Intestinal obstruction secondary to heterotopic pancreas (HP) is a rare pathology. We present the case of a 42-year-old male patient with no history of interest who came to our emergency department due to continuous, diffuse abdominal pain over approximately the previous 24h. He also presented nausea and vomiting, with no other associated symptoms.
Physical examination revealed hemodynamic stability and marked abdominal distension but no signs of peritoneal irritation.
Blood work showed an increase in leukocytes (17×109/L) with neutrophilia. Biochemistry analysis showed amylase and lipase in normal ranges, as well as the liver profile, except for slightly elevated GOT and GPT (60 and 68IU/L). Likewise, abdominal X-ray detected air-fluid levels in the small intestine. In the absence of signs of seriousness and the good clinical condition of the patient, we decided to admit the patient for conservative management.
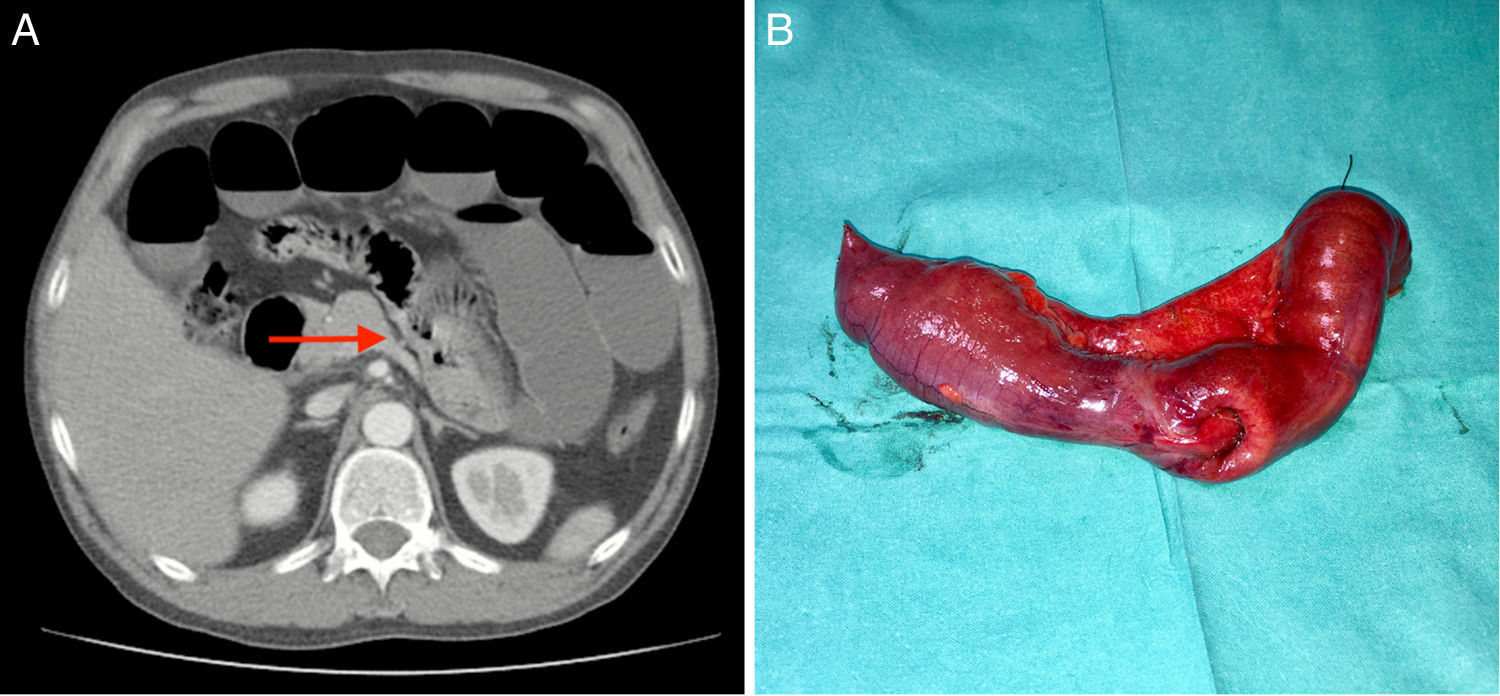
24h after admission, the patient showed no improvement in symptoms or analytical parameters. Therefore, a computed tomography (CT) scan was done with intravenous contrast, which showed proximal dilatation of small bowel loops with uptake in a segment of the jejunum, suggesting intestinal intussusception, with little free fluid in the bottom of the sac. Given these findings, we decided to proceed with surgery (Figs. 1 and 2).
