Mesenteric venous thrombosis (MVT) is a rare and insidious but potentially fatal form of mesenteric ischemia because its symptoms overlap with those of other diseases, delaying its diagnosis and treatment.1,2
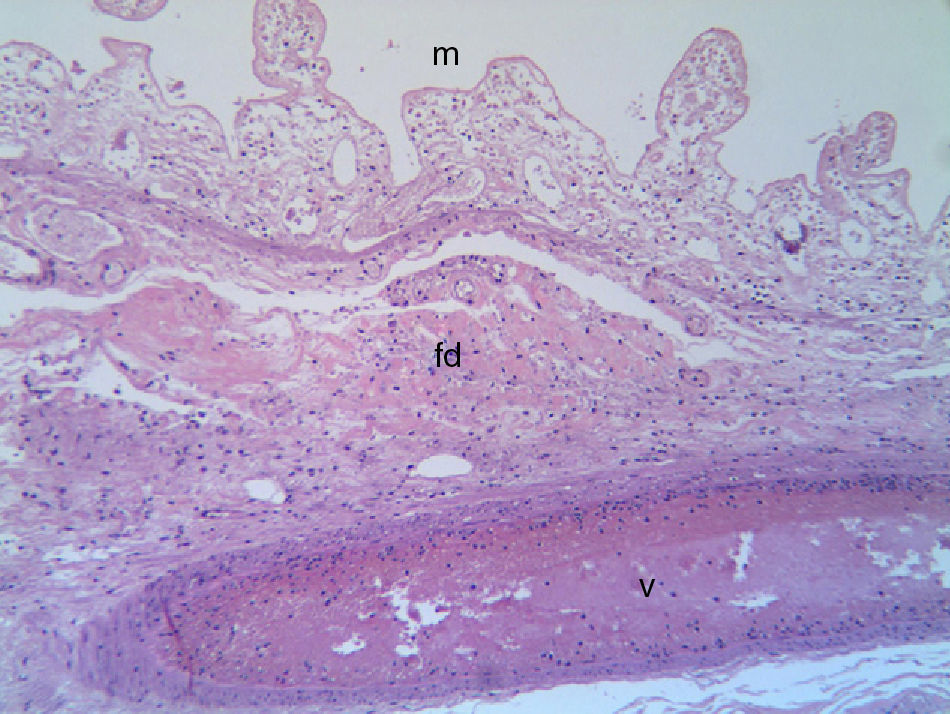
We present the case of a 64-year-old woman with a history of arterial hypertension and anxiety-depressive disorder that came to our Emergency Department due to abdominal pain and vomiting of 2 weeks duration. On physical examination, the patient was in a comatose state, with hypotension, anuria, notable dehydration and diffuse abdominal pain with distension and guarding. Blood tests showed moderate leukocytosis, hemoglobin 16.8g/dL, hematocrit 50.2%, glucose 270mg/dL, urea 315mg/dL, creatinine 10.8mg/dL, normal ionogram, pH 7.0, bicarbonate 9.2mmol/L, base excess 19.3mmol/L. Abdominal ultrasound and CT without contrast showed dilation of intestinal loops and the gastric chamber, a calcified aortic atheroma without involvement of the superior mesenteric artery, and images of intraluminal gas bubbles in an intestinal loop. We decided on hemodynamic and metabolic resuscitation prior to emergency laparotomy, during which an obstruction was found in the jejunum–ileal junction due to a solidified phytobezoar and areas of intestinal necrosis from the area of impaction up to the ileocecal valve. The ileum and ascending colon were resected and a manual jejunotransversostomy was performed. Histopathology reported transmural ischemic necrosis with associated mesenteric venous thrombosis (Fig. 1). In the immediate postoperative period, treatment with low molecular weight heparin was initiated with progressive recuperation from septic shock, and mechanical ventilation and vasoactive drugs were able to be withdrawn. The thrombophilia study found a slight elevation in homocysteine (23.4μM/L) and coagulation factor viii (194.6%). After 3 years of follow-up, the patient is asymptomatic and in treatment with acetylsalicylic acid (100mg/day).
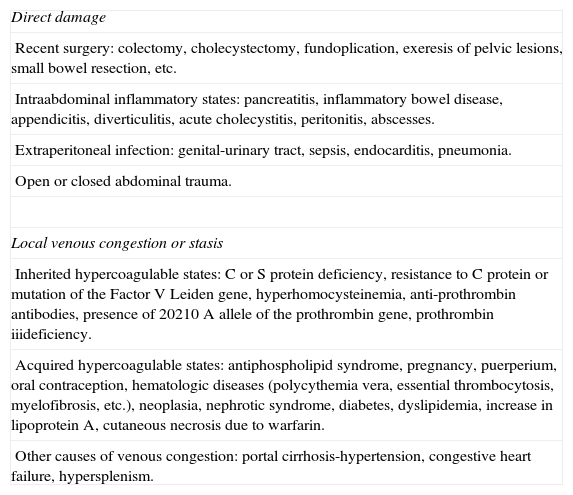
The mechanism and natural history of MVT are not clear, but there are risk factors in 75%–100% of patients,2–4 the most important of which are family and personal history of deep vein thrombosis1,3,5–7 and MVT. Associated risk factors are shown in Table 1. In our case, the causal factor was intestinal obstruction due to a bezoar that compressed the intestinal wall causing mesenteric venous congestion starting at the obstruction site (an association not found in the literature) together with mild increase in homocysteine and coagulation factor viii. Approximately half of patients present 2 or more risk factors, suggesting that the thrombosis is the result of multiple factors that interact.6,8
Risk Factors for Mesenteric Venous Thrombosis.
