Incisional hernias are a frequent complication, and their prevention includes proper closure of the abdominal wall.
MethodsA prospective study was conducted at a third-level hospital after the introduction of a midline laparotomy closure protocol. An objective measurement of the suture length to incision length ratio was made, and the postoperative results were analyzed.
Results127 patients were included and 34 of them (26.8%) had received a technically deficient closure. Incisional hernia was described in 20.5% of cases. An improvement in the quality of the abdominal wall closure was demonstrated over time.
ConclusionThe abdominal wall closure was deficient in nearly one-quarter of the laparotomies performed at a third-level medical center. A protocol improved the quality of the laparotomy closure.
La hernia incisional es una patología altamente prevalente cuya prevención incluye medidas como el correcto cierre de la pared abdominal.
MétodosSe llevó a cabo un estudio prospectivo en un centro de tercer nivel que incluyó a pacientes intervenidos de modo electivo y de urgencias tras la implementación de un protocolo de cierre de la laparotomía media. Se realizó una medida objetiva de la relación entre la sutura usada y la longitud de la laparotomía y se analizaron los resultados postoperatorios.
ResultadosDe los 127 pacientes incluidos, 34 (26,8%) recibieron un cierre técnicamente deficiente. La incidencia de hernia incisional fue del 20,5%. Se demostró una mejoría progresiva en la calidad del cierre.
ConclusionesEl cierre de la pared abdominal es deficiente en cerca de una cuarta parte de las laparotomías realizadas en un centro de tercer nivel. La implementación de un protocolo de cierre mejora la calidad del mismo.
The prevalence of incisional hernias (IH) after midline laparotomy can reach 35%.1 In 1976, Jenkins established the basis for the closure of abdominal incisions, defining the minimum ratio of 4:1 between the length of the suture used and the length of the wound (SL:WL) as a basic parameter for quality.2 The data from the most current literature seem to indicate that an SL:WL>4:1 with continuous suture of slow-absorbing material reduces the IH rate.3 However, laparotomy closure remains controversial. A recent Cochrane review presents moderate-quality evidence showing the superiority of using absorbable and monofilament material, as well as very low evidence regarding other aspects, such as mass closure or the use of continuous suture.4 The “small bite” technique, with sutures that are close together and close to the midline (3–6mm), seems to increase the resistance of the tissues.5 Another recent systematic review in the context of elective surgery concludes that the small bite technique, which leads to an increase in SL:WL, is the technique of choice for laparotomy closure.6 The follow-up and implementation of specific clinical guidelines, particularly the recommendations of the European Hernia Society published after the start of this study, should potentially improve IH incidence results.7 In the context of emergencies, a prospective study after the implementation of a closure protocol demonstrated a reduction in IH compared to a historical cohort.8
Considering this context, there seems to be room for improvement in the midline laparotomy closure technique. According to an abdominal wall closure survey conducted in 2013 with 131 surgeons and residents, close to half of the respondents were unaware of or did not know how to apply the 4:1 technique.9 The objective measurement of the SL:WL ratio may be absent in standard daily practice. This would be the first step to detect factors that may be improved based on current knowledge. Developing a protocol for the basic surgical technique of laparotomy closure may be beneficial in reducing IH rates.
The main objective of this study was to prospectively and systematically analyze the midline laparotomy closure technique after the implementation of a closure protocol at a tertiary hospital, in the context of both urgent and elective surgery.
MethodsA prospective study was conducted over a period of 3 years, from October 2014 to October 2017, after the implementation of an abdominal wall closure protocol. The project and patient follow-up were approved by the Ethics Committee. The study included patients undergoing midline laparotomy, as well as assistance laparotomies in laparoscopic procedures, in the context of both emergency and elective surgeries. We excluded patients who had undergone other types of laparotomy, those who had a history of IH or who had midline IH at the time of surgery, and patients included in other abdominal wall studies. All patients gave their signed informed consent.
