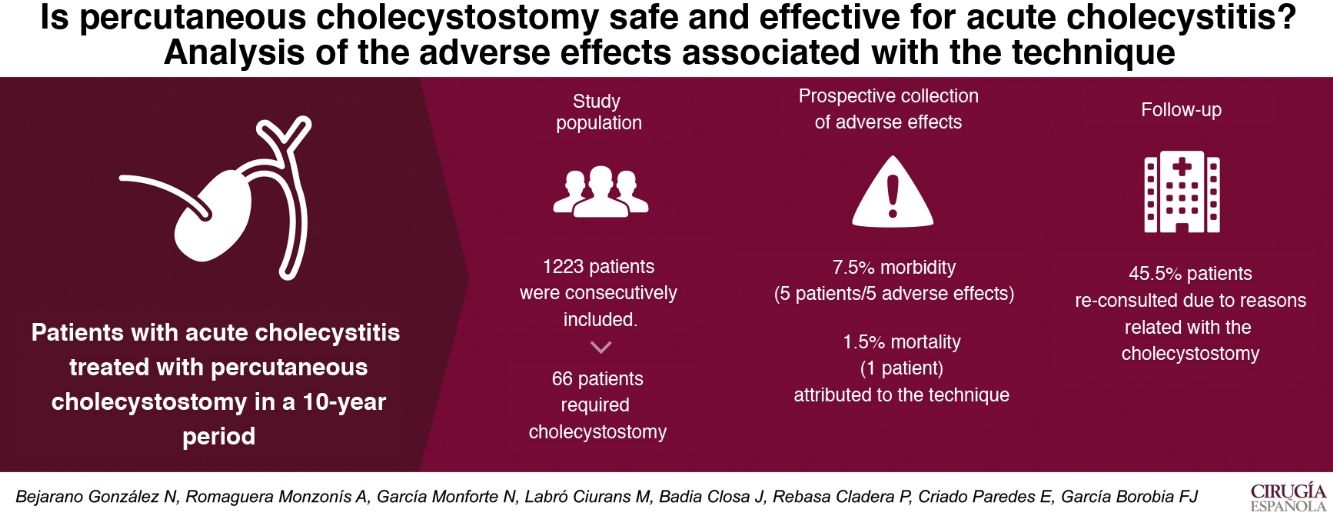
The main objective of our study is to assess the safety and efficacy of percutaneous cholecystostomy for the treatment of acute cholecystitis, determining the incidence of adverse effects in patients undergoing this procedure.
Material and methodObservational study with consecutive inclusion of all patients diagnosed with acute cholecystitis for 10 years. The main variable studied was morbidity (adverse effects) collected prospectively. Minimum one-year follow-up of patients undergoing percutaneous cholecystostomy.
ResultsOf 1223 patients admitted for acute cholecystitis, 66 patients required percutaneous cholecystostomy. 21% of these have presented some adverse effect, with a total of 22 adverse effects. Only 5 of these effects, presented by 5 patients (7.6%), could have been attributed to the gallbladder drainage itself. The mortality associated with the technique is 1.5%. After cholecystostomy, one third of the patients (22 patients) have undergone cholecystectomy. Urgent surgery was performed due to failure of percutaneous treatment in 2 patients, and delayed in another 2 patients due to recurrence of the inflammatory process. The rest of the cholecystectomized patients underwent scheduled surgery, and the procedure could be performed laparoscopically in 16 patients (72.7%).
ConclusionWe consider percutaneous cholecystostomy as a safe and effective technique because it is associated with a low incidence of morbidity and mortality, and it should be considered as a bridge or definitive alternative in those patients who do not receive urgent cholecystectomy after failure of conservative antibiotic treatment.
El objetivo principal de nuestro estudio es valorar la seguridad y eficacia de la colecistostomía percutánea para el tratamiento de la colecistitis aguda determinando la incidencia de efectos adversos que presentan los pacientes sometidos a este procedimiento.
