Myelolipomas are rare tumors that have a greater incidence in patients between the ages of 50 and 60; they show a preference for the female sex1,2 and are usually located in the suprarenal glands.1,3,4 A review of the literature shows that the presacral region is the most prevalent extraadrenal location, although they have also been reported in the mediastinum, lungs, liver or stomach.4,5 These lesions are benign, well-outlined and made up of fatty tissue and myeloid elements; they are generally hormonally inactive, although they can be related with Conn's syndrome, Cushing's syndrome or adrenal hyperplasia.2,3 Until now, there have been no documented cases of malignant degeneration of this type of tumor formation.4,6 Their diagnosis is generally incidental and is becoming more and more frequent due to the advances in imaging techniques.4,7
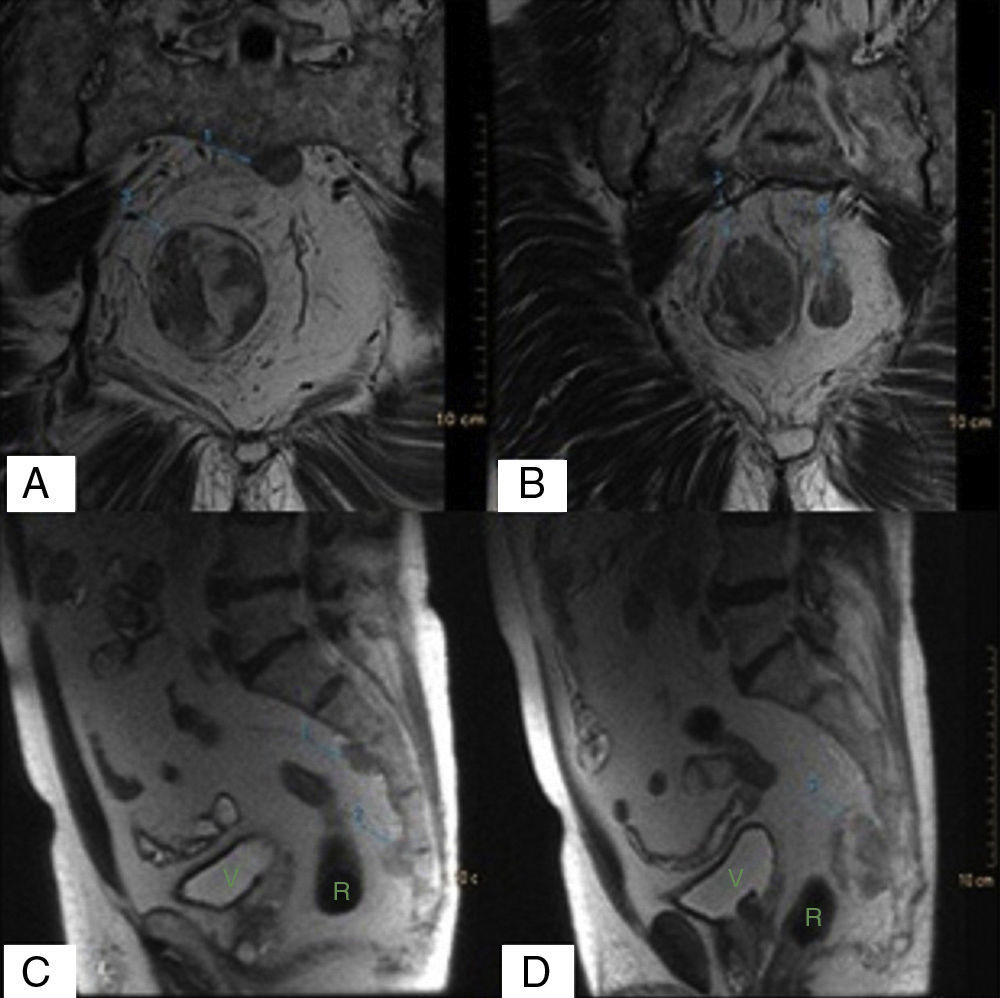
We present the case of a 74-year-old male whose only medical history of interest was arterial hypertension. He was being studied because of non-specific abdominal discomfort, constipation and radiculopathy in the left lower extremity. Magnetic resonance imaging showed a soft tissue tumor in the right presacral (S4) area with a 4.5cm craniocaudal axis and a 3.2cm anteroposterior axis, heterogeneous signal pattern and some interior images that suggested a probable fatty component. Two satellite tumor nodules were observed with discretely pathologic uptake in the post-contrast study. There was no evidence of associated bone involvement or communication with the sacral spinal canal (Fig. 1).
The differential diagnosis of presacral fat-containing masses should be made with several pathologies, including liposarcoma, teratoma, extramedullary hematopoiesis and neurogenic tumors like chordomas or neurofibromas.3,4,8 Although magnetic resonance imaging is the study of choice for this type of tumors, it is often not possible to arrive at the correct preoperative diagnosis. In these situations, histology analysis may be indicated because of its importance for later treatment.1,4,9
In this case, and given the high diagnostic suspicion for liposarcoma, the tumor was biopsied with a tomography-guided core needle, following the potential pathway of the resection during later surgery in order to avoid tumor cell dissemination. The pathology study reported the presence of hematopoietic material interspersed with isolated adipocytes, all of which was suggestive of myelolipoma.
