Laparoscopic common bile duct exploration (LCBDE) is a reliable, reproducible and cost-effective treatment for common bile duct stones. Several techniques have been described for choledochotomy closure.
AimsTo present our experience and the lessons learned from more than 200 cases of LCBDE.
Patients and methodsBetween January 1999 and July 2012, 206 patients with common bile duct stones underwent LCBDE. At the beginning of the series, we performed the closure of the CBD over a T-tube (36 patients), subsequently we favoured closure over an antegrade stent (133 patients), but due to a high incidence of acute pancreatitis in the last 16 patients we have performed primary closure.
ResultsThe 3 closure groups were matched for age and sex. Jaundice was the most frequent presentation. A total of 185 (88.5%) patients underwent choledochotomy, whereas in 17 (8.7%) patients the transcystic route was used. The group that underwent choledochotomy had a larger size of stones compared to the transcystic group (9.7 vs 7.6mm). In the stented group we found an 11.6% incidence of pancreatitis and a 26.1% incidence of hyperamylasemia. In the primary closure group we found a clear improvement of complications and hospital stay. The increased experience of the surgeon and age (younger than 75) had a positive impact on mortality and morbidity.
ConclusionsPrimary closure of the common bile duct after LCBDE seems to be superior to closure over a T tube and stents. The learning curve seems to have a positive impact on the outcomes, making it a safe and reproducible technique especially for patients aged under 75 years.
El abordaje laparoscópico de la vía biliar (ALVB) es una técnica segura, reproducible y coste-efectiva para el tratamiento de la coledocolitiasis frente a la cirugía abierta. Tras la realización de la coledocotomía han sido propuestas diversas técnicas para el cierre de la vía biliar principal (VBP).
ObjetivoPresentar nuestra experiencia en el ALVB como técnica rutinaria en el tratamiento de la coledocolitiasis y las lecciones aprendidas tras más de 200 casos.
Pacientes y métodosEntre enero de 1999 y julio de 2012 se realizó el ALVB en 206 pacientes con el diagnóstico de coledocolitiasis. En los inicios de la serie realizamos el cierre de la vía biliar (VB) mediante tubo de Kehr, posteriormente la técnica de elección fue la colocación de un stent anterógrado, pero dada la elevada incidencia de pancreatitis aguda (PA), en los últimos pacientes de la serie realizamos un cierre primario de la VBP sin drenaje de la misma.
ResultadosLos grupos fueron homogéneos en cuanto a edad y sexo. La presentación clínica más frecuente fue la ictericia. En 185 pacientes (88,5%) se realizó un abordaje quirúrgico mediante coledocotomía y en 17 pacientes (8,7%), transcístico. En los pacientes a los que se realizó coledocotomía, el tamaño medio de las litiasis fue mayor (9,7 vs 7,6mm en el abordaje transcístico). Tras la coledocotomía colocamos un tubo de Kehr para el cierre de la VBP en 36 pacientes, en 133 se colocó un stent anterógrado observando un 11,6% de PA y un 26,1% de hiperamilasemia, por lo que en los últimos pacientes de la serie (16) hemos realizado un cierre primario de la VBP sin drenaje, mejorando la morbilidad y la estancia hospitalaria. Se observó una disminución de la morbimortalidad en pacientes menores de 75 años y en el grupo de pacientes en los que existía una mayor experiencia por parte del cirujano.
ConclusionesTras la realización del ALVB en el tratamiento de la coledocolitiasis, un cierre primario de la VB sin drenaje de la misma presenta ventajas sobre otras técnicas más clásicas como la colocación de un tubo de Kehr o el stent. Es importante una adecuada curva de aprendizaje para mejorar los resultados en el manejo laparoscópico de esta enfermedad. El ALVB es una técnica segura y reproducible, especialmente en pacientes menores de 75 años.
Numerous prospective studies conclude that laparoscopic common bile duct exploration (LCBDE) is a safe, reproducible and cost-effective treatment for common bile duct stones compared with 2-stage treatment of choledocholithiasis (endoscopic retrograde cholangiopancreatography (ERCP) followed by laparoscopic cholecystectomy). Lithiasis extraction may be performed by a trancystic or choledochotomy approach.
