Neuroblastic tumors are neoplasms of the sympathetic nervous system originating from primitive sympathetic adrenergic cells formed in the neural crest during embryonic development. They are almost exclusively found in children; their presentation in adults is very rare and associated with a poor prognosis. The location of these tumors is usually intra-abdominal, generally adrenal, and their treatment is surgical whenever possible1. We present the case of a neuroblastic tumor diagnosed in an adult.
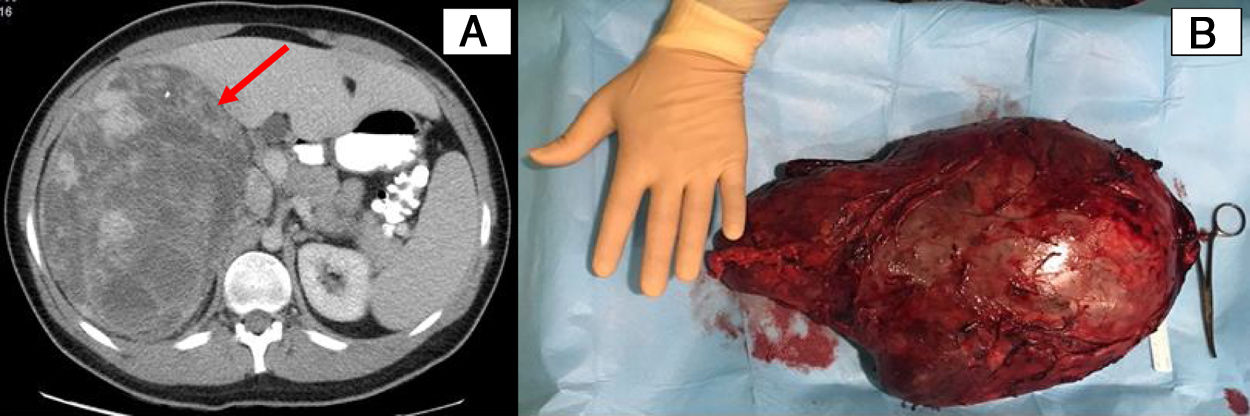
A 22-year-old male patient with no relevant personal history underwent an abdominal ultrasound to study mild, nonspecific, self-limited low back pain, as the origin could not be identified as mechanical and/or urinary. As an incidental finding during this ultrasound, a large right retroperitoneal mass was observed. On examination, a mass was palpable that occupied the entire right hemiabdomen, accompanied by mild local discomfort. The patient did not present obstructive intestinal or urological symptoms, fever, or other symptoms. Lab work demonstrated a slight increase in C-reactive protein (CRP) (1.40mg/dL) and a sedimentation rate of 22mm/h; the remaining parameters were normal. After hospital admittance for further study, a computed tomography (CT) scan revealed a voluminous mass occupying the right hypochondrium and flank. The mass measured 15×20×29cm and appeared to have a retroperitoneal origin (the adrenal gland was an initial possibility), with no evidence of lymphadenopathies or metastatic thoracoabdominal extension (Fig. 1). Catecholamine/metanephrine levels in urine were normal.
A) A heterogeneous mass measuring 15×20×29cm occupying the right hypochondrium and flank, probably adrenal in origin (identified with an arrow); B) Oval, encapsulated surgical piece measuring 35×20cm that corresponded with the tumor mass described in the imaging tests, originating in the right adrenal gland.
At this time, we decided to perform diagnostic-therapeutic surgery. A bilateral subcostal laparotomy revealed a large mass measuring 35×20cm that appeared to originate in the right adrenal gland. It was resected, after identification, ligation and division of the right inferior adrenal artery and vein (Fig. 1b). The histopathological study of the specimen revealed a poorly differentiated intermixed/nodular ganglioneuroblastoma of adrenal origin, with R1 resection margin. Subsequently, the patient was discharged three days after the procedure, with outpatient follow-ups by the Surgery and Oncology Services. On the postoperative 123I-MIBG scintigraphy, there was no evidence of extension at a distance. Treatment with radiotherapy was completed (21Gy [14×1.5Gy]), and the patient was asymptomatic and had no recurrence after 22 months of follow-up.