Material y métodoEstudio observacional con inclusión consecutiva de todos los pacientes con diagnóstico de colecistitis aguda durante 10 años. La variable principal estudiada ha sido la morbilidad (efectos adversos) recogida de forma prospectiva. Seguimiento mínimo de un año de los pacientes sometidos a colecistostomía percutánea.
ResultadosDe 1223 pacientes ingresados por colecistitis aguda, 66 pacientes han precisado colecistostomía percutánea. El 21% de éstos ha presentado algún efecto adverso, con un total de 22 efectos adversos. Tan sólo 5 de estos efectos, presentados por 5 pacientes (7,6%), han podido ser atribuidos al propio drenaje vesicular. La mortalidad asociada a la técnica es del 1,5%. Tras la colecistostomía un tercio de los pacientes (22 pacientes) han sido sometidos a colecistectomía. Se ha realizado intervención quirúrgica urgente por fracaso del tratamiento percutáneo en 2 pacientes, y diferida en otros 2 pacientes por recidiva del proceso inflamatorio. El resto de los pacientes colecistectomizados han sido intervenidos de forma programada pudiéndose llevar a cabo el procedimiento de forma laparoscópica en 16 pacientes (72,7%).
ConclusiónConsideramos la colecistostomía percutánea como técnica segura y eficaz por relacionarse con una baja incidencia de morbilidad y mortalidad, debiéndose considerar como alternativa puente o definitiva en aquellos pacientes no tributarios de colecistectomía urgente tras fracaso del tratamiento conservador con antibiótico.
Cholecystectomy is the treatment of choice for acute cholecystitis (AC). Due to the aging of the population, the comorbidity or severity presented by patients and the need for general anesthesia for its performance, alternative treatments are occasionally necessary, provided that antibiotic therapy is not sufficient for the resolution of the inflammatory/infectious process.
Percutaneous drainage of the gallbladder or percutaneous cholecystostomy (PC) is being used in our hospitals as a resource technique when it is impossible or difficult to perform cholecystectomy in patients with high surgical risk who present AC.1,2 However, there is little evidence about associated morbidity as there are no published prospective studies that assesses the safety of this procedure.
The objective of our study is to assess the safety and efficacy of PC for the treatment of AC, while determining the incidence of adverse effects (AE) presented by patients who have undergone this procedure, based on a strict follow-up. The secondary objectives were to assess the results of the technique and the survival of patients in the medium term.
MethodsThis is an observational and descriptive study carried out in the general surgery service with a reference population of 430 000 inhabitants. The development of the study has not altered in any way the treatment of the patients included. This study was approved by the Clinical Research Ethics Committee of our hospital, and the ethical principles for human medical research were followed at all times in accordance with the Declaration of Helsinki.3
All patients admitted for AC from January 2008 to December 2017 were consecutively included in the study, using the internationally accepted diagnostic criteria of the Tokyo Clinical Guidelines.4–6
Treatment was indicated based on the severity of the AC episode and the baseline status of the patient, following international clinical guidelines,1,2,6–8 which is standard clinical practice in our hospital. PC was indicated in patients who were not candidates for urgent surgery and who showed poor progress with antibiotic treatment.