The closure technique was done in both groups under the same guidelines, in accordance with the conclusions of the INLINE10 systematic review and meta-analysis. These included single-layer closure with continuous slow-absorption polydioxanone sutures (2/0 PDS, Ethicon®). In addition, an SL:WL of at least 4:1 was established with the small bite technique. The technique had been recorded on video and shown to all participating surgeons, meaning the entire General Surgery department, including residents and assistant surgeons. No previous experimental training was conducted. The SL:WL ratio was systematically recorded after intraoperative measurement of both lengths in centimeters with a sterile malleable ruler, using the formula described by Israelsson.11
The anesthetic risk was recorded according to the scale of the American Society of Anesthesiologists.12 Factors related to the appearance of hernias were registered, such as diabetes, tobacco habit, constipation, chronic obstructive pulmonary disease, use of corticosteroids and immunosuppressants, aortic aneurysm pathology or previous history of midline laparotomies.13,14 The characteristics of the surgical procedure were also recorded according to whether they were urgent or elective and the reason for the intervention (colon, small intestine, gastric or other pathology). The degree of contamination was described according to the description of the Centers for Disease Control and Prevention, defining the surgery as clean, clean-contaminated, contaminated or dirty.15 Other recorded data included the use of prophylactic antibiotic therapy, wall retention measures (total points) and closure by the attending surgeon or resident, without specifying the year of residence.
Immediate postoperative complications were recorded, including wound infection according to the criteria of the Centers for Disease Control and Prevention, evisceration, hematoma and reoperation during the first 30 days after surgery.16 Perioperative pain was also recorded, as defined by the visual analogue scale.17
The appearance of IH was assessed by physical examination 3 and 6 months after surgery, as well as a radiological evaluation by computed tomography (CT) at the 6-month follow-up visit; IH was considered an early complication of surgery.18 The presence of neoplastic pathology made it possible to adapt this control to the scheduled follow-up of the baseline pathology in the majority of patients. The diagnosis of IH was defined as the presence of a palpable mass under the surgical scar after Valsalva maneuvers on physical examination and an interruption between the abdominal rectus muscles on CT.
We analyzed the results from the total patient sample as well as the results from the following subgroups: patients operated on in the emergency department, patients who underwent elective surgery, patients with an SL:WL<4:1 (considered technically deficient) and patients with an SL:WL≥4:1. We also calculated the number of patients who did not comply with the SL:WL associated with the short bite technique (SL:WL 5:1).
Statistical AnalysisIn the statistical analysis and the bivariate and multiple comparisons, the Chi-squared, ANOVA and Scheffé tests were used, establishing statistical significance as a P value <.05 value. IBM SPSS statistics version 2.0 software for Mac was used.
ResultsA total of 127 patients who underwent midline laparotomy in the study period met the inclusion criteria.
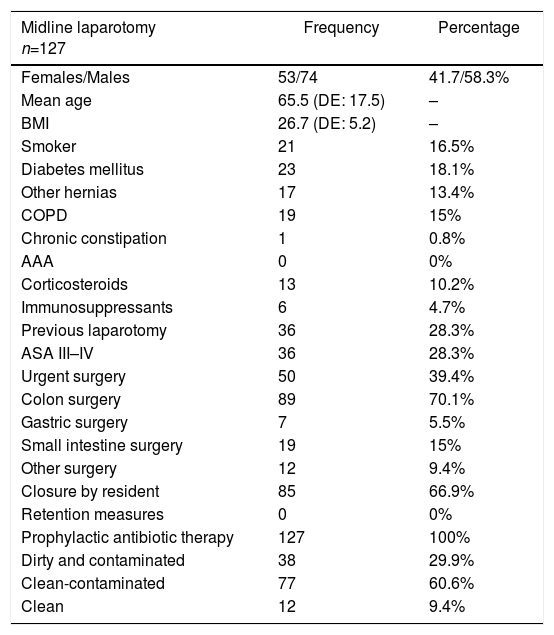
In the analysis of the total sample, 17 patients (13.4%) had a history of hernia pathology outside the midline and 36 (28.3%) had previously undergone midline laparotomy. Laparotomy was performed in an emergency context in 50 patients (39.4%), and in 89 cases the reason was colon pathology (70.1%). Thirty-eight patients (29.9%) were treated in a situation of dirty or contaminated surgery. The demographic and surgical characteristics of the sample are shown in Table 1.
