Hepatic adenomatosis is a rare disease defined by the presence of multiple lesions in a normal liver parenchyma. Described for the first time by Flejou in 1985, the number of adenomatous lesions needed to diagnose this disease was arbitrarily established to be 10.1 Later, Ribeiro considered the presence of 4 or more lesions to be sufficient.2
We present a new case of hepatic adenomatosis in a young man with a previous history of anabolic steroid use who was hospitalized due to acute abdominal pain secondary to an intratumoral hemorrhage.
Although hepatic adenomatosis has an uncertain etiology, it has been associated with malformations or vascular anomalies such as focal nodular hyperplasia, the absence of portal vein or hepatic venous shunt. Autosomal transmission has also been reported in 4 cases of this pathology in the same family.3 Initially, an equal distribution was described between the two genders, although recent publications show a clear predominance of affected females, related with fatty liver and glycogen storage diseases. The association with the use of oral contraception and androgenic steroids is uncertain,3–5 although their use is present in 10%–24% of patients with liver adenomas.
Two types of hepatic adenomatosis have been described. The massive form presents with hepatomegaly and deformed liver due to large tumor nodules, whose size in our patient ranged between 2 and 10cm in diameter. These nodules can sometimes advance rapidly. The other type is multifocal, with a normal-sized liver that is not deformed, with one or 2 adenomas predominating over the smallest lesions, with an apparently less aggressive clinical course.4
It generally occurs in healthy livers. Patients are usually asymptomatic, with normal liver analyses, although occasionally elevated liver enzymes for cholestasis are detected (alkaline phosphatase and gamma-glutamyl transferase) depending on the volume that the tumors occupy.1,4,5
The diagnosis is usually by chance in most patients or secondary to a hemorrhage (intraperitoneal or intratumoral). The most useful method for the initial diagnosis is computed tomography (CT) or magnetic resonance imaging (MRI).5,6 The diagnosis is confirmed by pathology studies.7 Typically, adenomas are well-defined and may have a partial or total capsule. The differential diagnosis should include multifocal hepatocellular carcinoma and metastatic disease.1,5,7
The complications that these patients frequently present are bleeding and the possibility of malignant degeneration of the lesions.1,7
The definitive treatment is still controversial; therapeutic options include clinical follow-up, liver resection, and liver transplantation (LT).2–4,8,9 As it is not possible to resect all the lesions (except with LT), symptomatic lesions that are accessible by surgery or are at risk for bleeding should be resected. Other treatment methods, such as embolization and radiofrequency ablation, may be useful complements in selected cases.4–7,10 The only definitive solution for this disease is LT, although the benefits of transplantation to prevent bleeding or malignant degeneration in these young patients should be balanced against the potential risks that LT entails. It is recommended for malignant transformation of an adenoma (infrequent but feasible) and in very symptomatic patients with several unresectable tumors.8,9
Follow-up should be done with CT and MRI tests. Alpha-fetoprotein should be monitored given the risk of malignant degeneration, although it is difficult to estimate this risk because of the rarity of the lesions.
Case ReportWe present the case of a 25-year-old male with no medical history of interest who was using anabolic steroids. He came to our Emergency Department due to sudden-onset epigastric abdominal pain.
Upon initial examination, the patient was pale and diaphoretic, with tachycardia and hypotension. The abdomen was painful on palpation, with signs of peritoneal irritation. The work-up showed high transaminases (AST: 234UI/L, ALT: 136UI/L, GGT: 97UI/L) and discrete leukocytosis (13.2×109/L), with no alteration of the red blood cell series or coagulation.
