The high level of therapeutic response obtained with combinations of fluorouracil and leucovorin with oxaliplatin or irinotecan and with monoclonal antibodies such as cetuximab or bevacizumab, and the results of the EORTC trial with peri-operative chemotherapy,1 have encouraged us to use neoadjuvant chemotherapy in a large number of patients with liver metastases from colorectal cancer. Metastases can disappear or reduce with neoadjuvant treatment after a few cycles, in such a way that their subsequent location can become very difficult. This is aggravated when liver toxicity occurs from therapeutic agents, giving the hepatic parenchyma an echogenicity which is highly homogenous with metastases. Furthermore, as we find a real pathological complete response in only 10% of lesions that disappear, resection of the hepatic parenchyma where the metastasis was located remains necessary.2 In order to avoid these location problems, some authors have described a technique of marking liver metastases prior to starting neoadjuvant treatment.3,4 This involves placing one or two coils next to the metastasis under radiological control, by ultrasound or CT scan, before starting chemotherapy treatment. Once the neoadjuvant treatment has been completed, the coils can be located by intraoperative ultrasound during the surgical procedure, even though the metastasis has either disappeared, or is not visible.
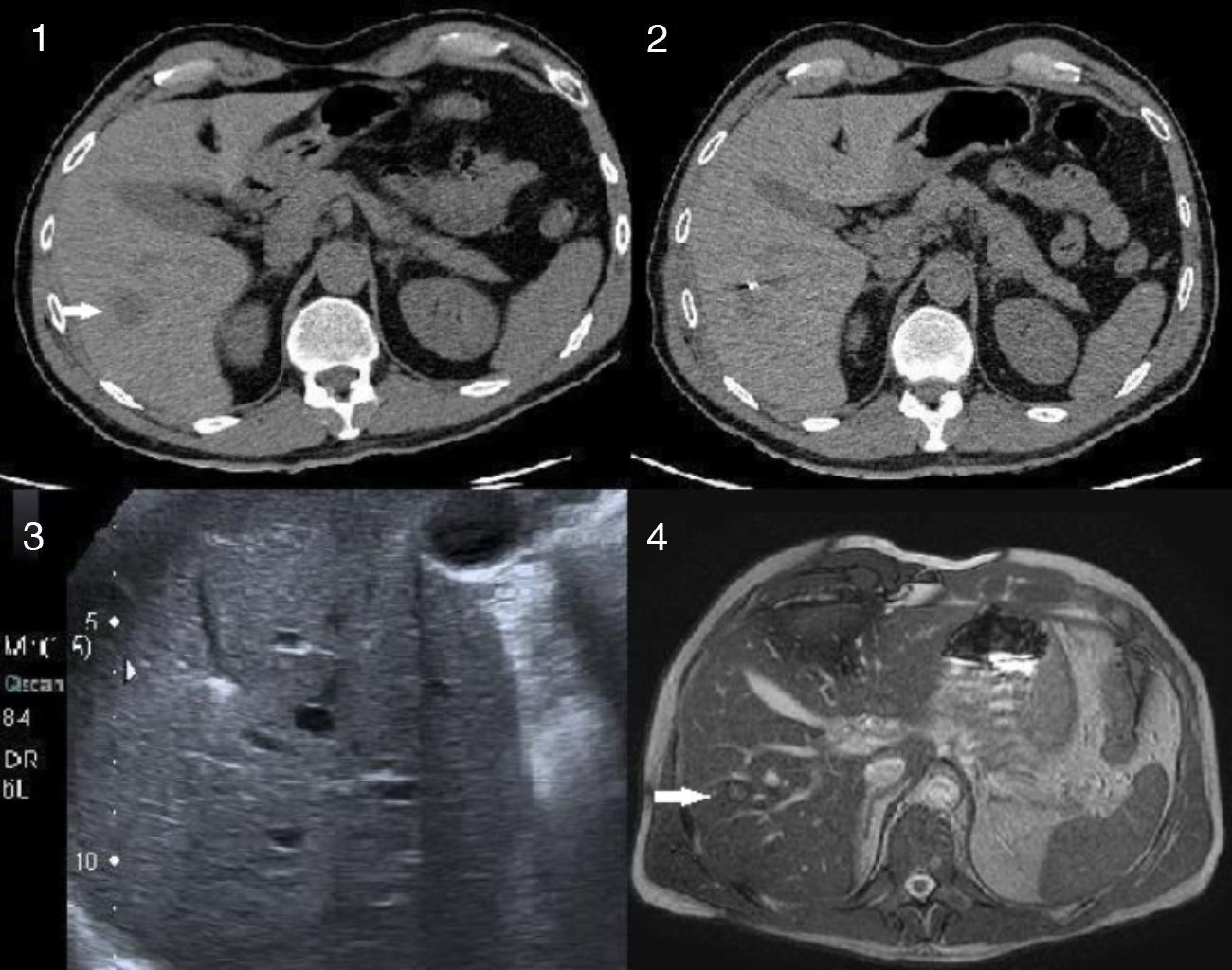
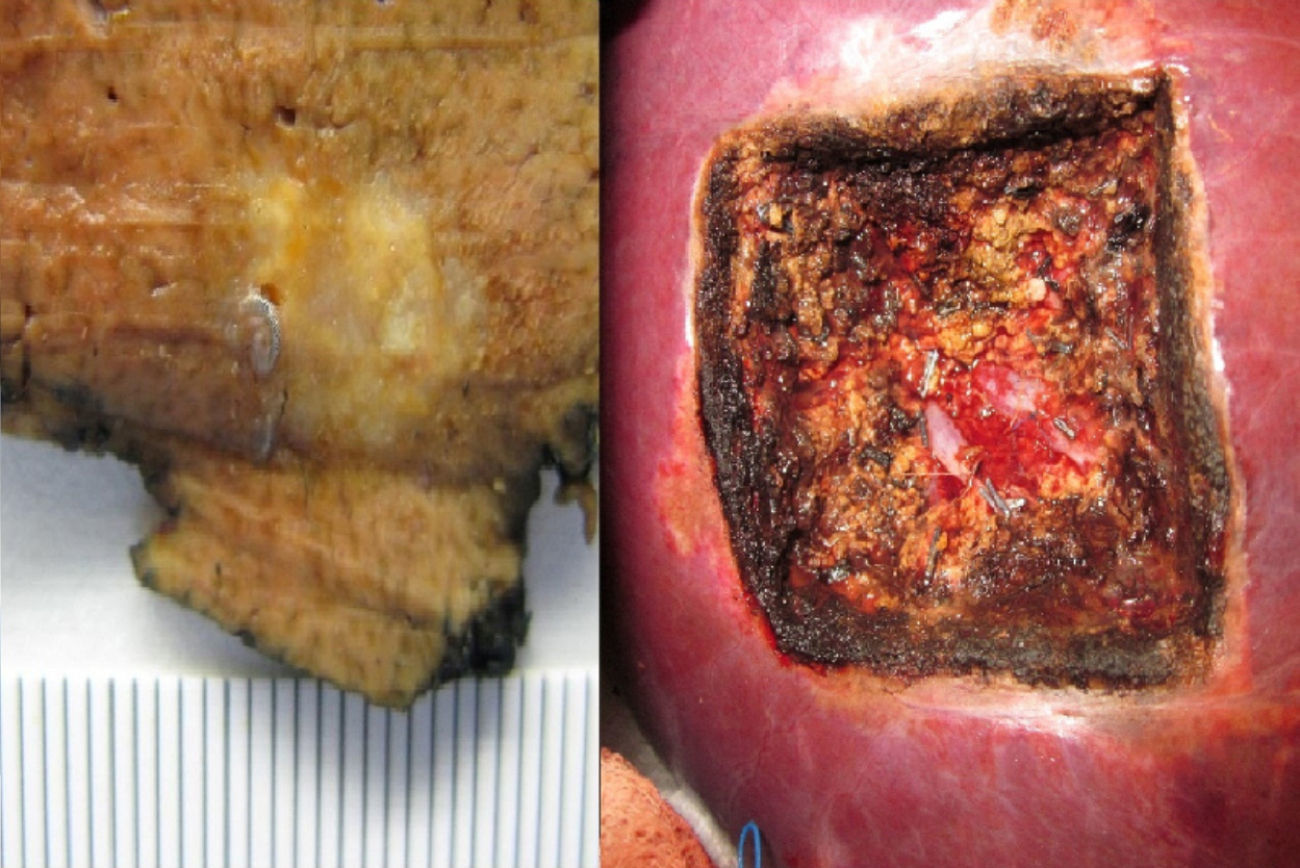
The following is a case where this marking technique was necessary. The patient was a 47-year-old male diagnosed with an adenocarcinoma of the colon, 15cm from the anal margin; the extension study of the carcinoma revealed hepatic metastasis of 2.5cm located deep in the intersection of segments v-vi-vii-viii (Fig. 1), but at sufficient distance from the vascular pedicles of these segments to allow a non-anatomical resection to be performed. The study also revealed a left-sided paraaortic adenopathy, cranial to the origin of the inferior mesenteric (artery), and another precaval