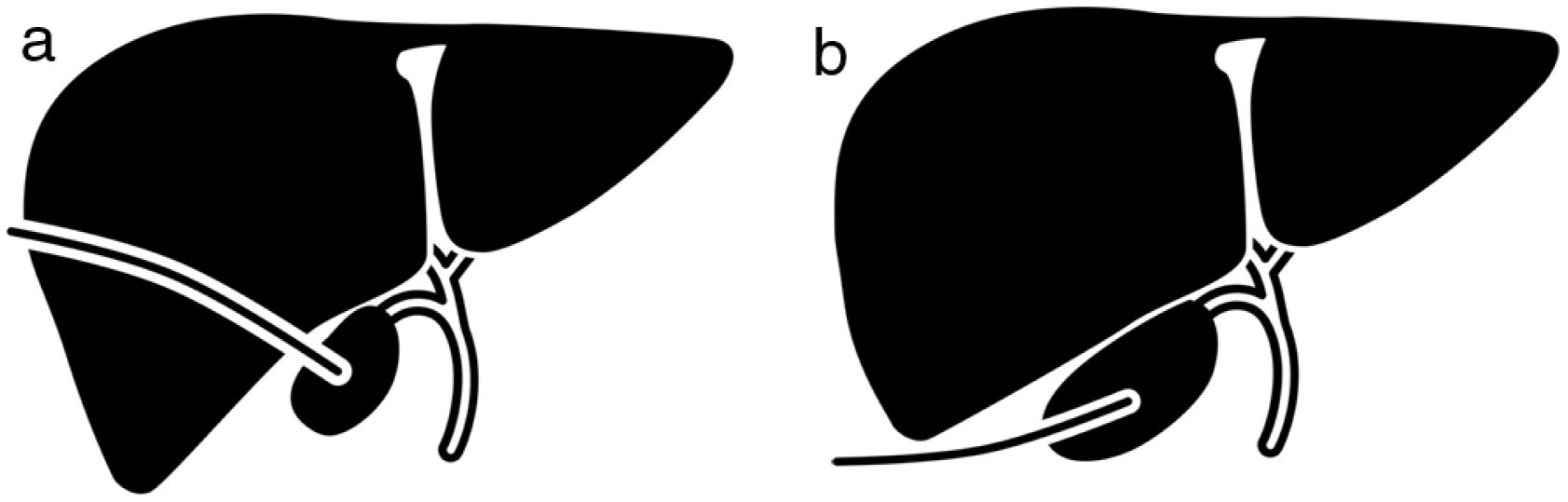
Percutaneous cholecystostomy technique and device controlGallbladder puncture for drainage was performed by the interventional vascular radiology team (available at our center 24 h/day), following the standard technique using ultrasound guidance and under local anesthesia. The percutaneous transhepatic or transperitoneal approach was used at the discretion of the operating radiologist, depending on the patient’s comorbidity and the existing ultrasound window (Fig. 1). The Seldinger technique was used, followed by the placement of a 10 Fr pigtail catheter with fluoroscopic guidance. Said drain tube was left at an angle for drainage and fixed to the skin with a hydrocolloid dressing (Hollister®). Once the acute infectious process had been resolved, the drain tube was checked by cholangiography as a scheduled procedure. The PC was closed when cystic duct patency was verified, and occupation or obstruction of the main bile duct was ruled out. The usual follow-up of patients with PC consisted of monthly replacement of the drainage fixation device and replacement of the pigtail itself every six months. Patients who underwent cholecystectomy continued with PC drainage until the catheter was removed in the operating room during the procedure.
Patients referred from other centers solely for PC placement were excluded from the study.
The data collection period encompassed the moment the patient was admitted to our service until December 2018 (minimum follow-up of one year). Spanish Organic Law 15/1999 from December 13 regarding the protection of personal data (LOPD) was complied with at all times.9 These data have been collected in Access® protected format.
The main variable studied was morbidity (AE). Each clinical situation that could be considered an AE was prospectively and thoroughly entered into the database on a daily basis by a single person. A reviewer not directly involved in patient management evaluated whether the event was an AE, the sequelae and the presence of error. AE was defined as an unexpected consequence or injury caused by patient treatment and not due to an underlying disease.10 To assess the associated damage and the degree of disability caused by each AE, the Brennan et al. scale was used,11 and, as of 2009, the Dindo-Clavien Classification was introduced.12
Other variables collected included age, sex, ASA classification, date of PC placement and removal, reason for indication, technique performed, monitoring and replacement of PC, date of cholecystectomy and type of surgery (elective/urgent), ICU stay, overall hospital stay, follow-up time, and mortality.
Statistical analysisThe SPSS®-25 IBM SPSS Statistics program (SPSS Inc, an IBM Company) was used to analyze the variables. In the descriptive analysis, the data are presented as mean and standard deviation in the case of continuous variables with normal distribution, median and interquartile range if the continuous variables do not follow the normal law, and as a percentage in the case of categorical variables. When extrapolations are made from the descriptive data to the general population, they are given with a 95% confidence interval.