Several techniques have been described for primary common bile duct closure (PCBDC) following choledochotomy. Closure over a T-tube is a technique with up to 15% complications, comparable figures to open surgery. A viable alternative to reduce complications from T-tube is the laparoscopic placement of an antegrade stent, followed by bile duct closure. However, this technique also presents a high rate of complications according to several series, including the development of acute postoperative pancreatitis (AP). Recently, primary bile duct closure during surgery following intraoperative cholangiography (IOC) has been proposed as a safe, reproducible technique with fewer complications than the previous procedures, where internal or external common bile duct drainage was performed.
In this retrospective study we describe and compare the postoperative results in a large series of patients who underwent LCBDE. At the beginning of the series, we performed common bile duct closure using a T-tube and later the technique of choice was placement of an antegrade stent, but due to the high incidence of AP we performed primary closure of the BD without drainage in the last patients of the series.
Material and MethodsBetween January 1999 and July 2012, LCBDE was performed on 206 patients diagnosed with choledocholithiasis in the senior author's department (AMI). 142 of the patients were women and 64 were men, with a median age of 57.2 (13–91) years. Data were collected prospectively and analysed retrospectively. All the patients underwent standard cholecystectomy during the same surgical procedure, except for 3 patients who had previously undergone cholecystectomy (one laparoscopic and 2 via conventional open approach).
Surgical TechniqueFor the surgical technique we placed trocars using the French technique with an extra 5mm port in the right hypochrondrium (RHC) over the common bile duct. Initially, standard cholecystectomy was performed generally using CIO (Horner needle). When the transcystic approach is used, the cystic duct is tightened with an Endoloop® (Ethicon Company, New Brunswick, Nueva Jersey, U.S.A.), externalised at RHC level with an Endoclose® (Covidien, Mansfield, Massachusetts, U.S.A.). For choledochotomy, we opened the common bile duct with laparoscopic scissors, except in the cases of severe cholangitis where pure cutting mode diathermy was used.
Subsequent to the completion of the cholecystectomy, we inserted a Nathanson divider through the epigastric trocar and through the 5mm port at the RHC, and also a choledochoscope which would function either through the choledochotomy or the cystic duct, depending on the chosen technique. We extracted the stones with a Dormia basket, and following this, a proximal and distal control choledochoscopy was performed.
In the first part of the study, following decompression of the common bile duct, we inserted a T-tube for drainage (n=36). The surgical technique used was similar to the conventional open approach. Ten days after choledochotomy, cholangiography was performed via the T-tube, and the T-tube was removed after 4 weeks when a good passage of contrast medium into the duodenum with no leakage was observed.
From June 2001, the procedure of choice was the insertion of an antegrade biliary stent, using direct vision (10fr×7cm Amsterdam type stent), followed by a PCBDC (n=133). Stent removal was generally performed after 2 weeks using upper digestive tract endoscopy in the outpatient unit.
A combined technique was used on 2 patients with a false tract (insertion of an endoprosthesis and a T-tube) and in another 2 patients it was necessary to perform laparoscopic biliary anastomosis (one choledochoduodenostomy and one choledochoenterostomy).
Transcystic approach for lithiasis removal with closure by ligation was performed on 17 patients.
From November 2011 (n=16), the technique of choice was primary choledochotomy closure after decompression of the PCBDC, with continuous suture (Vicryl 5/0, Ethicon, Johnson and Johnson Company, Edinburgh, United Kingdom), after confirming PCBDC permeability by IOC or choledochscopy.
Surgery was completed with the placement of a Robinson drain which was removed 24h after surgery, except in transcystic exploration cases which were generally completed without drainage.
Amylase testing was carried out in all patients 24h after surgery. When amylase levels were high (3 times the normal value) combined with the presence of symptoms, AP was diagnosed. In those cases with severe criteria according to the Glasgow scale, an abdominal CT scan was performed and the patients were transferred to the ICU.
The development of postoperative AP was classified as a major complication, and postoperative hyperamylasaemia without pancreatitis was classified as a minor complication.
When the presence of bile in a drainage bag was detected the patients were classified as having biliary fistula.
Statistical AnalysisThe epidemiological characteristics, intraoperative findings and postoperative results of all patients were analysed. The statistical differences between the different groups were determined using the Student t-test. P<.05 was considered statistically significant. The statistical programme SPSS Spanish version 10.0 20 was used for the analysis.