Demographic and Surgical Characteristics of the Patients With Midline Laparotomy.
| Midline laparotomy n=127 | Frequency | Percentage |
|---|---|---|
| Females/Males | 53/74 | 41.7/58.3% |
| Mean age | 65.5 (DE: 17.5) | – |
| BMI | 26.7 (DE: 5.2) | – |
| Smoker | 21 | 16.5% |
| Diabetes mellitus | 23 | 18.1% |
| Other hernias | 17 | 13.4% |
| COPD | 19 | 15% |
| Chronic constipation | 1 | 0.8% |
| AAA | 0 | 0% |
| Corticosteroids | 13 | 10.2% |
| Immunosuppressants | 6 | 4.7% |
| Previous laparotomy | 36 | 28.3% |
| ASA III–IV | 36 | 28.3% |
| Urgent surgery | 50 | 39.4% |
| Colon surgery | 89 | 70.1% |
| Gastric surgery | 7 | 5.5% |
| Small intestine surgery | 19 | 15% |
| Other surgery | 12 | 9.4% |
| Closure by resident | 85 | 66.9% |
| Retention measures | 0 | 0% |
| Prophylactic antibiotic therapy | 127 | 100% |
| Dirty and contaminated | 38 | 29.9% |
| Clean-contaminated | 77 | 60.6% |
| Clean | 12 | 9.4% |
ASA: American Society of Anesthesiologists; SD: standard deviation; COPD: chronic obstructive pulmonary disease; BMI: body mass index.
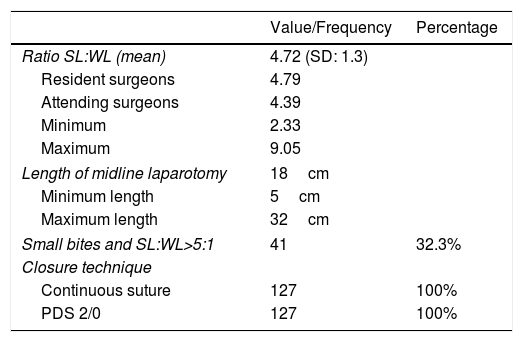
In 85 cases (66.9%), the laparotomy was closed by the resident surgeon. The mean SL:WL ratio was 4.7:1. Both attending surgeons and residents closed with an average SL:WL ratio>4:1. The average size of the incision was 18.1cm, with a minimum of 5cm and a maximum of 32cm.
Table 2 shows the context in which the abdominal wall was closed and its characteristics.
Laparotomy Closure Technique.
| Value/Frequency | Percentage | |
|---|---|---|
| Ratio SL:WL (mean) | 4.72 (SD: 1.3) | |
| Resident surgeons | 4.79 | |
| Attending surgeons | 4.39 | |
| Minimum | 2.33 | |
| Maximum | 9.05 | |
| Length of midline laparotomy | 18cm | |
| Minimum length | 5cm | |
| Maximum length | 32cm | |
| Small bites and SL:WL>5:1 | 41 | 32.3% |
| Closure technique | ||
| Continuous suture | 127 | 100% |
| PDS 2/0 | 127 | 100% |
SD: standard deviation; SL:WL ratio: ratio between suture length and incision length.
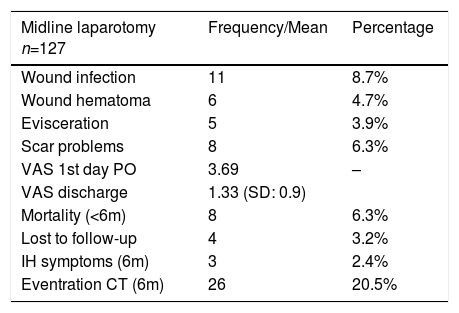
The 6-month IH rate diagnosed by CT was 20.5%, while only 3 patients (2.4%) had a clinically detectable IH. An intention-to-treat analysis was completed. There were 8 patients who died during the first 6 postoperative months (6.3%) and 4 patients who were lost to follow-up (3.2%). Postoperative morbidity is shown in Table 3.
Postoperative Results.
| Midline laparotomy n=127 | Frequency/Mean | Percentage |
|---|---|---|
| Wound infection | 11 | 8.7% |
| Wound hematoma | 6 | 4.7% |
| Evisceration | 5 | 3.9% |
| Scar problems | 8 | 6.3% |
| VAS 1st day PO | 3.69 | – |
| VAS discharge | 1.33 (SD: 0.9) | |
| Mortality (<6m) | 8 | 6.3% |
| Lost to follow-up | 4 | 3.2% |
| IH symptoms (6m) | 3 | 2.4% |
| Eventration CT (6m) | 26 | 20.5% |
SD: standard deviation; VAS: visual analogue scale; IH: incisional hernia; PO: postoperative; CT: computed tomography.