Under general anesthesia, exploratory laparotomy confirmed the presence of intestinal intussusception caused by a tumor and exophytic growth, with no involvement of neighboring organs. Retrograde drainage was conducted of the content proximal to the stoppage and the lesion was resected with free margins of (5cm). The procedure was completed with isoperistaltic side-to-side anastomosis. The patient progressed favorably, with no complications, and was discharged on the fifth day post-op.
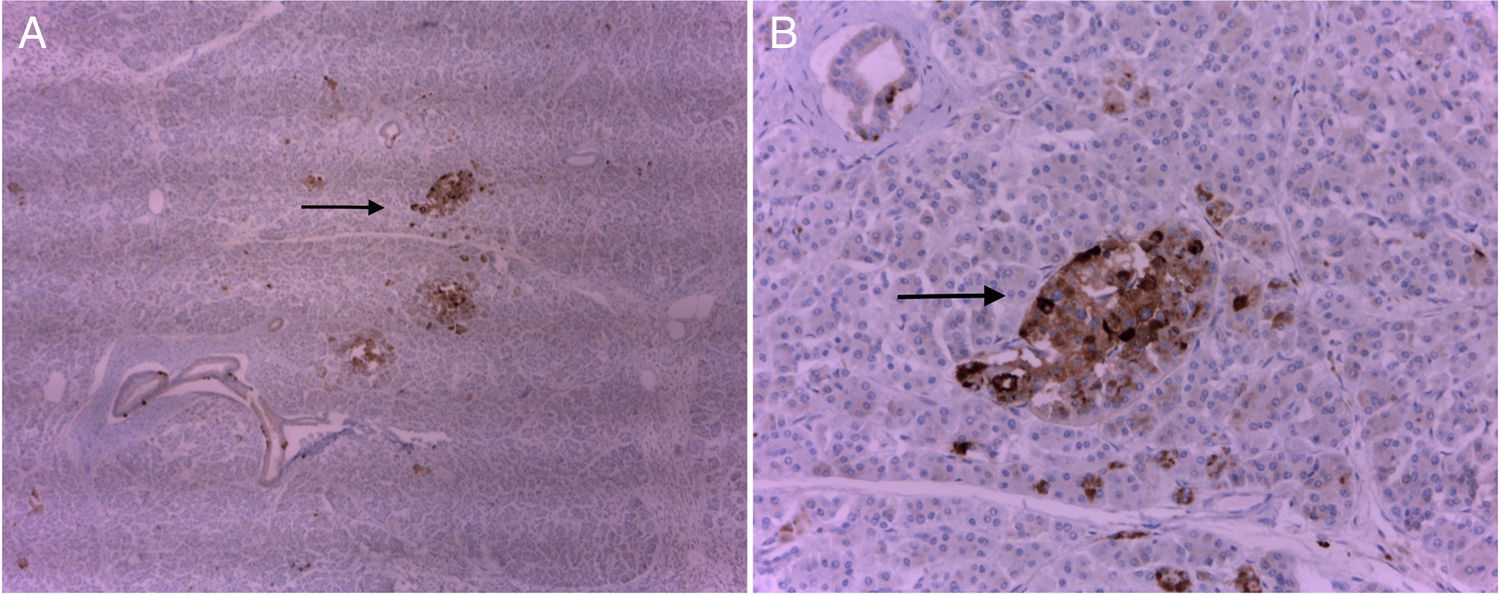
In the microscopic study of the surgical piece, the tumor was described as normal pancreatic tissue, exocrine with lobules and ducts. Mentioned was also made of endocrine tissue with islets of Langerhans. Microabscessed foci of polymorphonuclear cells were observed in the wall of the loop and surrounding the heterotopic pancreatic tissue.
