Pheochromocytomas and paragangliomas (PGL) are rare neuroendocrine tumors. 53% of paragangliomas are located in the organ of Zuckerkandl, situated in the distal abdominal aorta, between the inferior mesenteric artery and the aortic bifurcation.1 Most sympathetic paragangliomas and pheochromocytomas are catecholamine-secreting tumors, so determining plasma and/urine levels is the initial study used in these patients.2 After confirming the diagnosis, the initial imaging study should be computed tomography (CT), which can determine the tumor location in most cases. In cases of suspected paragangliomas that are not detected on CT, nuclear medicine studies can be used. Metaiodobenzylguanidine (MIBG) is an analog of guanidine, which is similar to noradrenalin. When used in clinical practice and radio-labeled with 123I, it accumulates in the adrenergic cells present in pheochromocytomas and paragangliomas. Used in conjunction with CT, this technique provides exact tumor localization and is an essential tool in difficult-to-diagnose tumors.3 Treatment for paragangliomas of the organ of Zuckerkandl is surgical resection, although occasionally exact identification of the location of these lesions is complex, so the use of a gamma probe could be a useful tool during surgery as it is more precise than ultrasound.
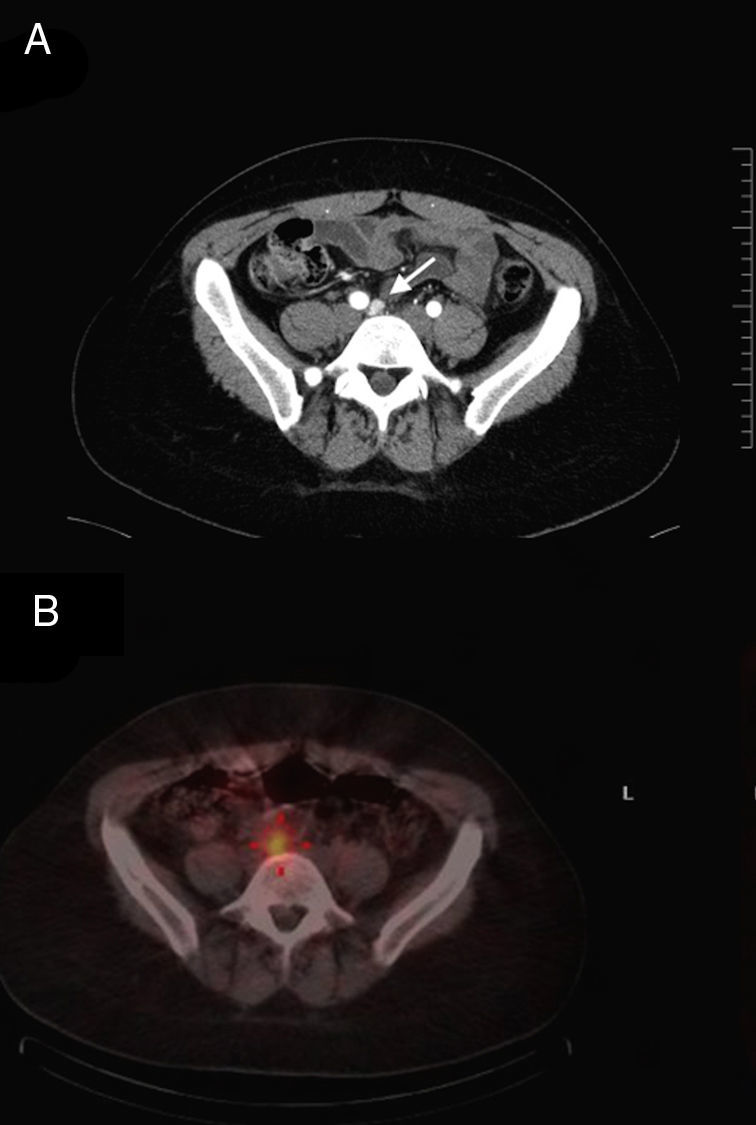
We present the case of a 33-year-old female patient with a 2-year medical history of recurring episodes of sweating and tachycardia. Physical examination demonstrated high blood pressure. The initial finding in the hypertension study was positive metanephrines in urine. The complementary study confirmed a 5cm mass located in the left para-aortic region under the inferior mesenteric artery. For preoperative preparation, alpha and beta blockers were used to achieve optimal blood pressure. Afterwards, the patient underwent