Multicystic biliary tract hamartoma is a rare cystic disease of the liver, of which only 8 cases have been published worldwide as of 20121. It is usually asymptomatic, and, in most published series, it is diagnosed incidentally or as a result of autopsy studies2.
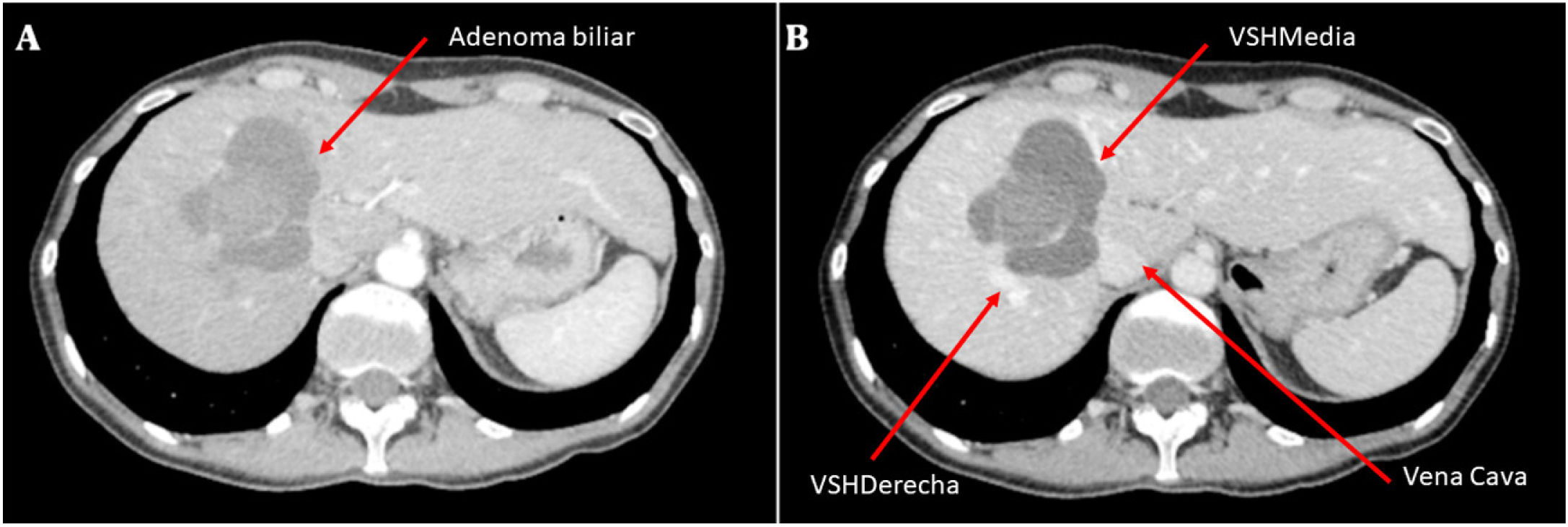
We present the case of a 45-year-old woman, with no relevant personal history, with clinical symptoms of epigastric abdominal pain over several months and no other associated symptoms. An abdominal ultrasound scan was performed, followed by magnetic resonance imaging (MRI), which revealed a polylobulated cystic liver lesion with internal septa, located between segments VII–VIII, measuring approximately 6.5 × 6 × 6.5 cm. The peripheral loculations showed fluid content, while the central loculation showed heterogeneous haemorrhagic content. An angio-CT scan was also performed (Fig. 1), with findings compatible with biliary cystic neoplasia, and a PET/CT scan, with no evidence of SOL uptake. Laboratory results showed no abnormalities, and CEA and Ca 19.9 values were normal.
Computed tomography angiography (CT angiography), showing a polylobulated, septated cystic liver lesion, located between segments VII–VIII, of approximately 6.5 × 6 × 6.5 cm. (A) Arterial phase. Arrow: biliary adenoma. (B) Portal phase. Arrows: right suprahepatic vein (SHV), middle SHV, vena cava.
It was decided to perform elective surgery via right subcostal laparotomy, showing a hepatic SOL in segments VII and VIII with apparent infiltration of the right suprahepatic vein, without free fluid or other hepatic or peritoneal lesions. A right hepatectomy was performed with resection of diaphragmatic pastille of approximately 5 × 5 cm due to infiltration by the tumour. A sample of the intracystic fluid was taken, which was sterile and showed cytological findings of extensive tumour necrosis and few atypical cells suspicious of adenocarcinoma.