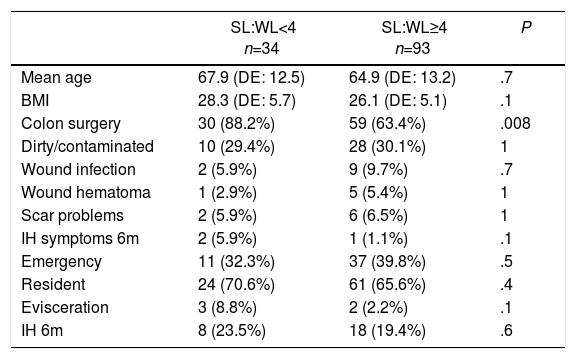
Closure was done in 34 patients (26.8% of the sample) with an SL:WL<4:1. The IH rate diagnosed by CT 6 months later was 23.5% in this group, compared to 19.4% in the group of patients with a ratio equal to or greater than 4:1, which was not statistically significant (P=.3). Two of the 5 eviscerations of the total sample occurred in the group with a technically deficient closure, representing 5.9% of the cases, with no observed statistically significant difference (P=.4). The comparison according to the technical quality of the closure is shown in Table 4.
Comparison According to Quality of Laparotomy Closure.
| SL:WL<4 n=34 | SL:WL≥4 n=93 | P | |
|---|---|---|---|
| Mean age | 67.9 (DE: 12.5) | 64.9 (DE: 13.2) | .7 |
| BMI | 28.3 (DE: 5.7) | 26.1 (DE: 5.1) | .1 |
| Colon surgery | 30 (88.2%) | 59 (63.4%) | .008 |
| Dirty/contaminated | 10 (29.4%) | 28 (30.1%) | 1 |
| Wound infection | 2 (5.9%) | 9 (9.7%) | .7 |
| Wound hematoma | 1 (2.9%) | 5 (5.4%) | 1 |
| Scar problems | 2 (5.9%) | 6 (6.5%) | 1 |
| IH symptoms 6m | 2 (5.9%) | 1 (1.1%) | .1 |
| Emergency | 11 (32.3%) | 37 (39.8%) | .5 |
| Resident | 24 (70.6%) | 61 (65.6%) | .4 |
| Evisceration | 3 (8.8%) | 2 (2.2%) | .1 |
| IH 6m | 8 (23.5%) | 18 (19.4%) | .6 |
SD: standard deviation; IH: incisional hernia; BMI: body mass index; SL:WL: ratio between length of suture used and length of the incision.
The small bite closure technique with an associated SL:WL rate ≥5:1 was only fulfilled in 41 of the cases reviewed (32.3%).
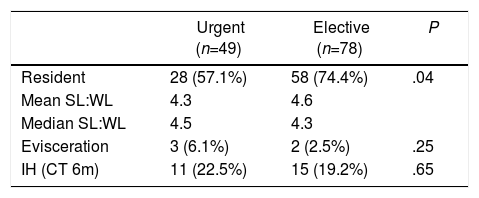
Results were compared between patients who were operated on in an emergency situation and those who underwent elective surgery. In the emergency context, a lower percentage of laparotomies were closed by residents (57.1%) compared to the proportion found in elective surgeries, which was statistically significant (P=.04). In both groups, the mean value and the median SL:WL was higher than 4:1. The incisional hernia rate diagnosed radiologically at the 6-month follow-up was higher in the emergency group (22.5%), as was the rate of evisceration (6.1%), although no statistically significant differences were found (Table 5).
Comparison of Laparotomy Closure According to Urgent or Elective Surgery.
| Urgent (n=49) | Elective (n=78) | P | |
|---|---|---|---|
| Resident | 28 (57.1%) | 58 (74.4%) | .04 |
| Mean SL:WL | 4.3 | 4.6 | |
| Median SL:WL | 4.5 | 4.3 | |
| Evisceration | 3 (6.1%) | 2 (2.5%) | .25 |
| IH (CT 6m) | 11 (22.5%) | 15 (19.2%) | .65 |
IH: incisional hernia; SL:WL: ratio between length of suture used and incision length.