laparoscopic resection of the tumor, with no complications. The histopathologic study confirmed a paraganglioma with no signs of malignancy, and metanephrine levels in urine after surgery were normal. Four months later, the patient's arterial hypertension persisted in spite of using alpha-1 adrenergic blockers (doxazosin). Abdominopelvic CT showed a lesion measuring 1.2cm immediately below the aortic bifurcation that had not been identified in previous studies (Fig. 1A). To complete the study, scintigraphy was conducted with 123I-MIBG, which confirmed a paraganglioma in the iliac region. The day prior to surgery, a 123I-MIBG SPECT/CT was done, and the SPECT images were merged with the CT scans to improve spatial localization and provide better anatomical correlation (Fig. 1B).
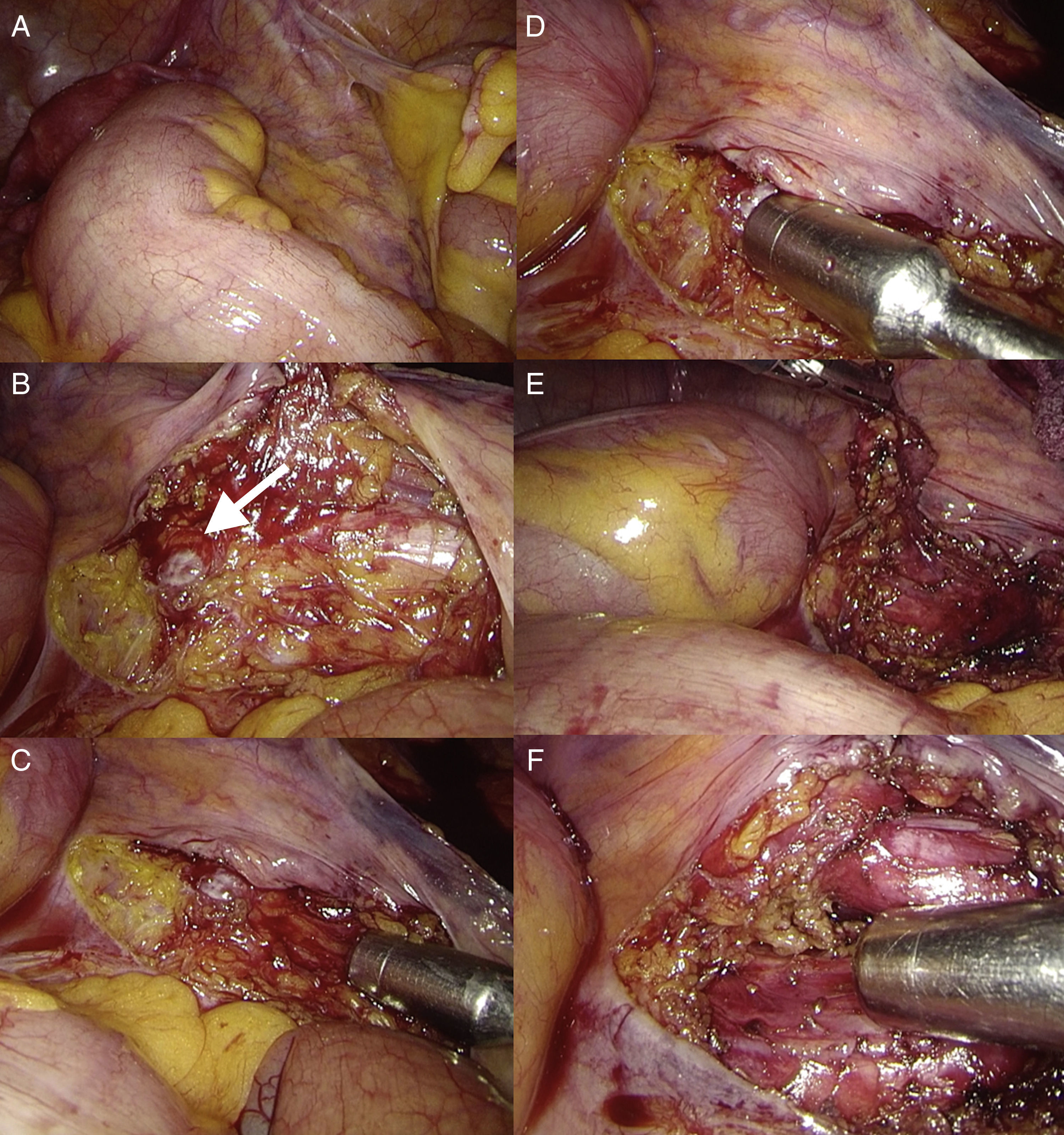
The patient underwent another laparoscopic resection 20h after the injection of 123I-MIBG (Fig. 2A). After dissection of the right iliac vessels (Fig. 2B), the lesion could not be identified with certainty. Given this circumstance, a sterile gamma probe was used to determine the exact location of the tumor (1.2cm). The probe showed an uptake of 78 counts per second (cps) in the suspected lesion, compared with the surrounding tissue at a normal uptake of 28cps (Fig. 2C and D). After confirmation, resection was performed, and there were no perioperative complications (Fig. 2E). Before concluding the surgical intervention, another gamma probe study was completed, which showed no evidence of other tissue with high 123I-MIBG uptake (Fig. 2F). The hospital stay was 3 days, and in the short-term evaluation no new episodes of hypertension have been detected. The biopsy study reported the same histology as the first resection, and postoperative hormone tests have been normal.
