The patient was a healthy adolescent who suffered blunt abdominal trauma while skiing (direct impact of the abdomen against a post). He was brought to the emergency department of our hospital by ambulance.
On admission, the patient was hemodynamically stable (blood pressure: 110/70mmHg, HR: 80) with hemoglobin 12g/dl. He presented multiple abdominal erosions with signs of peritoneal irritation.
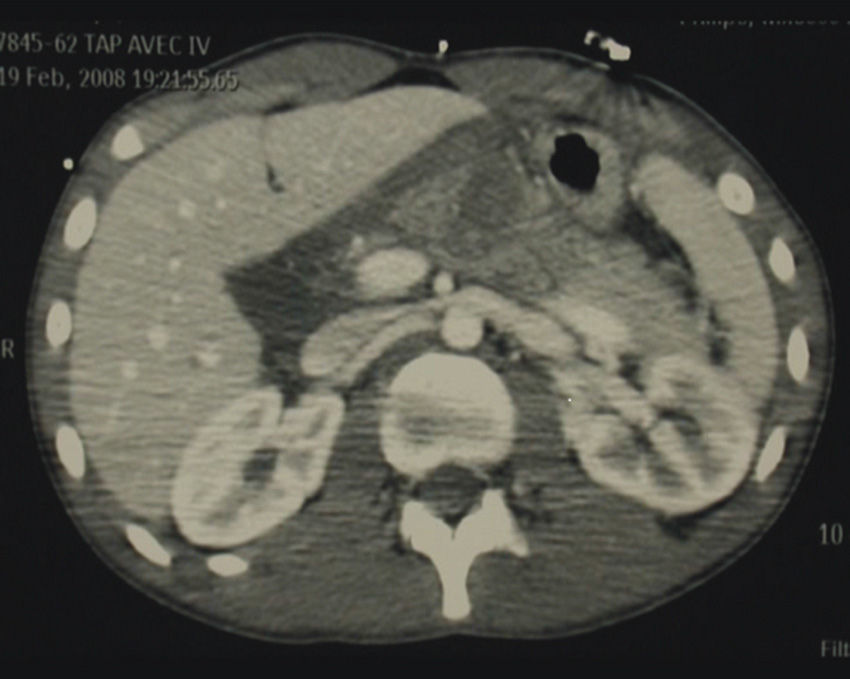
Abdominal CT scan showed an isolated pancreatic trauma injury (pancreatic hypodensity, enlarged pancreatic body and infiltration of peripancreatic fat), suspicious signs in a section of the pancreatic body and probable active arterial bleeding from the main pancreatic artery (Fig. 1).
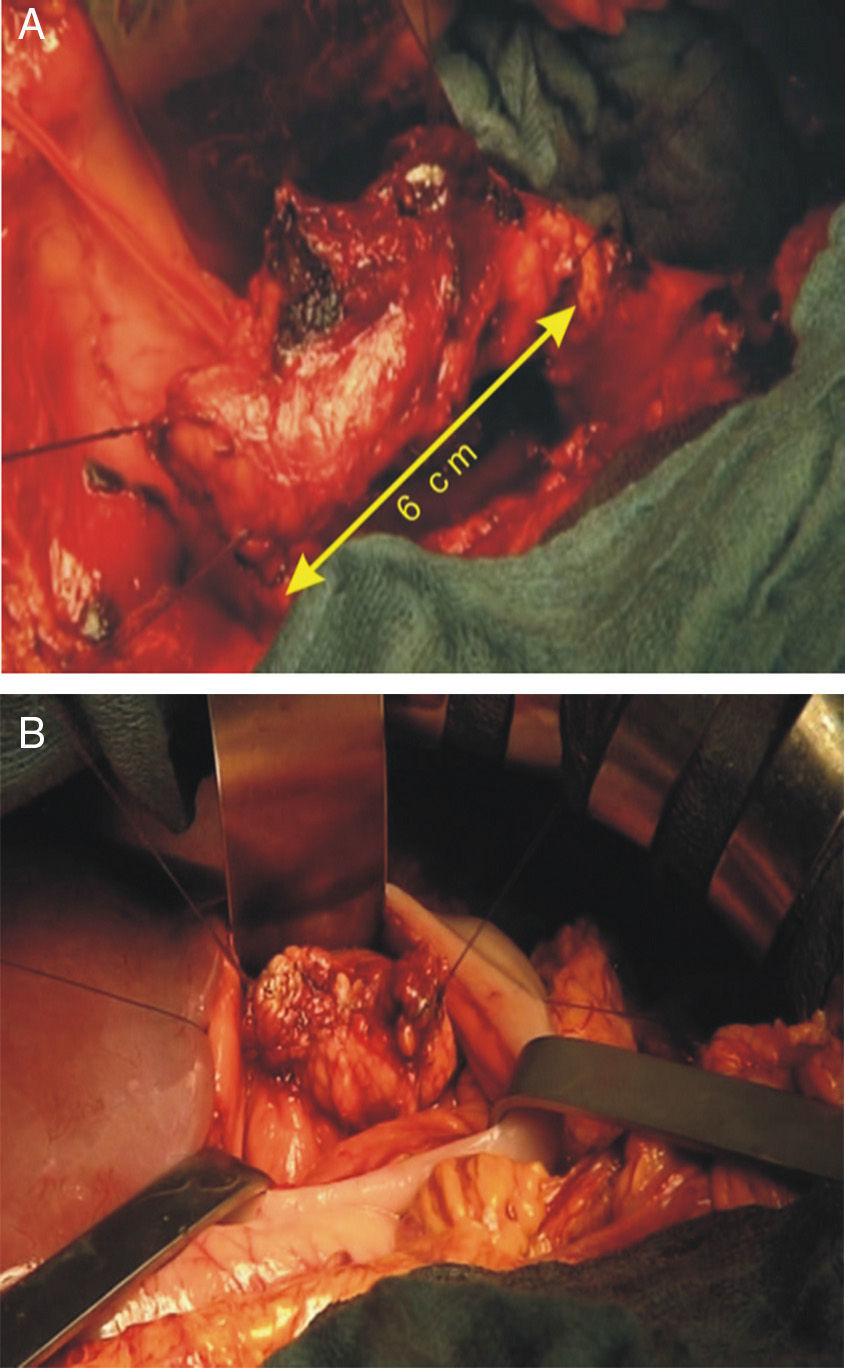
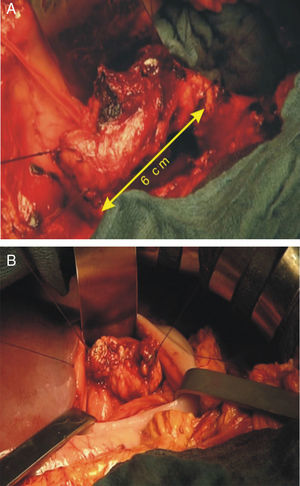
The patient underwent emergency laparotomy with bilateral subcostal incision. Abdominal exploration revealed: moderate hemoperitoneum and confirmation of the complete rupture of the duct of Wirsung at the pancreatic isthmus with arterial bleeding at the main pancreatic artery (Fig. 2A); the tail and body of the pancreas were also surrounded by a voluminous hematoma.
We initially achieved hemostasis by compression, followed by the identification and selective control of the hepatic and splenic arteries. Ultrasonic dissection (CUSA®) was used to resect the pancreatic region close to the portal vein with selective control of the duct of Wirsung at the head of the pancreas (Fig. 2B). Distal section of the area was macroscopically healthy.
Digestive continuity was reestablished by means of a pancreato-gastric end-to-side anastomosis with interrupted PDS 5–0 in 2 planes by invagination of the pancreatic stump in the gastric cavity, protected by omentoplasty. The proximal pancreas was protected with a TachoSil® sponge. Cholecystectomy was performed with external transcystic biliary drainage. The duration of the operation was 3h 20min, with no blood transfusion.
The patient presented good post-operative course. Oral uptake was reinitiated on the 7th day with no clinical or test signs of pancreatic fistula. Clinical-biological follow-up continued for 2 years after the intervention, with normal body growth and no signs of either diabetes or exocrine pancreatic failure.
