Anastomotic dehiscence in rectal cancer is one of the most feared complications. In the long term, a presacral sinus can form that is difficult to manage. The advent of biological tissue adhesives for the treatment of complex fistulas can be an effective alternative for this type of complication. We present a case of anastomotic dehiscence after low anterior resection and the later formation of a chronic presacral sinus, which was resolved with the endoscopic application of a biological tissue adhesive.
The patient is a 67-year-old woman with no prior medical history of interest. After finalizing treatment with neoadjuvant chemo-radiotherapy, she was treated surgically for a rectal adenocarcinoma 7cm from the anal margin by a laparoscopic low anterior resection with mechanical end-to-end anastomosis without protective ileostomy. The patient was discharged on the 4th day post-op. Three days later, she came to the emergency room with fever and abdominal pain. Abdominal CT scan showed dehiscence of the posterior side of the anastomosis. At reoperation abdominal cavity lavage with a protective ileostomy was performed.
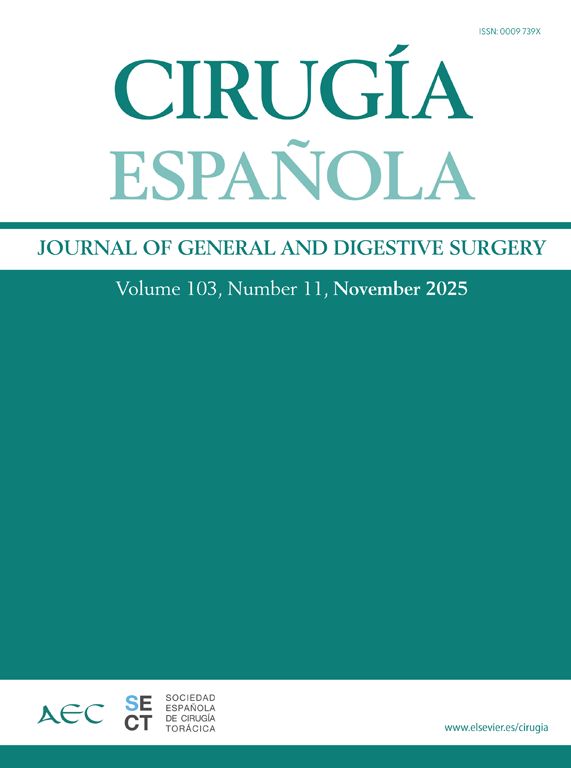
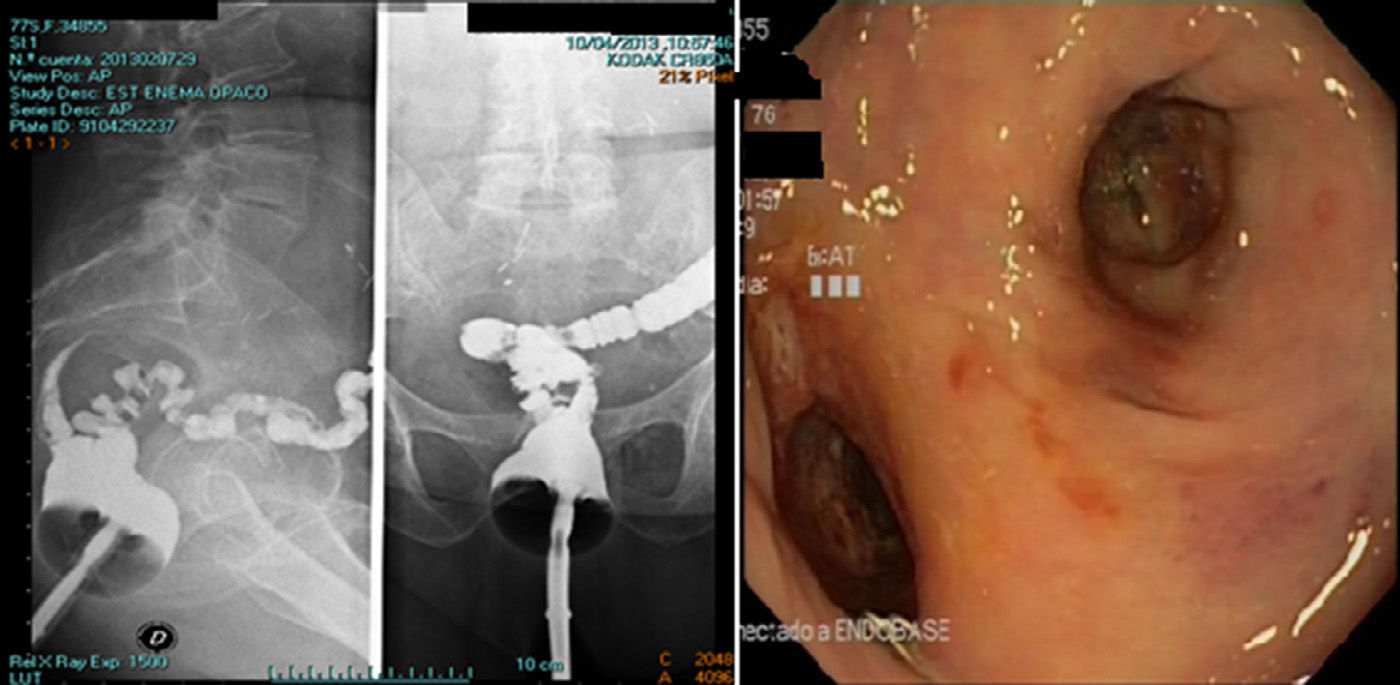
During follow-up, colonoscopy and barium enema (Fig. 1) detected the formation of a presacral sinus on the posterior side of the anastomosis. The sinus was 0.6cm wide and extended to 4cm from the anastomosis. One year after surgery and in spite of conservative measures, the presacral sinus remained, which impeded the closure of the ileostomy. Given this situation, we used colonoscopy to carry out curettage of the presacral sinus in conjunction with the application of a cyanoacrylate biological tissue adhesive (Glubran 2®). Four weeks later, barium enema and follow-up colonoscopy confirmed the closure of the defect (Fig. 2). One month after this resolution, the ileostomy was closed without incident. The patient is currently asymptomatic, with proper intestinal function and no recurrence of the disease.
Anastomotic dehiscence after resection of the rectum is a complication with an important morbidity and mortality. Its incidence varies between 5% and 30%.1 One treatment strategy is the defunctionalization of the anastomosis with an ileostomy, which, although it does not avoid leaks, prevents serious septic complications. The use of protective ileostomy after low anterior resection, even after having received neoadjuvant chemoradiotherapy, depends on the experience of the surgical team and the final result of the anastomosis.
With this management, most leaks resolve spontaneously, although in 1%–5% of cases they may lead to the appearance of a presacral sinus.2 Symptomatic patients present inflammation or sepsis in the pelvic region and are usually studied with barium enemas and repeated colonoscopies to confirm resolution. There are risk factors, such as preoperative radiotherapy, which make resolution difficult. Complications may develop, including the formation of fistulas, periurethral fibrosis, infection of adjacent tissues and even malignant degeneration.