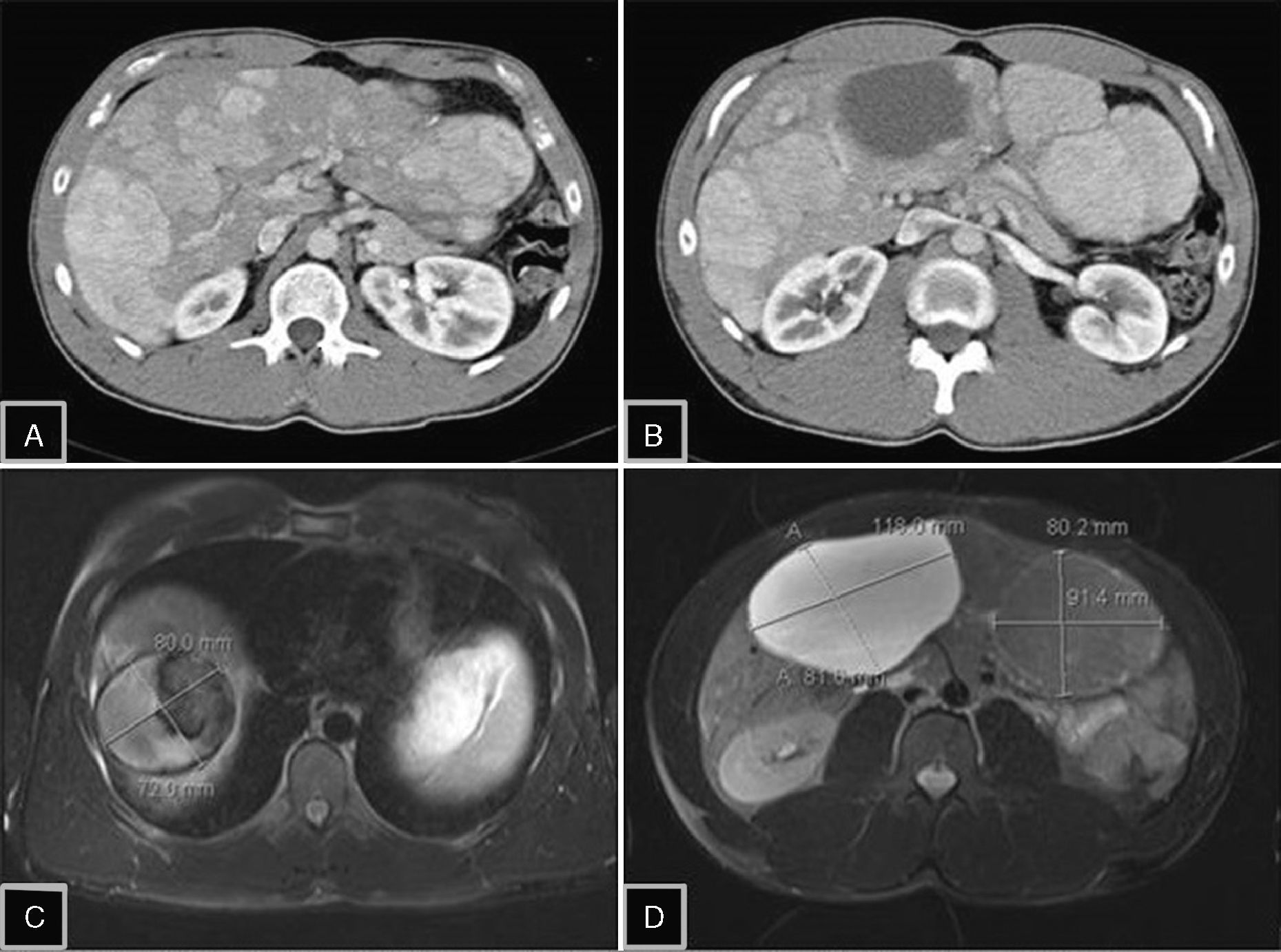
Ultrasound detected hepatomegaly with multiple solid lesions and others with a liquid component that diffusely affected both liver lobes. The largest measured 12cm in segment IV in the right liver lobe (RLL). The study was completed with CT and later with MRI, which established the diagnosis of hepatic adenomatosis. Several hypervascular lesions were detected, the largest of which were in segment IVb 11cm×12cm×8.5cm; segment V/VI 11cm×8.1cm (both with signs of bleeding) and between segment VII/VIII 8.2cm×7.2cm; segment III 9.1×8cm; segment VII 4×3cm. Several smaller solid lesions were detected in the rest of the parenchyma. The preserved parenchyma presented no disease (Fig. 1). Alpha-fetoprotein levels were within normal range.
(A) Abdominal computed tomography (CT) with contrast showing the presence of multiple adenomas with enhancement in the arterial phase, occupying practically the entire liver parenchyma; (B) CT with adenomatous lesion, heterogeneous due to intratumoral bleeding in segment IV; (C) magnetic resonance imaging (MRI) enhanced in T1 with saturation of the fat, which shows evidence of hyperintense lesion in segment VIII due to the intralesional hemorrhagic component; (D) MRI enhanced in T2 with saturation of the fat: 2 lesions are identified, one hyperintense with cystic component in segments V–VI, and another isointense lesion in segment III, a typical characteristic of hepatic adenoma.