Laparoscopic image of the right iliac vessels (A) and uncertain identification of the lesion after dissection (B); gamma probe confirmed the pathologic uptake of the lesion compared with the surrounding tissue (C and D). Complete resection of the tumor was achieved (E). The gamma probe was used for the confirmation of the complete resection, with no evidence of uptake in the surrounding tissue (F).
Paragangliomas are uncommon tumors with an incidence of 0.1% in the general population.4 High diagnostic suspicion, therefore, is essential. After diagnostic confirmation with the measurement of catecholamines in plasma and/or urine, the location of the paraganglioma should be determined. Even though CT is able to locate the tumor, in most cases the use of 123I-MIBG fused with CT has been demonstrated to be more precise with greater specificity.5 This test could have been useful in the preoperative study of the first resection and could have provided early detection of the tumor in the organ of Zuckerkandl. Intraoperative localization by means of a portable gamma probe has been described in thyroid cancer and in neuroendocrine tumors, to mention a few.6,7 However, in the medical literature, there are only a few case reports of laparoscopic paraganglioma resection in the organ of Zuckerkandl,4,8 and even less frequent are those that also use a gamma probe to confirm the location of this type of tumors in order to guide surgery.9
Preoperative studies with radio-labeled MIBG, combined with the intraoperative use of a gamma probe, is safe, feasible and a valuable tool for surgeons in order to detect not just small paragangliomas but also pheochromocytomas and to achieve complete oncological resection of these lesions.
Please cite this article as: Navarrete A, Almenara R, Momblán D, Lacy A. Resección laparoscópica de paraganglioma en el órgano de Zuckerkandl guiado por sonda gamma con 123I-metayodobencilguanidina. Cir Esp. 2017;95:239–241.