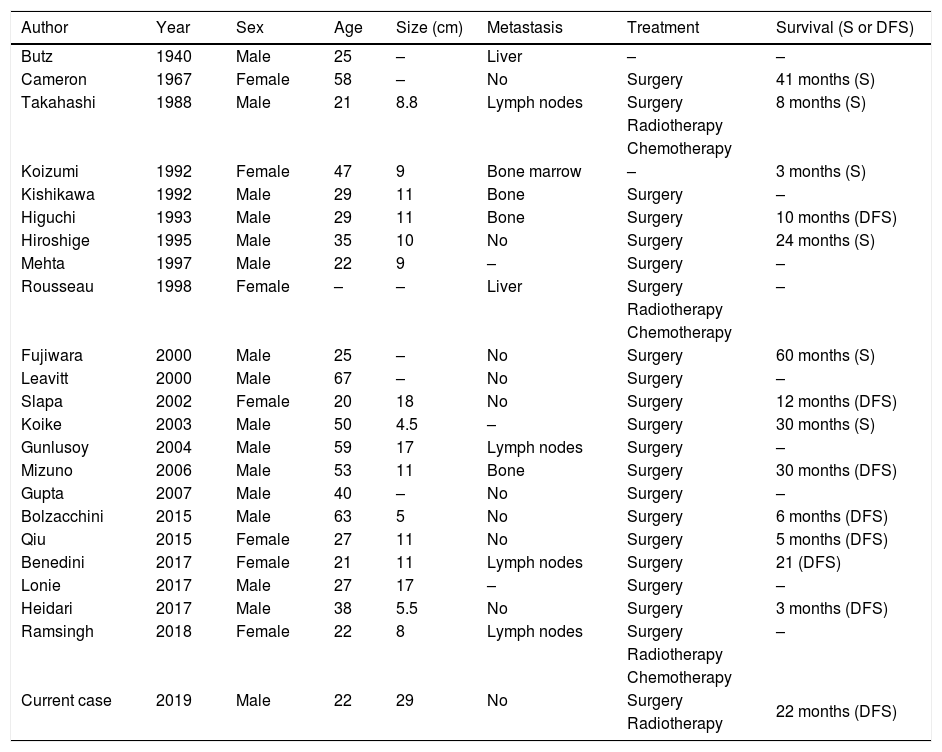
To assess the frequency of adult neuroblastic tumors, a literature review was performed in PubMed, updated on June 26, 2019, with the following search strategy: ganglioneuroblastoma, and adult. There were 22 cases of adult neuroblastoma found in the current literature2,3, 72% of which were males. The median age of the published cases was 29, ranging from 21 to 67 years (Table 1).
Description of worldwide cases of neuroblastic tumors in adults until 20192,3.