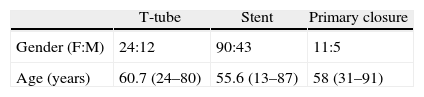
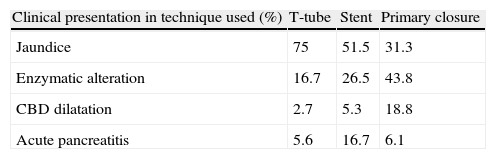
ResultsWhen analysing the characteristics of the patients included in this study, we found that there was a predominance of women in the 3 groups, with a comparable mean age (Table 1). The most frequent clinical presentation was jaundice, followed by liver enzyme alteration (Table 2).
The choledochotomy approach was used in 185 patients (88.5%) and transcystic approach in 17. At the beginning of the series 2 patients needed duodenotomy and open sphincteroplasty and 2 patients underwent laparoscopic biliary bypass (choledochoduodenostomy and choledochoenterostomy). Median stone size was 0–28mm and the mean diameter of PCBDC was 12mm (7–23mm). The mean size of the lithiasis in the transcystic approach was 7.6mm (3–20mm), whilst with the choledochotomy approach it was 9.7mm (2–30mm). The choledochotomy approach was justified due to the greater size of the lithiasis in these patients.
25.3% of patients in the series (n=52) underwent surgery after failed ERCP (20% from failure in extraction after cannulation and 5.3% from failure in cannulation). In patients under 75 years (n=160) ERCP failed in 31 of them (19.3%), 3.7% due to failure in cannulation and 15.6% from failure in extraction after cannulation. In patients over 75 years (n=46) ERCP failed in up to 45.6%, 13% due to failure in cannulation and the remaining 32.6% from failure in extraction after cannulation, which justified surgery.
Of the 206 patients who underwent surgery, laparoscopic extraction could not be completed in 11 (5.3%) cases; conversion to open surgery was performed in 4 patients (1.9%); disimpaction of the stone was carried out in one, assisted by hand, and the other 6 patients were referred for postoperative ERCP