In cases of blunt abdominal trauma, the pancreas is the most exposed of the retroperitoneal organs due to its anatomic position in front of the spinal column. Isolated pancreatic trauma in adolescents is rare (3%–12%).1,2 Frontal trauma (bicycle handles, blow to the epigastrium) can cause a fracture of the pancreas at the junction between the body and tail. The 2 main clinical–radiological elements that determine surgical treatment are: complete pancreatic duct rupture and the presence of active bleeding.
The American Association for Surgery of Trauma (AAST)3 classifies pancreatic injuries into 5 grades. According to most experts, this classification is a rational guideline of the selection of candidates for surgery, which is recommended in trauma injuries grades iii–v, particularly in cases with active bleeding.
Different surgical options have been proposed in cases of complete pancreatic duct rupture: splenopancreatectomy, caudal pancreatectomy with splenic preservation and fistulization directed by proximal drainage.4
Non-surgical treatment (parenteral nutrition, somatostatin analogs, papillotomy or endoscopic pancreatic prosthesis5) has been proposed in minor grade i and ii pancreatic trauma,6 while pancreatectomy is recommended for major grade iii and iv trauma.
Central pancreatectomy in an adolescent patient is unusual and has never been reported as emergency surgery. Fischer et al.7 published a case of central pancreatectomy in a 16-year-old teenager, in whom pancreatectomy was performed two months after trauma, which had initially been treated conservatively.
Most authors advocate left pancreatectomy with splenic preservation or exeresis8–10 in cases of pancreatic trauma with complete rupture of the pancreatic duct (grade iii).
Central pancreatectomy with pancreato-gastric anastomosis is a valid alternative. This type of surgery achieves preservation of the endocrine and exocrine function of the pancreas as well as the protective role of the spleen.
Central pancreatectomy (with pancreato-gastric anastomosis) in the emergency setting due to isolated trauma in an adolescent is possible, provided that the hemodynamic state is stable.
As we have reported in our case, after a 24-month follow-up, we can confirm good clinical tolerance and the absence of exocrine and endocrine pancreatic failure after surgery.7
This case is the first time a central pancreatectomy was performed in the emergency department on a teenager.
Please cite this article as: López Penza P, Rosso E, Marzano E, Oussoultzoglou E, Bachellier P. Pancreatectomía central de urgencia por traumatismo cerrado de abdomen. Cir Esp. 2013;91:545–546.