Pancreatic endocrine neoplasms are a group of tumors that sporadically affect this gland, although their etiopathogenesis, diagnosis and treatment are still object of debate. The approximate incidence of these neoplasms is from 1 to 2% of all pancreatic tumors1 and their clinical symptoms depend on the production of hormones or biologically active amines.2 The cystic presentation of these tumors is a much rarer situation (approximately 4.5%), which usually makes their preoperative diagnosis difficult. Therefore, they are frequently confused with other cystic neoplasms of the pancreas with different therapeutic approaches, such as serous cystadenomas, mucinous cystic neoplasms, intraductal papillary mucinous neoplasms, and epithelial cysts, among others.3–5
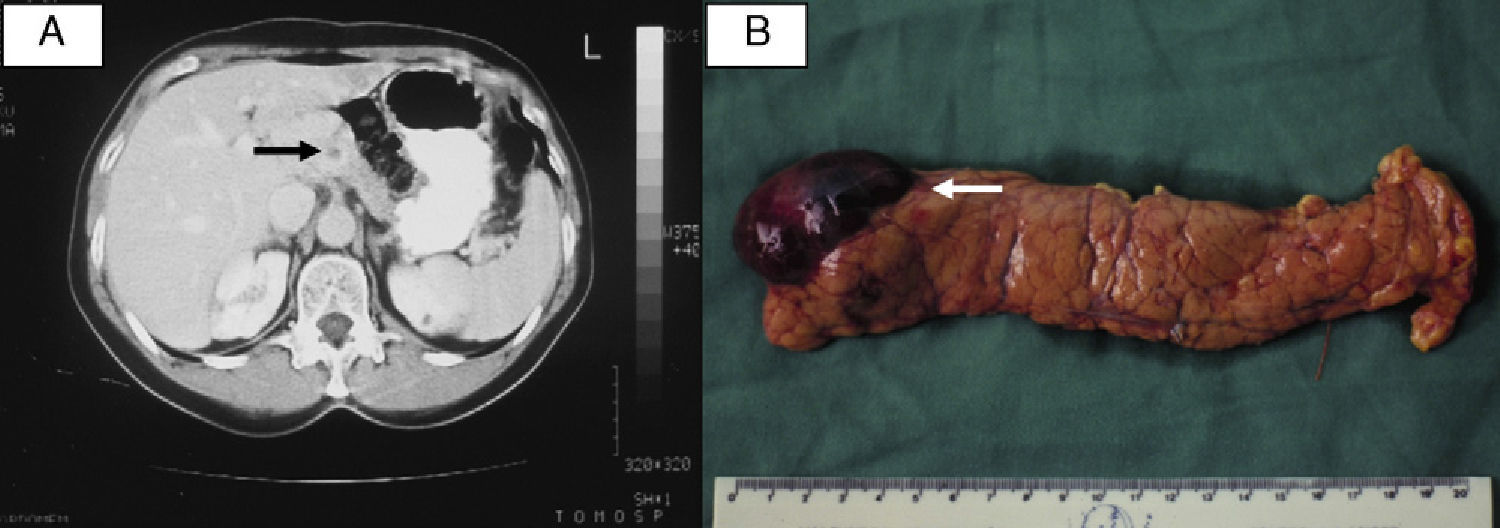
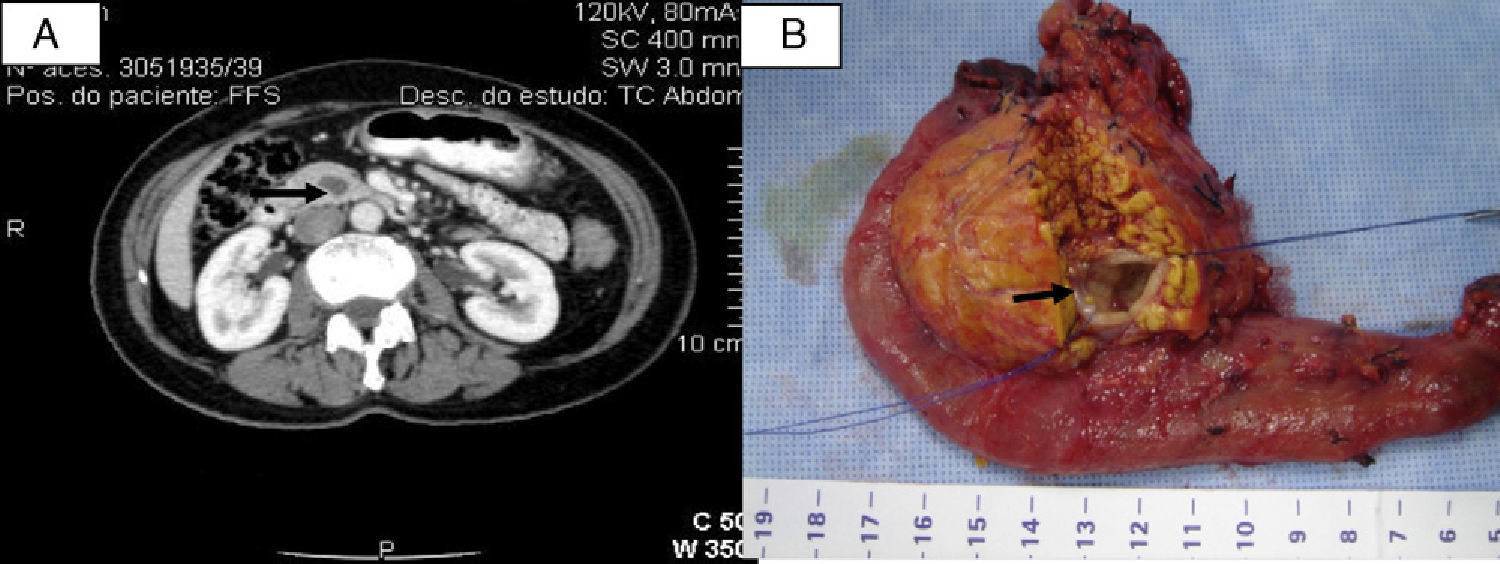
The aim of this letter is to present 3 new cases of non-functioning pancreatic neuroendocrine tumors with predominantly cystic characteristics. The patients are two females, aged 53 and 63, and one male, aged 25. The first two patients presented no specific symptoms. The male patient was in follow-up for a diagnosis of multiple endocrine neoplasia type 1 (MEN-1) and Cushing's disease. The diagnosis of the pancreatic lesions was incidental. Computed tomography showed evidence of a cystic formation with hypodense areas measuring 3.5cm in the body of the pancreas in the first case (Fig. 1A). In the second case, a solid cystic lesion was detected in the uncinate process measuring 1.7cm (Fig. 2A), which was confirmed by endoscopic ultrasound. And, in the third case, magnetic resonance showed a predominantly cystic lesion with cell thickening in the tail of the pancreas measuring 6.2cm. Surgery was indicated in all cases: in the first, pancreatectomy of the body and tail of the pancreas with splenectomy (Fig. 1B); in the second, pylorus-preserving pancreaticoduodenectomy (Fig. 2B); and, laparoscopic distal splenopancreatectomy in the third case. This last patient presented a type ipancreatic fistula in the postoperative period.
Hematoxylin-eosin confirmed the diagnosis of well-differentiated pancreatic endocrine neoplasm, with mitotic index inferior to 10 fields in the 3 cases. Immunohistochemistry showed positivity for chromogranin A, cytoplasmic neuroendocrine marker and neuron-specific enolase in the first case. The second case was positive for chromogranin A, synaptophysin, progesterone receptor 1A6, Mib-1, AE1, AE3 and the proliferation rate (Ki-67) was 5%. In the third patient, this method was positive for somatostatin, enolase monoclonal, chromogranin A, synaptophysin and glucagon, with Ki-67 less than 1%. The first 2 patients had no symptoms in follow-up, and the third patient continues in clinical and endocrinological follow-up.