after draining of the common bile duct with a T-tube (n=2) or stent (n=4). The most frequent cause of failure was the impaction of distal stones. Of these 11 patients for whom the laparoscopic procedure was not completed, 8 belonged to the first 100 and 3 to the following 106 patients, with the importance of the experience of the surgeon being significantly reflected (P=.02). Conversion to open surgery from case 100 upwards was 0%.
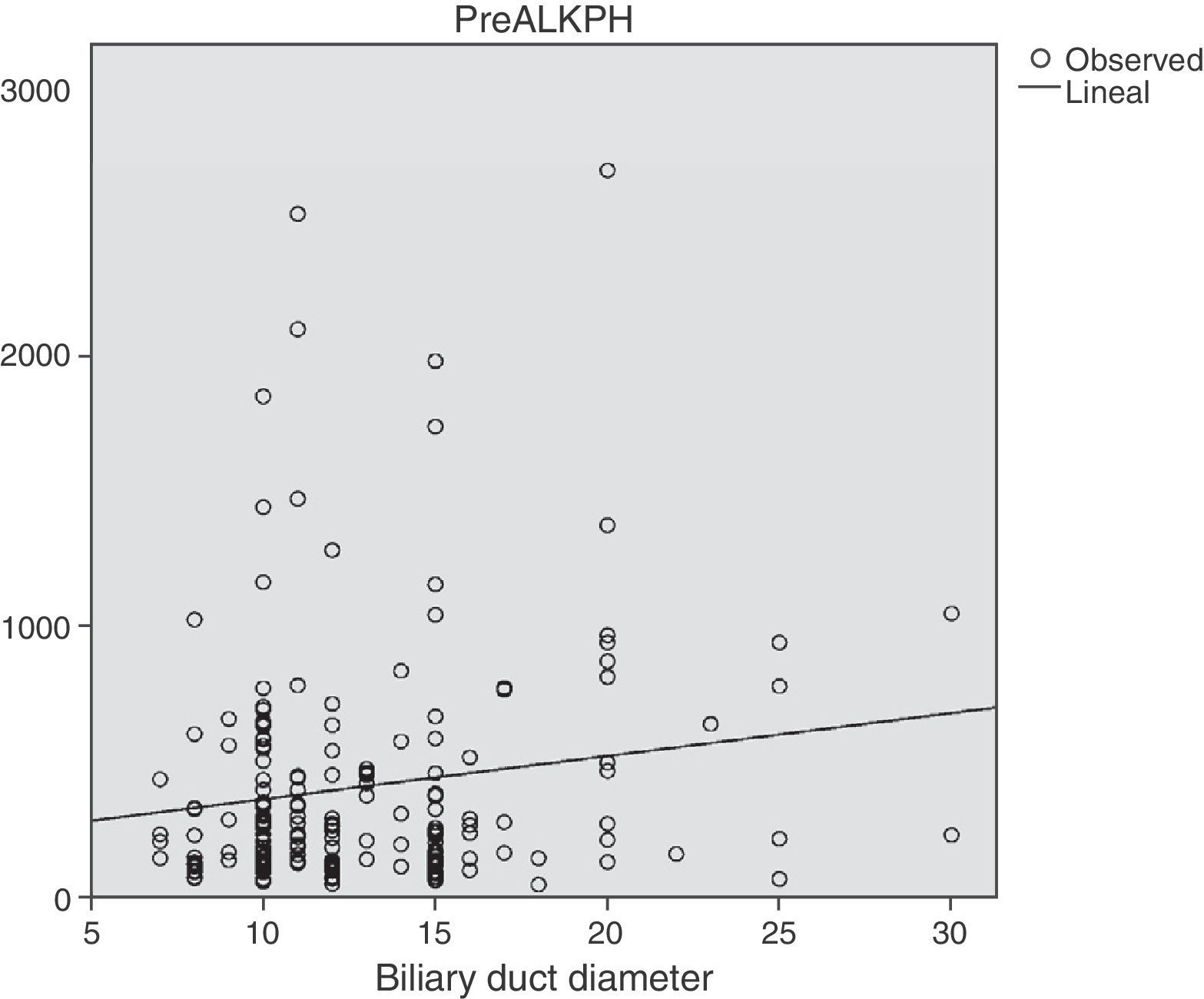
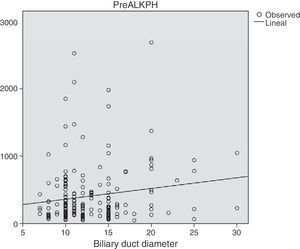
Analysis of the relationship of the bile duct size with preoperative analytical parameters, showed that patients with high levels of alkaline phosphatase had significantly greater dilatation of the bile duct (P=.04). No correlation between the Br and preoperative amylase figures and the bile duct diameter was found (Fig. 1).
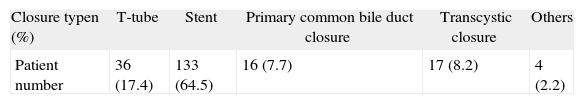
Common bile duct closure is shown in Table 3; at the beginning of the series most of the closures included the placement of T-tubes and primary closure at present.
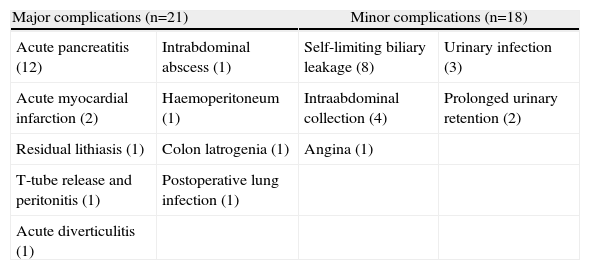
The total number of major complications following surgery was 10.5% (n=21), most of them AP, and 9% minor complications (n=18) were mainly postoperative biliary leakage which did not require reintervention (Table 4). Three patients died after surgery (1.5%), one of them due to acute complicated diverticulitis during the post-operative period and the other 2 from postoperative acute myocardial infarction; all three patients were aged over 75 years, 2 belonged to the first group (first 100 patients) and one to the last group (n=106). In 2 of the 3 patients who died, surgery was justified by the impossibility of completing ERCP. There was no mortality in patients aged under 75 years in our series.