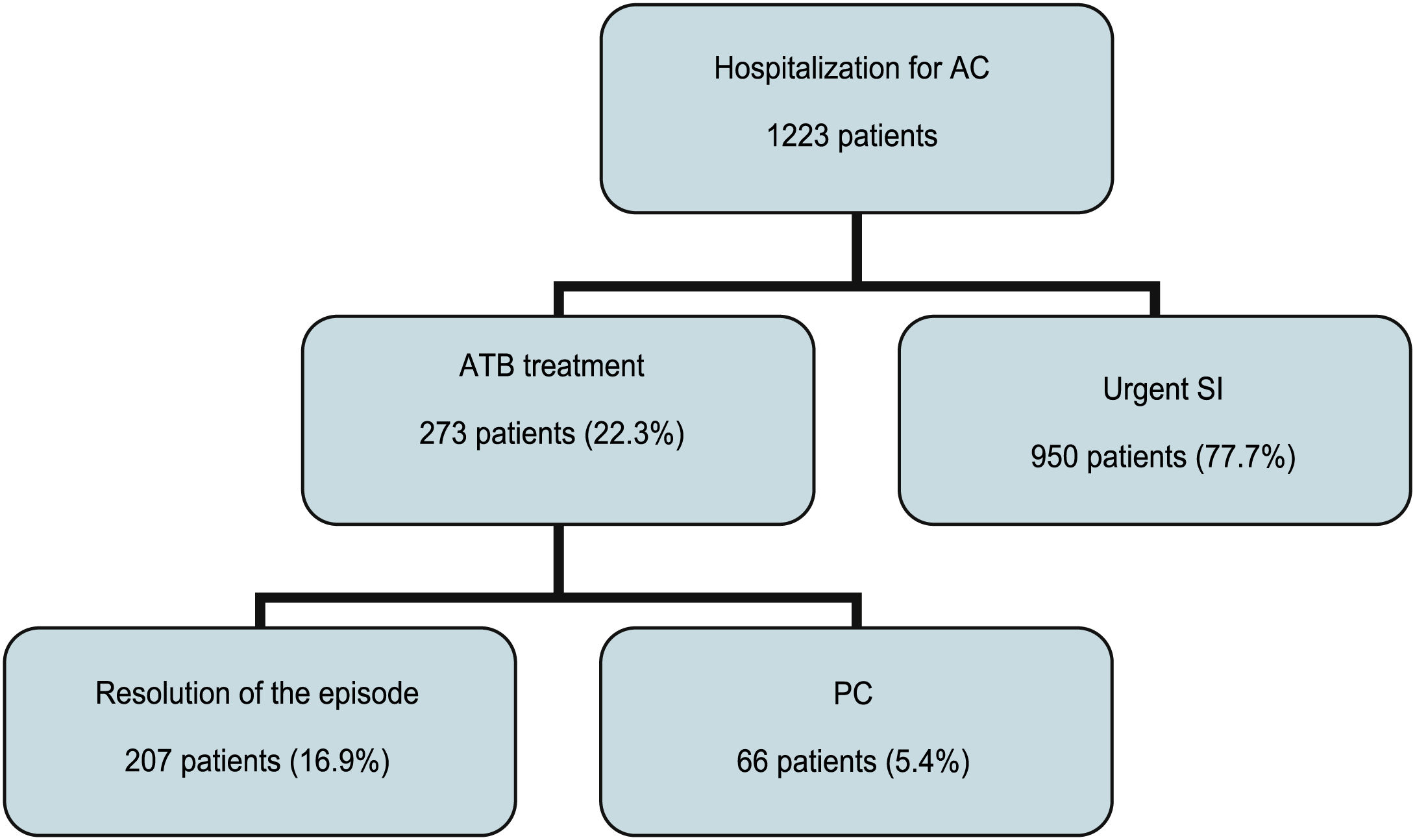
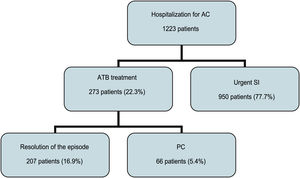
ResultsA total of 1223 admitted patients with a diagnosis of AC were included over the 10-year period of the study. Out of this total, 273 (22.3%) did not undergo urgent surgery during hospitalization for the acute episode due to high surgical risk (ASA III or higher), symptoms for more than 7 days, associated cholestasis that required a more complete study prior to surgery or refusal of the patient to undergo surgery. Among the patients who were not candidates for surgery during the emergency episode, 66 had a poor outcome despite being treated with antibiotics and required PC, which represented 5.4% of all patients admitted with this diagnosis to our unit (Fig. 2).