| Author | Year | Sex | Age | Size (cm) | Metastasis | Treatment | Survival (S or DFS) |
|---|---|---|---|---|---|---|---|
| Butz | 1940 | Male | 25 | – | Liver | – | – |
| Cameron | 1967 | Female | 58 | – | No | Surgery | 41 months (S) |
| Takahashi | 1988 | Male | 21 | 8.8 | Lymph nodes | Surgery | 8 months (S) |
| Radiotherapy | |||||||
| Chemotherapy | |||||||
| Koizumi | 1992 | Female | 47 | 9 | Bone marrow | – | 3 months (S) |
| Kishikawa | 1992 | Male | 29 | 11 | Bone | Surgery | – |
| Higuchi | 1993 | Male | 29 | 11 | Bone | Surgery | 10 months (DFS) |
| Hiroshige | 1995 | Male | 35 | 10 | No | Surgery | 24 months (S) |
| Mehta | 1997 | Male | 22 | 9 | – | Surgery | – |
| Rousseau | 1998 | Female | – | – | Liver | Surgery | – |
| Radiotherapy | |||||||
| Chemotherapy | |||||||
| Fujiwara | 2000 | Male | 25 | – | No | Surgery | 60 months (S) |
| Leavitt | 2000 | Male | 67 | – | No | Surgery | – |
| Slapa | 2002 | Female | 20 | 18 | No | Surgery | 12 months (DFS) |
| Koike | 2003 | Male | 50 | 4.5 | – | Surgery | 30 months (S) |
| Gunlusoy | 2004 | Male | 59 | 17 | Lymph nodes | Surgery | – |
| Mizuno | 2006 | Male | 53 | 11 | Bone | Surgery | 30 months (DFS) |
| Gupta | 2007 | Male | 40 | – | No | Surgery | – |
| Bolzacchini | 2015 | Male | 63 | 5 | No | Surgery | 6 months (DFS) |
| Qiu | 2015 | Female | 27 | 11 | No | Surgery | 5 months (DFS) |
| Benedini | 2017 | Female | 21 | 11 | Lymph nodes | Surgery | 21 (DFS) |
| Lonie | 2017 | Male | 27 | 17 | – | Surgery | – |
| Heidari | 2017 | Male | 38 | 5.5 | No | Surgery | 3 months (DFS) |
| Ramsingh | 2018 | Female | 22 | 8 | Lymph nodes | Surgery | – |
| Radiotherapy | |||||||
| Chemotherapy | |||||||
| Current case | 2019 | Male | 22 | 29 | No | Surgery | 22 months (DFS) |
| Radiotherapy |
S: survival; DFS: disease-free survival.
Neuroblastic tumors are classified according to the International Neuroblastoma Pathology Classification (INPC) into four categories based on their morphology, clinical characteristics, and behavior: neuroblastoma, nodular ganglioneuroblastoma, intermixed ganglioneuroblastoma, and ganglioneuroma4. Like paragangliomas and pheochromocytomas, some have the ability to synthesize and secrete catecholamines and cause the symptoms derived from their increase.
These are the most common solid tumors in children under the age of five. Their presentation in adults is very rare, since less than 6% of cases are diagnosed in patients over 20 years of age. Their location is most frequently adrenal, followed in frequency by other intra-abdominal, thoracic, cervical, or pelvic node locations. They generally appear as an abdominal mass with associated abdominal or lumbar pain and/or symptoms derived from metastases, which usually affect lymph nodes, bone, orbits, liver, skin, lung and brain. The diagnosis is made with clinical suspicion and imaging tests such as CT or magnetic resonance imaging (MRI). It is necessary to add a study of catecholamines in urine since these tumors can be functional. Both for the extension and follow-up studies, it is necessary to perform 123I-MIBG scintigraphy. Treatment is surgical, whenever possible. Chemotherapy is used in advanced stages to reduce tumor size, while radiotherapy is used as a complement to surgery when complete resection of the tumor has not been achieved. The prognosis in children is good, and survival increases at lower ages of onset. Adults have a poor prognosis, with 3-year and 5-year survival rates of 46% and 36%, respectively. All the cases in adults that exist in the current literature have a survival of less than 20 years from diagnosis5,6. This case represents a poor prognosis given the age of the patient and his poor differentiation in the anatomopathological characteristics, although the follow-up is still too short to draw prognostic conclusions.
In conclusion, although the onset of neuroblastic tumors in adults is very rare (there are very few cases published in the current literature) and has a poor prognosis, the case we report remains in remission 22 months after surgical and radiotherapy treatment.
Please cite this article as: Baeza Murcia M, Valero Navarro G, Flores Pastor B, García Marín JA, Aguayo Albasini JL. Tumores neuroblásticos en el adulto. Cir Esp. 2021;99:159–161.