Description of Postoperative Complications.
| Major complications (n=21) | Minor complications (n=18) | ||
| Acute pancreatitis (12) | Intrabdominal abscess (1) | Self-limiting biliary leakage (8) | Urinary infection (3) |
| Acute myocardial infarction (2) | Haemoperitoneum (1) | Intraabdominal collection (4) | Prolonged urinary retention (2) |
| Residual lithiasis (1) | Colon latrogenia (1) | Angina (1) | |
| T-tube release and peritonitis (1) | Postoperative lung infection (1) | ||
| Acute diverticulitis (1) | |||
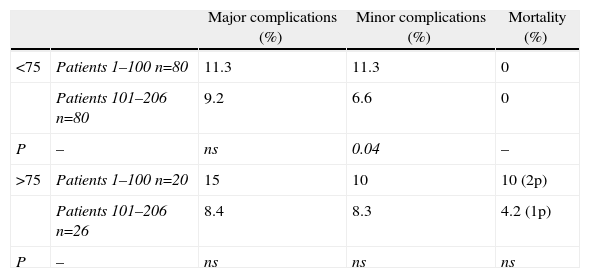
After case 100 a reduction in postoperative morbidity was observed, when the technique was perfected and the surgeon had more experience, in both major (P=ns) and minor (P=.04) complications. We also observed differences in morbidity by age group, the rate of major (P=ns) and minor (P=.04) complications being lower in younger patients (aged under 75 years) (Table 5).
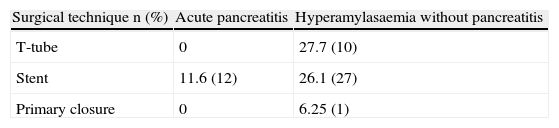
The global incidence of AP was 6% (12 patients). Our analysis of the incidence of AP and hyperamylasaemia according to the surgical technique used revealed that patients for whom a stent had been placed as the technique of choice presented a higher rate of AP compared with that in the other surgical techniques; this was statistically significant (P=.001) (Table 6). There was no relationship between the surgeon's experience and the rate of AP.
A stent was inserted in 29 patients after having previously performed an ERCP. The AP rate in them was 3.4% (only one patient) and that of hyperamylasaemia was 10.3% (3 patients), which would suggest that the patients who had previously undergone an ERCP with sphincterotomy had a significantly lower rate of AP and hyperamylasaemia than those without ERCP (P=.03).
Analysis of the relationship between preoperative Br figures and postoperative complications, showed that high Br counts prior to surgery did not lead to an increase in AP complications or longer postoperative hospital stay, even in patients with preoperative Br greater than 100 (unit), P>.05.
The overall mean hospital stay in our series was 6.22 days (1–81 days). Patients with a longer hospital stay (14.3 days) were those who had had a T-tube placed during surgery. The series of patients with stents had a postoperative stay of 6.2 days (1–30 days). A significant reduction in hospital stay was observed for those patients who underwent primary closure of the biliary duct (P<.05), their stay was 3.5 days (1–12 days).
DiscussionThe laparoscopic approach for choledocholithiasis has been demonstrated as a valid, safe alternative with fewer complications and shorter hospital stay than open surgery and is currently the technique of choice in the treatment of this disease.1,2
Several prospective studies have shown that LCBDE in a single surgical stage is a safe and more cost-effective surgical technique than 2-stage treatment (ERCP followed by cholecystectomy) in the treatment of choledocholithiasis, reducing the number of procedures, health costs and hospital stay of the patient.3–7 LCBDE may be carried out using the transcystic or choledochotomy approach, depending on the indication.8
LCBDE is the choice for patients with gastric bypass with choledocholithiasis due to the total impossibility of access with ERCP, which occurred in one of our patients.
For many years, insertion of the T-tube was the technique of choice for decompression of PCBDC following choledochotomy. However, this technique led to a high level of complications ranging between 6% and 30%, according to different studies,8,9 the figures obtained being similar to results obtained in open surgery. The most frequent complication with this technique is biliary leakage.10,11 Another inherent disadvantage to this technique is the need for the patient to have a drainage tube for several weeks, causing pain in the surrounding area. Quality of life is compromised and there is a delay in their return to work.