For the treatment of this condition, Whitlow et al.3 described unroofing of the anastomosis by means of the division of the wall between the presacral sinus and the lumen of the adjacent bowel. In another series,4 however, intersphincteric resection of the rectal stump together with debridement of the sinus and omentoplasty or muscular flap is presented as the technique with the best results for healing. The Endo-SPONGE® system introduced by Weidenhagen et al.,5 based on vacuum suction through a sponge that is inserted in the presacral space, showed a high rate of success, although a later study performed to evaluate these long-term results observed up to 25% of recurring abscesses.6 Another study compared EndoVAC® with rectal lavage and drainage, demonstrating that healing was significantly accelerated in the EndoVAC® group.7 When conservative treatment fails, “endoscopic stapled marsupialization” and endoscopic therapy with topical doxycycline injection are presented as effective alternatives.8 In the mid-1970s, the first endoscopic series were published of gastrointestinal fistula treatment using tissue adhesives (cyanoacrylate), which reported encouraging results.9
There is only one study published by Swain and Ellis10 with 7 patients where, as in this case, biological tissue adhesive was applied endoscopically for the treatment of a chronic presacral sinus after low anterior resection. As in our patient, their series reports healing of the sinus in all cases one week after the application of the treatment, and no cases of recurrence during 11 months of follow-up. This technique allowed for ileostomy closure 6–8 weeks after treatment.
Some authors postulate that this technique is only effective in cases with small cavities and tracts and is of little use in a large-cavity sinus with a small orifice. But the fact is that endoscopic treatment with biological tissue adhesive is a reliable, simple technique with low morbidity, low recurrence rate and high success rate. The limited number of cases published about this treatment method and the lack of comparative studies make it difficult for the technique to become standardized.
FundingNone.
AuthorshipStudy design, data collection, analysis and interpretation of the results and writing of the article were done by Víctor López and Jesús Abrisqueta. Juan Luján and Pascual Parrilla were involved in the process of study design, analysis and interpretation of the results, writing of the article, critical review and approval of the final version. Andrés Serrano was involved in the process of data collection, analysis and interpretation of the results.
Please cite this article as: López V, Abrisqueta J, Luján J, Serrano A, Parrilla P. Tratamiento endoscópico con pegamento tisular biológico del seno presacro crónico tras resección anterior baja. Cir Esp. 2015;93:197–199.
The following was presented as a poster at the 27th National Meeting of the Spanish Coloproctology Association in Madrid, May 14–16, 2014.