The mean age of the patients requiring PC was 79 years (SD ± 10 years), and 57.6% were male.
The distribution of patients according to the ASA classification was 4.5% ASA II patients, 28.8% ASA III patients, 47% ASA IV patients and 19.7% ASA V patients.
The technique used for the placement of gallbladder drainage was mainly transperitoneal (93.9%), and the transhepatic approach was only used in 4 patients. The median time elapsed between the time of diagnosis or initiation of antibiotic treatment and the placement of the PC was one day (p25 one day, p75 4 days).
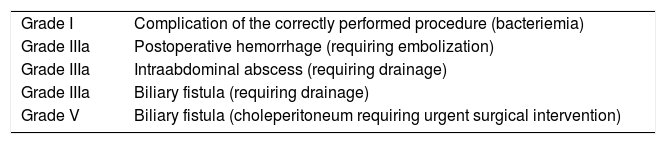
In terms of adverse events, 21% of the patients who underwent PC presented an AE after drain tube placement and during hospitalization for the AC episode (14 out of 66 patients). These 14 patients presented a total of 22 AE. Only 5 AE presented by 5 patients (7.6%) could be attributed to the PC itself. These are shown in Table 1 according to the gradation of the Dindo-Clavien classification.
AE grades presented after PC during hospitalization according to the Dindo–Clavien classification.
| Grade I | Complication of the correctly performed procedure (bacteriemia) |
| Grade IIIa | Postoperative hemorrhage (requiring embolization) |
| Grade IIIa | Intraabdominal abscess (requiring drainage) |
| Grade IIIa | Biliary fistula (requiring drainage) |
| Grade V | Biliary fistula (choleperitoneum requiring urgent surgical intervention) |
EA, adverse effect; PC, percutaneous cholecystostomy.
The hospital stay was a median of 12 days (p25 9 days, p75 18 days), while the hospital stay after the procedure was a median of 10 days (p25 7 days, p75 14 days).
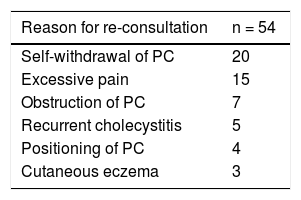
In the follow-up of the patients once the acute process had been overcome, 30 patients (45.5%) required re-consultation for different reasons related to PC. A total of 54 events related to morbidity attributable to said drainage have been collected (Table 2). These re-consultations have involved radiological verification of the drain tube (transcholecystostomy cholangiography) except for patients who have re-consulted for skin changes (eczema).