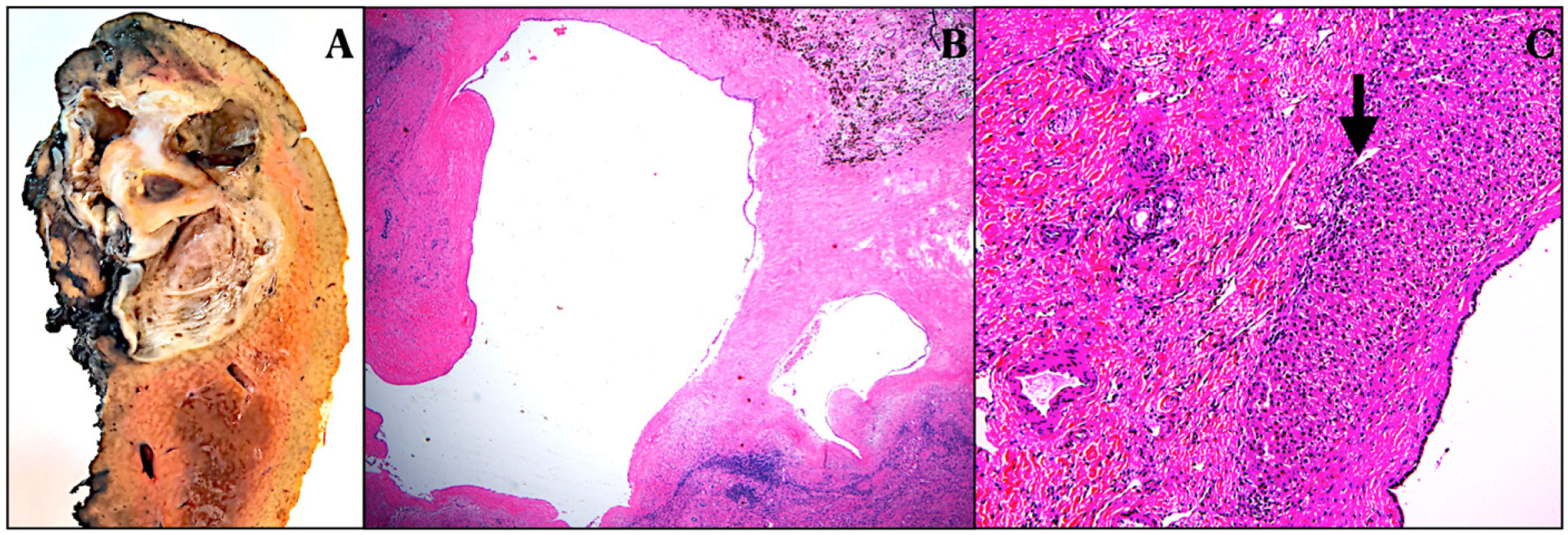
The final anatomopathological analysis showed a right hepatectomy specimen with multiple cysts lined with biliary epithelium, without atypia, with the presence of haemorrhagic content, thrombosis and partial recanalisation in the largest cyst, without identifying ovarian-like stroma, all indicative of multicystic biliary hamartoma (Fig. 2). No other abnormalities were identified in the rest of the liver parenchyma.
(A) Right hepatectomy specimen with identification of a multicystic lesion with cavities between .3–4 cm in diameter with abundant haematic content inside, located immediately proximal to the right SHV. (B) Multiple cysts lined with cylindrical or cuboidal biliary epithelium without atypia, with areas of haemorrhage at the periphery. H&E staining. 10× magnification. (C) Cysts lined by cuboidal biliary epithelium without atypia and interposed liver tissue (arrow). No ovarian-type stroma is observed in the lamina propria of any of the cysts. H&E staining. 10× magnification.
The patient progressed favourably and was discharged home on the fifth postoperative day without complications.
Multicystic biliary hamartoma was first described in 20061 as a rare lesion of unknown aetiology2, characterised by irregular and branched bile ducts with a malformed appearance.
It is considered a benign liver malformation originating as a result of a disturbance in the bile duct cells triggered by a disruptive or ischaemic factor during bile duct lamina remodelling3, which is an embryonic structure generated by the development of the distal ducts2.
As mentioned above, it is usually asymptomatic, although it can sometimes be associated with episodes of pain in the right hypochondrium, as well as bloating and a sensation of abdominal mass2.
It is not usually associated with analytical abnormalities2 and radiologically it is very similar to malignant lesions, such as liver metastases4, making differential diagnosis by imaging tests alone difficult. MRI-cholangiography is probably the most important imaging test in establishing the differential diagnosis3.
Radiological features include a honeycomb appearance and the presence of normal liver parenchyma intermingled within the nodular lesion, usually in the peripheral portion of the lesion5. It can be differentiated from biliary cystadenoma by its shape, as multicystic hamartoma has a honeycomb-like appearance and the cysts are relatively uniform in size, although they may vary if haemorrhage occurs, whereas this does not occur in cystadenoma or biliary cystadenocarcinoma5.
The definitive diagnosis is established by biopsy, which should be taken by wedge or core needle biopsy2, as fine needle aspiration biopsy is usually nondiagnostic and leaves more uncertainty6.
Macroscopically, there are superficial, subcapsular nodulations, .1 to .5 cm in diameter, with no proven lobar predilection, although there are cases that suggest that there may be a greater frequency in the right lobe7.
It is a lesion that is usually located around the hepatic capsule, near the fissure of the falciform ligament, protruding from the liver. It is usually composed of ductal structures, periductal glands and fibrous connective tissue, which contain biliary material in these structures8.
It is treated conservatively, although it is usually operated due to diagnostic uncertainty, and cases of cholangiocarcinoma have been reported almost anecdotally2.
AuthorshipVictoria Carmona: drafting of the article; critical review and approval of the final review.
Iago Justo: data collection and acquisition; critical review and approval of the final review.
Yolanda Rodríguez-Gil: data collection and acquisition.
Alberto Marcacuzco: critical review and image selection.
Carmelo Loinaz: approval of final review.
Carlos Jiménez: critical review and approval of final review.
Conflict of interestsThe authors have no conflict of interests to declare.