| Direct damage |
| Recent surgery: colectomy, cholecystectomy, fundoplication, exeresis of pelvic lesions, small bowel resection, etc. |
| Intraabdominal inflammatory states: pancreatitis, inflammatory bowel disease, appendicitis, diverticulitis, acute cholecystitis, peritonitis, abscesses. |
| Extraperitoneal infection: genital-urinary tract, sepsis, endocarditis, pneumonia. |
| Open or closed abdominal trauma. |
| Local venous congestion or stasis |
| Inherited hypercoagulable states: C or S protein deficiency, resistance to C protein or mutation of the Factor V Leiden gene, hyperhomocysteinemia, anti-prothrombin antibodies, presence of 20210 A allele of the prothrombin gene, prothrombin iiideficiency. |
| Acquired hypercoagulable states: antiphospholipid syndrome, pregnancy, puerperium, oral contraception, hematologic diseases (polycythemia vera, essential thrombocytosis, myelofibrosis, etc.), neoplasia, nephrotic syndrome, diabetes, dyslipidemia, increase in lipoprotein A, cutaneous necrosis due to warfarin. |
| Other causes of venous congestion: portal cirrhosis-hypertension, congestive heart failure, hypersplenism. |
MVT should be suspected in patients with acute abdominal and general symptoms (abdominal pain, nausea, vomiting, diarrhea, gastrointestinal bleeding, fever, clinical deterioration, anorexia)2–6 with previous episodes of thrombosis, coagulopathies, recent surgery or other associated factors1–8 (Table 1). Physical examination is of little use until the patient develops peritonitis or gastrointestinal bleeding that suggest the presence of mesenteric ischemia.7 The preoperative diagnosis is based on clinical suspicion and on CT findings with contrast, which is the radiological test with the greatest sensitivity (79%–100%).3–9 The most specific finding is dilation of the thrombotic vein with a central area of low attenuation that represents the intraluminal thrombus.6–8 In addition, intestinal viability is assessed, which provides for better selection of patients who are candidates for conservative treatment, and other diseases are ruled out.6,7 Phytobezoars are observed as ovoid or round masses with gas bubbles.10 Laparoscopy can be performed early on in the diagnostic-therapeutic algorithm of MVT because it facilitates the diagnosis of intestinal infarction and reduces unnecessary laparotomies in uncertain cases.9 In our case, we did not perform laparoscopy due to the poor general condition of the patient.
The primary aim of treatment is to prevent or limit intestinal gangrene and should be individualized according to the severity of the symptoms.5,6 It should be initiated with hydration, anticoagulation, nasogastric decompression, wide-spectrum antibiotics and, if indicated, thrombolysis and/or early surgical intervention.1,5,8,9 Before thrombolytic treatment, the diagnosis of MVT should be certain, the patient should be clinically stable with no evidence of intestinal perforation or infarction, and there should be no contraindication for its administration.2
Surgery is indicated by the presence of signs of peritonitis, hemodynamic instability or absence of diagnosis in patients with worsening abdominal symptoms.1,3,5,9 The procedure involves: (a) limited intestinal resection with liberal second-look laparotomy; (b) not performing thrombectomy unless it is proximal in the SMV and recent (<3 days), since most patients with acute MVT have diffuse MVT with distal extension, not appropriate for venous thrombectomy; and (c) in cases of extensive ischemic compromise, no resection should be done.1,3,5,6
Factors that seem to alter early survival are early diagnosis and anticoagulation,3,6 associated diseases and patient age.1,6 The relapse rate is high; thus, when a hereditary hypercoagulable state is detected, prolonged systemic anticoagulation should be maintained, while in other pro-thrombotic conditions 6 months of treatment provide adequate coverage.3,6
In summary, in patients with abdominal pain that has developed over several days or weeks with no demonstrated cause, MVT should be considered since early treatment can avoid mesenteric ischemia or a fatal outcome.
Please cite this article as: Del Rey-Moreno A, Jiménez-Martín JJ, Doblas-Fernández J, Marín-Moya R, García-Hirchsfield J. Trombosis venosa mesentérica asociada a obstrucción intestinal por fitobezoar. Cir Esp. 2013;91:461–463.