infrarenal lymph node, of 2 and 3cm respectively, with pathological uptake shown on PET scan. It was decided to start treatment with systemic chemotherapy and carry out simultaneous surgical resection of all lesions if there was a response. Given the probable disappearance of the liver metastasis, and/or its very difficult intra-operative location in the event of a response, it was decided to mark the lesion prior to starting chemotherapy. Our team of interventional radiologists, guided by CT, placed a coil in the deep margin of the lesion. The patient received three cycles of FOLFOX and was reassessed using PET/CT and hepatic MRI. The PET/CT showed metabolic and complete radiological response at hepatic level–the lesion was not seen – and partial response of the primary tumour and retroperitoneal adenopathy. The MRI detected liver metastasis with a reduction in size to 1cm. We performed a pre-operative liver ultrasound which enabled us to see the coil but not the metastasis. Given the evidence of response to the chemotherapy, it was decided to perform one-stage surgery of the entire disease. Surgical exploration showed the primary tumour at the recto-sigmoid junction and the retroperitoneal adenopathies described above; the hepatic lesion was not palpable. The coil was located using intra-operative ultrasound, without it being possible to clearly distinguish the metastasis. The primary tumour and precaval and paraaortic lymph node metastases were resected first. We then proceeded to resect the metastasis by non-anatomical hepatectomy on segments v-vi-vii-viii. Continuously guided by ultrasound, we resected the hepatic parenchyma area around the coils, taking into account the initial size of the lesion, and achieving at least a margin of 1cm in depth from the coils. We performed the resection with electrocautery and ultrasonic aspirator, without hilar clamping. When the resection sample had been extracted, we confirmed the presence of an eight mm lesion with free margins, situated 8mm from the deep margin (Fig. 2). The histology study confirmed that it was a colorectal adenocarcinoma metastasis. There were no complications in the post-operative period; the patient was discharged on the eighth day after surgery.