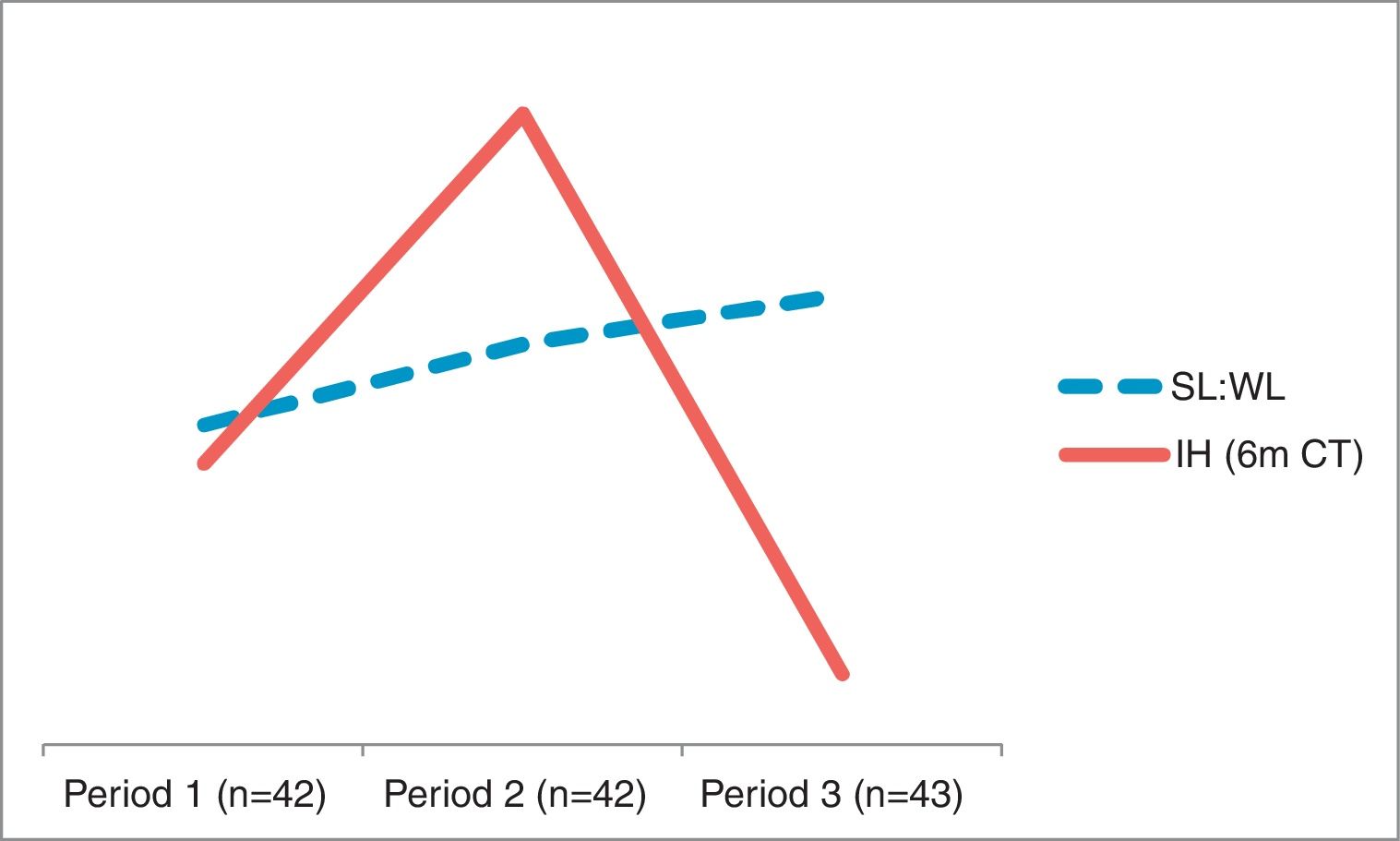
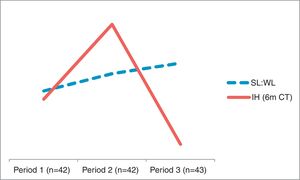
The mean SL:WL increased over the course of the study period. The chronological division into 3 time periods within the study provided SL:WL ratios of 4.28, 4.86 and 5.21, respectively. The last period studied had a significantly higher average ratio (P=.027) compared to the first. In this period, a lower IH rate was observed (11.6%), which was below the observed global rate, with no statistical significance (P=.07). The results over time in the study period are shown in Fig. 1.