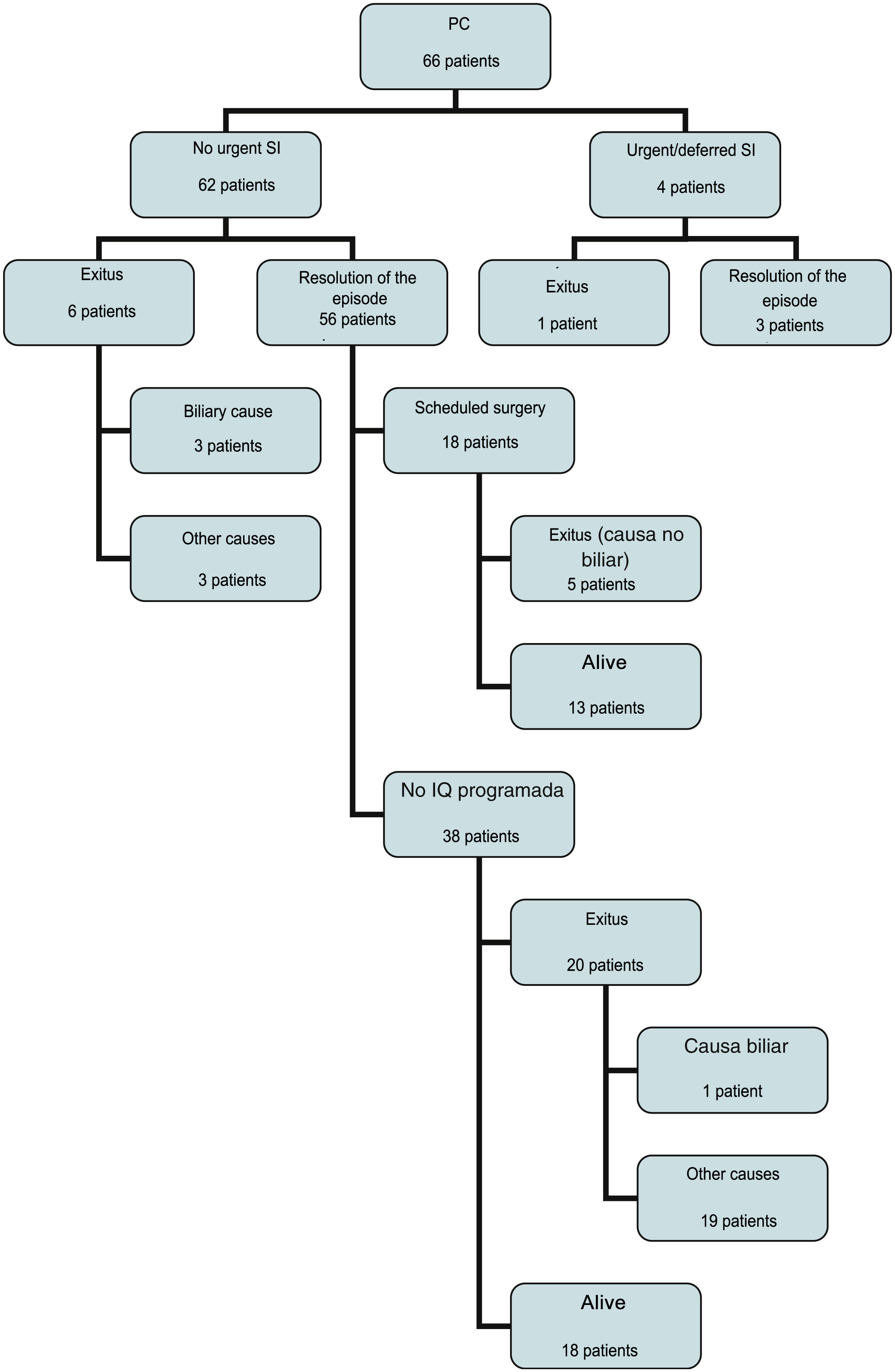
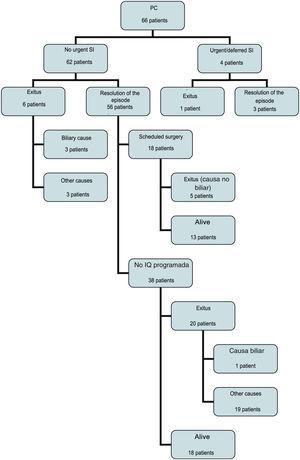
After PC, one-third of the patients (22 patients) have undergone cholecystectomy. Urgent surgery was performed due to failure of the percutaneous treatment in 2 patients, 2 and 4 days after placement of the PC and in another 2 patients as deferred surgery after 74 and 98 days due to AC recurrence. The patient operated on 4 days after PC presented choleperitoneum with an unfavorable evolution that led to his death. This was the only case of mortality that we could attribute to a complication of the technique (mortality 1.5%). The remaining patients underwent elective surgery (Fig. 3), and the procedure was laparoscopic in 16 patients (72.7%).
