The objectives of “glove port” liver resection are to minimize postoperative pain, improve esthetic results, lower procedure costs and maintain patient safety. The access device proposed by our Unit is made up of a standard skin retractor (medium-sized Alexis®) and a number 8 surgical glove.
We present the case report of a 72-year-old patient who was diagnosed with ovarian cancer in February 2013. The patient underwent surgery, where a stenosing sigmoid tumor with ovarian infiltration and 2 liver metastases in segment 4b (1cm in diameter) and segments 2 and 3 (10–11cm in diameter) were found. We performed a hysterectomy with double adnexectomy, sigmoidectomy and limited hepatectomy of segment 4b as an initial phase.
After 10 cycles of chemotherapy with Folfox and Bevacizumab, we re-evaluated the patient, who had a good response. In September 2013, it was decided to schedule a surgical intervention of the liver metastasis in segments 2 and 3.
The surgical technique that we used included a skin incision over the previous laparotomy with an orifice in the aponeurosis that measured 5–6cm in length, which allowed for proper placement of the skin retractor as well as a sufficiently large orifice for the extraction of liver segments 2 and 3. Once the adherences to the abdominal wall were released, the interior ring was put in place. With the placement of the intraperitoneal device, we correctly fitted the external ring, turning the device to achieve proper placement in the external abdominal wall and thus obtaining correct retraction. Prior to giving the last 2 turns to the external ring, we fitted the glove to be included in the last two turns so that the device had no air leaks and remained set in place during the entire surgical intervention.
In a manner that is similar to what we have described in other articles for cholecystectomy and appendectomy, we cut 2–3cm of the glove fingers in order to allow for greater fixation of the trocar to the glove and greater stability as well as good mobility. We have used the same instruments as in conventional laparoscopy since the device does not restrict their size. We introduced two 11-mm trocars in the fourth and second fingers, and in the middle finger we placed the optical trocar. The trocars were set in place by tying the fingers of the other glove around them, which also sealed the device (Fig. 1).
Likewise, this access method provides a good entry orifice for the instruments that need to be interchanged during surgery (camera, endostapler, Cusa®, etc.) while still maintaining pneumoperitoneum at all times.
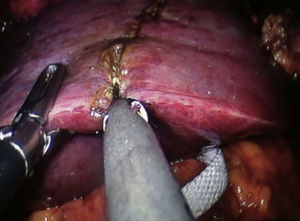
First of all, the adherences were released from the liver parenchyma and the hepatoduodenal ligament in order to perform the intraoperative ultrasound and the Pringle maneuver. With intraoperative ultrasound done through the skin retractor, we identified a liver metastasis in segment 2 and 3 that measured 10cm in diameter, and a malignant-looking scar in the bed of the previous resection in segment 4b. Through this single incision, we also palpated the liver parenchyma. We mounted the device, marking the lesions and then resecting them with a CUSA®, Ultracision harmonic scalpel, endostapler and conventional clip applier (Fig. 2).
Hemostasis of the liver bed was achieved. Once the surgical specimen was free, it was held by retractor forceps. When the glove was detached from the retractor, it was able to be extracted through the orifice of the Alexis®. We should also mention the additional savings when using the skin retractor as it enables the surgeons to not have to use an extractor bag for the surgical specimen. The skin incision was closed with staples.
We have used this technique in a patient in September 2013, without immediate complications. With its use, we have found several advantages, and not just those related to cost.1,2 The use of this device is easy and allows for 5 instruments to be used simultaneously, while the majority of commercially available devices have only 3 or 4 working ports.
Glove ports also offer certain benefits to the single-incision technique as this device provides a larger range of motion. The instruments can be interchanged, crossed and rotated according to the requirements of the situation. In addition, there is freedom of movement both in the horizontal as well as the vertical planes. Friction between the trocars and the abdominal wall is avoided, which could be an advantage with regards to wall trauma as seen in a decrease in postoperative pain.3,4
The use of the glove port is an inexpensive, safe and easy technique, which should therefore be considered in numerous procedures,5–9 such as in accessible liver resections. It is a technique that is, at the very least, similar to specifically-designed commercial devices. Due to its ease of use and to the fact that it is a reproducible, low-cost technique, we believe that glove ports can be used in uncomplicated liver resections in selected patients.
Please cite this article as: Mir Labrador J, Gumbau Puchol V. Segmentectomía 2-3 hepática glove port. Cir Esp. 2014;92:562–563.