Later, the use of an antegrade biliary stent, following choledochotomy, became a valid alternative to the T-tube. Numerous studies showed that the insertion of a stent for CBD drainage after surgery led to a shorter hospital stay compared with that using the T-tube, and a faster return of the patient to their normal routine. The number of postoperative complications such as biliary leakages or duodenal erosions also dropped.9,12–16 In our series, we chose to use a stent for CBD drainage in 132 patients (66%) and observed a high rate of AP (11.6%) and hyperamylasaemia without pancreatitis (26.1%), which made us reconsider its use, although there were no cases of AP in patients in the earlier series in whom we had placed a T-tube as a drainage system. Several studies which use stents as an internal CBD biliary drainage technique show AP rates from 3% to 12%.8,16
We observed that patients who had an ERCP and sphincterotomy prior to placement of the stent (n=29) presented significantly lower incidence of AP and hyperamylasaemia, thus highlighting the protective effect of the sphincterotomy in these patients.
Due to the high AP rate we decided to abandon using stents as the technique of choice for biliary drainage after LCBDE, performing primary closure of the CBD in the last patients of our series, after verifying intraoperatively by cholangiography or choledochoscopy the absence of residual lithiasis and the good passage of contrast medium through the CBD or an open sphincter. Randomised prospective studies define this as the technique of choice for the treatment of choledocholithiasis,11,17,18 demonstrating that primary closure of the CBD is a safe technique and has fewer complications compared to the use of stents or the placement of a T-tube. A recent meta-analysis of 956 patients11 compares a group of patients who underwent CBD drainage and a second group without drainage after a LCBDE for choledocholithiasis, demonstrating that the group with drainage (T-tube) presented a greater amount of postoperative complications, and therefore concludes that the routine use of biliary drainage after surgery is not justified and is only reserved for selected cases. In our series we performed primary closure of PCBDC without drainage in 16 patients without encountering AP, or major or minor complications, and these patients presented a significantly shorter hospital stay compared with those who were given a stent or T-tube for CBD drainage. Therefore it appears that this technique is marking the future for the laparoscopic treatment of choledocholithiasis, although further prospective studies need to be conducted to support this current trend.
Several studies have analysed the risk factors which may affect unfavourable results after LCBDE.19,20 These authors conclude that the preoperative Br figures are a risk factor for the development of postoperative complications. In a recent study published by Noble et al.,21 age and anaesthetic risk (ASA) are defined as poor prognostic factors after surgery and high levels of preoperative Br are associated with higher rates of conversion to open surgery and a longer postoperative hospital stay. In our study, however, we dispute this idea showing that higher preoperative Br figures, even above 100μmol/l, do not lead to increased complications, to AP, conversion to open surgery or longer hospital stay, and therefore we believe this should not be a limiting factor when planning surgery.
When we analysed the influence of age on surgical results, we found higher rates of morbimortality in patients aged over 75 years, similar to other studies where a greater amount of complications is associated with advanced age.22 There was no mortality in our series in patients aged under 75 years, and therefore LCBDE is considered the technique of choice in these patients. We must be particularly careful with this surgery in patients aged over 75 years, respecting cases where it is contraindicated or there was a failure in performing ERCP or in those selected who present a low surgical risk.
Better results are also observed in the patient group with a more experienced surgeon, highlighting the importance of a correct learning curve and perfection of the technique aimed at obtaining better results with a lower rate of complications and conversion to open surgery. For this reason, we believe that the surgeons who are learning the current technique could benefit from the author's learning curve.
ConclusionLCBDE is the technique of choice in the treatment of choledocholithiasis compared with the 2-stage treatment approach. Among the techniques used, placement of a biliary drain after surgery, via either T-tube or stent, has disadvantages which include a high rate of biliary leakage, longer hospital stay and AP respectively, making primary closure of PCBDC without drainage the technique of choice in the treatment of this disease. A correct learning curve is important for improving results in the laparoscopic management of this disease; as this is a safe and reproducible technique, particularly in patients aged under 75 years.
Authors/co-authorsTwo of the co-authors of this study practice in the United Kingdom (London).
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Abellán Morcillo I, Qurashi K, Abrisqueta Carrión J, Martinez Isla A. Exploración laparoscópica de la vía biliar, lecciones aprendidas tras más de 200 casos. Cir Esp. 2014;92:341–347.