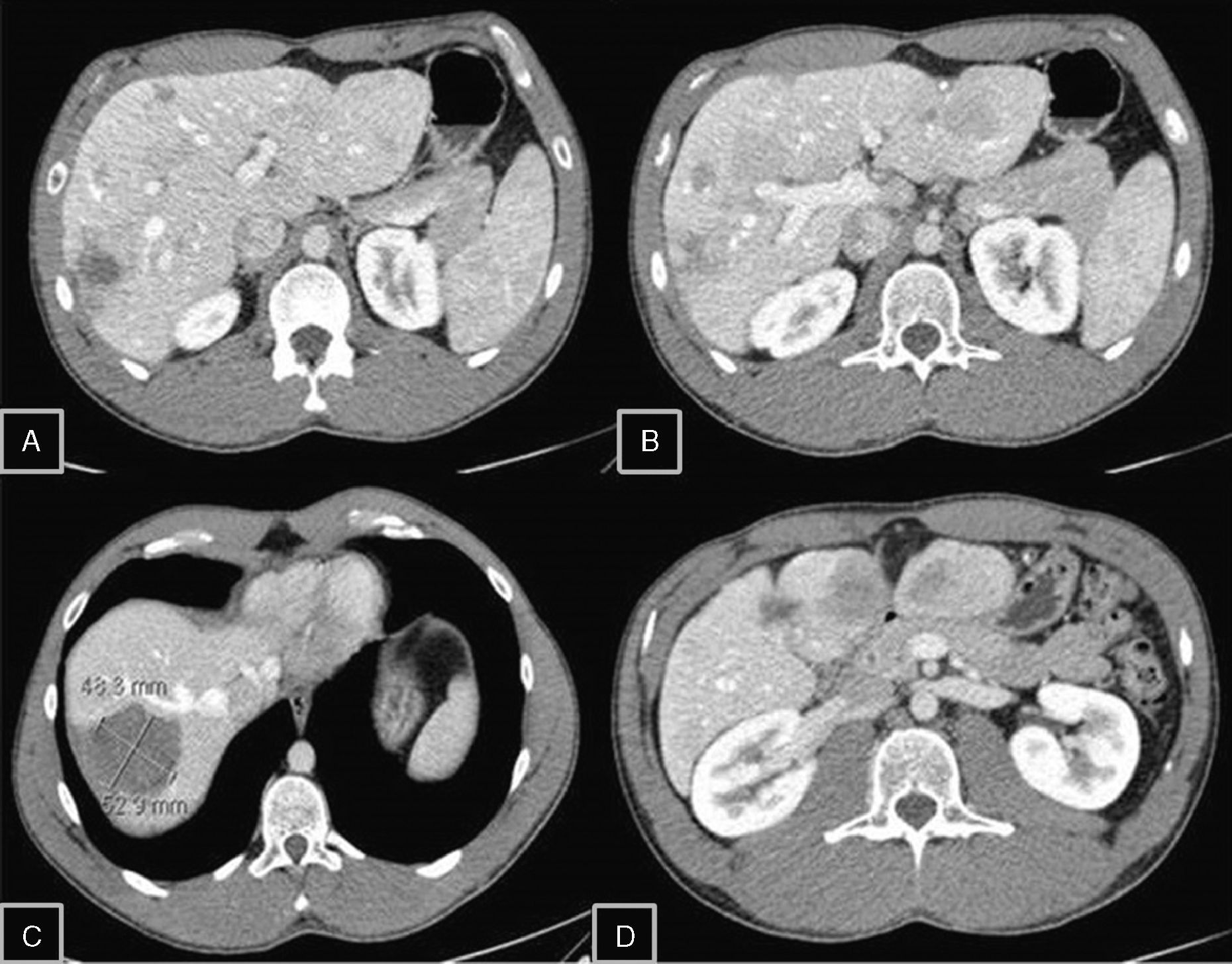
After the acute symptoms subsided, and given the impossibility to resect the lesions, liver transplantation was proposed to the patient, which was rejected. He is currently being followed with scheduled office visits and has presented a decrease in the size of the lesions with hemorrhagic component and alpha-fetoprotein within normal range (Fig. 2).
Follow-up CT 3 years later: (A–D) a decreased number and size of the hepatic adenomas are seen, as well as a change in density; (C) reduced size and hemorrhagic component of the adenoma in segment VIII, with no signs of re-bleeding; (D) partial reabsorption of the cystic component in segment V.
Please cite this article as: Lucas E, Pareja E, Carvajal N, Pacheco A, Moya Á. Adenomatosis hepática: una enfermedad de tratamiento controvertido. Cir Esp. 2014;92:284–286.