The CT scan shows a 2.5cm metastasis at the confluence of segments v-vi-vii-viii, which is resectable by non-anatomical hepatectomy. Marking with coils prior to neoadjuvant treatment (2) allows subsequent location of the metastasis with ultrasound although it is not ultrasonically visible (3). (4) The post chemotherapy MRI scan shows the metastasis which is 1cm in size.
High risk patients with synchronic hepatic metastasis, “potentially resectable” metastasis or synchronic extrahepatic disease will be treated with chemotherapy prior to hepatic resection.5 This marking technique is indicated when these patients present with a small, deep metastasis, which is likely to disappear if there is a good response to treatment. The technique is simple, reproducible and has a low risk of complications. It allows a parenchyma-sparing resection, avoiding unnecessary major anatomical hepatectomies and having to wait for the metastasis to reappear to treat it at a second stage. In our case, only a right-sided hepatectomy could have ensured resection if the lesion had not been marked. It is important for the coil to be placed in the deep edge of the lesion, without crossing it, to prevent it from spreading. Pre-operative ultrasound, although not essential, allows us to check that the coils are easily visible. The use of intra-operative ultrasound is essential. Hepatic resection will be guided exclusively by ultrasonic image, and the resection margins will depend on the correct knowledge of this technique. Intra-operatively, it must be checked that the metastasis and/or the coils are in the resection sample.
Please cite this article as: Alonso Casado O, González Moreno S, Encinas García S, Rojo Sebastián A, Olavarría Delgado A. Marcaje de metástasis hepática antes de quimioterapia neoadyuvante para su posterior localización y resección mediante hepatectomía no anatómica. Cir Esp. 2013;91:687–689.