After 6 months of follow-up, the patient was clinically asymptomatic. On the follow-up CT, no notable alterations were found.
HP is defined as “pancreatic tissue that has no vascular or anatomical communication with the pancreas itself”.1–3 The first case of HP developed in an ileal diverticulum and was reported by Jean Schultz in 1727, but the first histological confirmation dates from the 19th century, by Klob in 1859.4 According to necropsy studies, the prevalence is between 0.6% and 12.7%, with a predominance in males in their fifth and sixth decades of life.3,5 HP is most often found in the stomach (25%–38%), and the antrum is the most common place in 90%. It can also appear in the duodenum (17%–36%), jejunum (15%–21%) and other less common places such as bile ducts, mesentery, omentum, etc.3,6,7
There are basically 2 theories about its origin:
- -
The first suggests that the pancreas is created from the invagination of endodermal tissue in the primitive duodenum. The head of the pancreas is born from its ventral exposure, and the body and tail from its dorsal exposure. This is called the “poor position” theory because it refers to the fact that, during rotation of the proximal intestine, some elements of the primitive pancreas can be separated and thereby eventually develop into other tissues.1,6,8
- -
The second is called the “metaplasia theory”. This puts forth the possibility that the HP is born from areas of pancreatic metaplasia of the endoderm, which migrate to the submucosa during embryogenesis.8,9
The majority of cases are asymptomatic and are found during an abdominal study due to another cause, during laparotomy or during autopsy.2,3,5,6,8–10 Symptoms depend on the size and location of the lesion. Thus, it can more frequently cause abdominal pain, gastrointestinal bleeding, nausea and/or vomiting, among other less specific symptoms.11,12 These symptoms predominate when the lesion is greater than 1.5cm or is in a pre-pyloric position.2,3,6,9 It is rare for an injury to cause obstruction or intussusception. However, lesions of this type in the context of an emergency can simulate other entities, such as stromal tumors. The secretion of pancreatic hormones or enzymes and the subsequent inflammation or chemical irritation of the tissue may also be related to the initial symptoms.10–12 Likewise, if the heterotopic pancreatic tissue is functionally viable, it can cause pancreatitis, pseudocysts, abscesses and/or neoformations, such as adenocarcinoma of the pancreas.11
The recommended initial study is upper gastrointestinal endoscopy if the HP is located in the stomach or first portion of the duodenum.8 Currently, complementary tests such as endoscopic ultrasound have an important role and are able to diagnose HP between 0.5 and 2cm in diameter, and, used together with fine needle aspiration (FNA), sensitivity can reach 80%–100%.3,9 Other detection methods, such as CT, barium transit, magnetic resonance imaging or capsule endoscopy may be useful depending on the location and clinical symptoms. This entity is usually an incidental finding and its diagnosis is difficult as it is not initially considered in the differential diagnosis.
The criterion to indicate a more important intervention is the presence of symptoms due to the location or secondary to a complication. It is recommended to perform complete exeresis of the HP if it is found incidentally during surgery, if it has a diameter equal to or greater than 3cm, and obviously if there are symptoms.6,10 Currently, there are not enough cases to recommend endoscopic follow-up versus surgical intervention.6
Please cite this article as: Falckenheiner Soria J, Bernal Moreno D, Flores Rivera JM, Toro Guillen M, Lérida Vaca JL. Páncreas heterotópico. Obstrucción intestinal por invaginación del yeyuno. Cir Esp. 2018;96:237–239.