DiscussionIn the literature, an SL:WL ratio ≥4:1 has been reported to be advantageous for the closure of midline laparotomies.19 The technical variability in the closure method, lack of knowledge about the 4:1 technique, clinical difficulties in emergency situations and little importance given mainly to the closure of laparotomies may all alter the closure technique.20
Although IH are a consequence of several factors, technique is the only factor that depends exclusively on the surgeon.21 In a resident training program on abdominal wall closure techniques, a progressive improvement in technical skills was observed, as well as an initial lack of knowledge of the optimal relationship between suture length and incision length.22 it is necessary to homogenize the closure technique and systematically calculate the SL:WL ratio to assess the quality of the closure.23 Our results show a progressive technical improvement in the closure of the abdominal wall throughout the study, with a lower IH rate in the last period of the study.
According to our study, the closure of laparotomies falls to a large extent on residents, especially in the context of elective surgery. In a review of 100 consecutive patients, the SL:WL ratio was calculated, which was equal to or greater than 4:1 in 76% of cases. The ratio below 4:1 was more frequent in closures performed by residents and was associated with a higher rate of wound infection.24 In our sample, the average SL:WL ratio for both adjunct surgeons and residents is slightly higher than 4:1 and lower than 5:1. Only systematic measurement and calculation of this ratio can guarantee a technically correct closure.
A technically deficient closure (SL:WL<4:1) could be the cause of a higher IH rate. In this review, the results show 26.8% of patients with closures that could be considered incorrect due to not meeting the technical requirements. Although a higher IH rate was observed in this group of patients and in the patients with emergency procedures, these differences were not statistically significant. A greater participation of residents was observed in this subgroup, although this was not a statistically significant difference.
A greater proportion of patients treated for colon pathologies was found among the technically deficient closures (88.2 versus 63.4%), although the proportion of contaminated and dirty surgery in both groups was homogeneous. Colon surgery, due to its higher rate of surgical site infection compared to clean surgeries, presents a greater risk for IH.25 For this reason, closure in these patients should be especially meticulous.
A prospective study that included 560 randomized patients demonstrated a lower rate of IH in elective midline laparotomies after closure with the small bite technique associated with a mean SL:WL ratio of 5:1.26 Of the total number of patients studied in our sample, 86 did not receive a closure that met these requirements.
The present study shows 2 fundamental limitations: a limited sample size and a short follow-up. The limited sample was due to the exclusion of patients participating in other studies. However, it is an easily reproducible study that provides essential information about the technical quality of routine abdominal wall closure, both in an urgent and elective context.
Although the present study has a limited number of patients, it demonstrates a technical improvement in the closure of laparotomies after the establishment of a closure protocol and systematic collection of SL:WL data. However, no statistically significant differences were found in the presence of eviscerations, wound infections or in the appearance of IH based on this factor.
Although detection of IH can be done early on with CT, a higher rate of symptomatic and detectable IH can be expected on physical examination with follow-ups longer than 6 months.
The closure technique was deficient in one-quarter of midline laparotomies performed at a tertiary medical center as emergency or elective surgery. This proportion reached 70% when the small bite technique with an SL:WL ratio>5:1 was used as a reference, which is supported by current evidence in elective surgery.
The implementation of a closure protocol significantly improves technical results.
Both resident surgeons and adjunct surgeons are able to perform technically correct closures after proper training.
Resident surgeons are most involved in the closure of laparotomies, both in the context of emergency and elective surgeries.
Among the technically deficient closures, a higher rate of colon surgery is observed, with special attention being paid to this patient subgroup.
A greater number of patients is required to evaluate the impact of this technical improvement on the appearance of IH, as well as a longer-term follow-up.
The preventive effect of prophylactic mesh for the reduction of IH should be assessed, which was not done in this study as it was not among the objectives.
FundingNo funding was received for the completion of this study.
Conflict of InterestsThe authors have no conflict of interests to declare.
Special thanks to Dr. López-Cano and Dr. Sánchez for their personal dedication and wise advice.
Please cite this article as: Valverde S, SánchezLuis JL, Pereira JA, Armengol M, López-Cano M. Cierre de la laparotomía electiva y urgente. Importancia de protocolizar la técnica. Cir Esp. 2019;97:97–102.