Taking into account the rate of patients successfully treated using this technique, we can confirm that it has been effective in 59 patients (89.4% of cases).
During follow-up, almost half of the patients died (32 patients; Fig. 3). Among the patients who did not undergo surgery and who are still alive, only 3 continue with the PC to date.
DiscussionCurrently, there are no doubts about the role of cholecystectomy in the treatment of AC, and laparoscopic cholecystectomy is the gold standard treatment for acute disease. However, PC is a resource to be considered as an alternative to surgery and antibiotic treatment in inoperable patients. Loozen et al.13 have recently published a prospective study comparing both techniques (urgent cholecystectomy vs PC) by randomizing the patients. This study has been completed earlier than expected because it has shown that PC presents greater morbidity, greater need for reoperations, and is associated with greater recurrence of biliary disease compared to cholecystectomy. These results confirm that PC should be indicated in highly selected patients who are not candidates for urgent cholecystectomy.
Regarding the technique used to perform PC, the literature14,15 recommends the percutaneous transhepatic technique or direct gallbladder puncture. In our series, there is a definite tendency to perform an ultrasound-guided percutaneous transperitoneal approach. It is possible that the high number of re-consultations due to loss or self-withdrawal of the PC is due to this fact. Although the literature consulted in this regard does not show statistically significant differences in the rate of complications between the two approaches,16 transhepatic access is associated with a lower risk of bile leak (choleperitoneum), provides greater drainage stability and faster maturation of the tract, and is also considered the safest method in patients with ascites and colonic interposition.17 Nevertheless, it is associated with higher rates of hepatic hemorrhage and iatrogenic pneumothorax.18
In the literature published to date, no publication presents data with prospective collection of AE associated with the PC technique. As this is the greatest strength of our study, we can affirm that a small percentage of patients who underwent this procedure have presented some AE during the acute episode that can be attributed to the technique. The rate of complications presented by the retrospective studies consulted varies from 5.6% to 26.3%,19–21 with mortality rate of up to 10% related with the procedure,22,23 while our morbidity (7.5%) and mortality (1.5%) figures are at the lower limit.
In contrast, during the follow-up of our patients, we observed a high rate of re-consultation after hospital discharge, requiring a high number of extraordinary radiological follow-up studies in addition to the already established visits every six months to proceed with drain replacement. This fact has led to a prioritization of these patients on the waiting list to undergo cholecystectomy when they are finally considered operable, as recommended in the literature.24 In addition, there is a greater tendency to remove the drain early in inoperable patients who are candidates for its withdrawal.
However, we are aware of the limitation presented by the fact that this is a descriptive observational study that was conducted in a single hospital.
ConclusionsWe believe that PC is a safe and effective technique because it is associated with a low incidence of AE and mortality. It should be considered a bridge technique or definitive alternative in patients who do not require urgent cholecystectomy after the failure of conservative treatment with antibiotics. However, given the high rate of re-consultation and the radiological checks that patients require during follow-up, it should only be used in selected cases.
The high mortality rate observed in the follow-up of non-operated patients attributed to other causes supports the appropriate indication of PC in patients with severe associated comorbidity.
Conflict of interestsNone of the authors have conflicts of interests to declare.
FundingThis study has received no specific funding from public, commercial or non-profit organizations.
Please cite this article as: Bejarano González N, Romaguera Monzonís A, Rebasa Cladera P, García Monforte N, Labró Ciurans M, Badia Closa J, et al. ¿Es segura y eficaz la colecistostomía percutánea en la colecistitis aguda? Análisis de los efectos adversos asociados a la técnica. Cir Esp. 2022;100:281–287.