial for dealing with disease than passive ones.27,28 Thus, styles characterized by helplessness and hopelessness entail the presence of depression, while a greater ‘fighting spirit’ is associated with non-depressed patients.28 This associative pattern is frequently found in patients waiting for transplantation, regardless of the organ.11,26,29
In this study, only 8% of patients adapted to the disease adequately after being placed on the waiting list for liver transplantation. This type of coping strategy enables them to confront the diagnosis like a challenge, with a perceived degree of control and an optimistic view of the prognosis. This survival scheme allows patients to develop an active role in their recovery along with a positive emotional tone, although there may be mild anxiety. The remaining 92% adapted poorly to the disease. The most common strategy among these patients was that of a weaker fighting spirit. Furthermore, most used some type of maladaptive pattern, such as anxious preoccupation, helplessness, hopelessness or denial, all of which generate a negative emotional tone in the patient, making them especially depressed and anxious.
In addition to how to deal with the disease, social and family support is a very influential prognostic factor that affects the wellbeing of a person in any situation. Therefore, it is being increasingly analyzed in different clinical services.30–32 Inadequate or limited social or family support contributes to the development of physical, psychological and psychosomatic symptoms in the patient30–32 that can become pathological and, as a result, could affect their mental health. Among the patients we evaluated, 21% had non-functional social or family support, while the most deficient areas were emotional support and support derived from positive social interaction related to leisure and hobbies. In addition, the fact that there is a direct relationship between the coping strategies of these patients, the process of their illness and deficient social or family support should be emphasized. Consequently, there will be patients who, in addition to presenting inadequate strategies to cope with the disease, will lack the infrastructure of social and family support in the context of increasing pressure on physical limits caused by the disease.
Given the problems observed, there is a clear need for a Psychological Care Unit integrated in the Liver Transplantation Unit, as these are patients with specific psychological characteristics.3,7 As for the cost and effectiveness of the unit, all transplant centers have an infrastructure to organize the management of patients on the waiting list. Our experience shows that it is possible to detect and manage the psychopathological problems of patients on the waiting list for liver transplantation in a highly effective manner.7 In addition, based on the information presented, it is necessary to design specific psychological care programs for those patients in whom problems are detected. It is also necessary to take into account the need for guidance and psychological care of family members who provide the patients’ closest support throughout the process.11,33–36
In conclusion, patients on the waiting list for liver transplantation adapt to the disease inadequately, which has emotional implications that lead to psychological alterations. Therefore, it is important to establish appropriate psychological care for these patients when they are placed on the waiting list, which should be provided through a Psychological Care Unit.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: López-Navas AI, Ríos A, Vargas Á, Pons JA, Martínez-Alarcón L, Ruiz-Manzanera JJ, et al. Perfil psicológico y estrategias de afrontamiento ante la enfermedad de los pacientes en lista de espera para un trasplante de hígado. Cir Esp. 2019;97:320–328.