The development of diagnostic imaging methods in recent decades has undoubtedly resulted in the diagnosis of a series of asymptomatic pancreatic neoplasms, which before would probably have gone undetected with traditional methods. This has also led to controversial situations in the diagnosis and especially the treatment of certain diseases.6
Among these incidental diagnoses, pancreatic endocrine neoplasms are the most frequent.7 Their low incidence causes great diagnostic difficulties due to the absence of characteristic disease symptoms. This diagnostic difficulty can increase when these endocrine tumors adopt a cystic form,8 which is different than what happens in MEN-1.4 There are several theories that try to explain cystic pancreatic endocrine neoplasms.9–12
Imaging methods such as computed tomography and magnetic resonance imaging often confuse this form of presentation of pancreatic endocrine neoplasms with mucinous cystadenomas, cystadenocarcinomas and Frantz tumors due to their common characteristics with these neoplasias.6 Nevertheless, one of the invariably reported characteristics present in cystic pancreatic endocrine neoplasms is the increased vascularization of the cyst wall and, in some cases, the presence of cystic formations in the main cyst.4,5
Diagnostic methods like ultrasound endoscopy should also be considered in some situations, especially in those in which, depending on the magnitude of the surgical procedure, only the confirmation of this type of disease could justify surgery4; this method was used in our second case.
It seems that surgical treatment is the best therapeutic alternative for these patients as it eliminates the possibility for malignant transformation of these neoplasms.8 Depending on the location of these lesions, surgical resection can vary from caudal, central or body-tail pancreatectomy to pancreaticoduodenectomy. When the published series were analyzed, there is a noticeable elevated frequency of distal pancreatectomy, a fact that is justified by the greater tendency of these tumors to be located in these regions of the pancreas.3–5
In spite of the low levels of scientific evidence, we can conclude that cystic endocrine neoplasms are rare situations that can be confused with other diseases13 and that surgical treatment is a good therapeutic option.
Please cite this article as: Apodaca-Torrez FR, de Oliveira ML, Triviño T, Goldenberg A, Lobo EJ. Tumor neuroendocrino quístico no funcionante del páncreas. Una presentación poco usual. Cir Esp. 2015;93:51–52.