There is no consensus about the management of extraadrenal myelolipomas. Because in many cases these tumors are asymptomatic, once the definitive diagnosis is made, periodical follow-up with imaging tests is sufficient in most cases.9,10 Nevertheless, voluminous tumors have a high risk for intratumoral hemorrhage as well as symptoms secondary to the mass effect due to compression of adjacent structures. In the case of a presacral location, urinary retention, constipation, radiculopathy or sciatic pain have been described, along with other symptoms.4,5,10 As our patient was symptomatic and there was risk for hemorrhage due to the size of the lesions, surgery for removal of the tumors was decided.
There are 3 possible different surgical approaches for the resection of presacral tumors. The anterior approach is the choice for tumors whose lower margin is above S4. The posterior approach is preferable for small benign lesions below S3. The combined approach is recommended in cases where the lesion extends both above and below S3.4 In our case, we opted to resect the lesions with a combined approach. Using the anterior approach, an opening was made in the mesorectum and the tumor located at S1 was resected. In a second stage, using the posterior approach, distal sacrectomy was performed from S3, which included the other 2 lesions that the patient presented; biological mesh was used as a pelvic diaphragm.
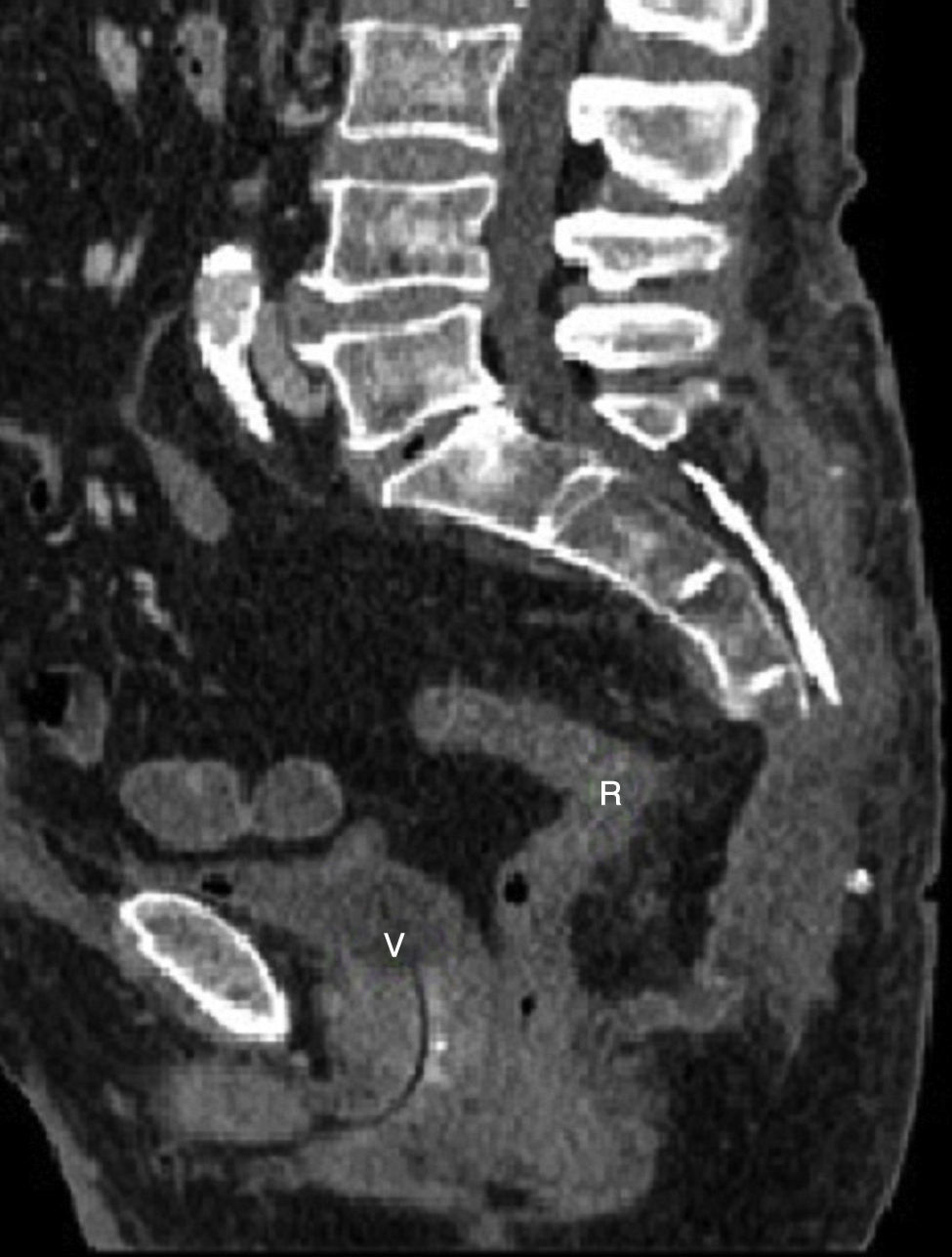
The pathological report of the surgical specimen confirmed the diagnosis of myelolipoma. The patient had a favorable postoperative course. Follow-up tomography demonstrated seroma in the surgical bed and resection of the lesions (Fig. 2). No adjuvant treatment was required given the benign nature of this type of tumors.
No financial support was needed for the development of this manuscript.
Presentation at CongressesThis data has not been previously presented at any congresses.
Please cite this article as: Sagarra Cebolla E, Díaz-Zorita Aguilar B, Rodriguez del Campo J, Ponce Dorrego MD, García Sabrido JL. Mielolipoma gigante presacro. Cir Esp. 2014;92:628–629.