Find out the long-term economic cost associated with the treatment of severe fecal incontinence by SNS versus symptomatic conservative treatment and definitive colostomy.
MethodsDetailed descriptive study of the costs of the healthcare process (interventions, consultations, devices, complementary tests, hospitalization, etc.) of 3 treatment alternatives for fecal incontinence using analytical accounting tools of the Health Service based on clinical activity data. The frequency of use of health resources or the quantity of products dispensed in pharmacies (medication, diapers, ostomy material, etc.) was estimated in each case. Costs derived from adverse situations were included. Patients with severe fecal incontinence, defined by a score greater than 9 on the Wexner severity scale, in whom first-line treatments had failed, were included.
Data from a consecutive cohort of 93 patients who underwent an SNS between 2002 and 2016 were used; patients who underwent definitive colostomy (n=2); parastomal hernia (n=3); and colostomy stenosis (n=1).
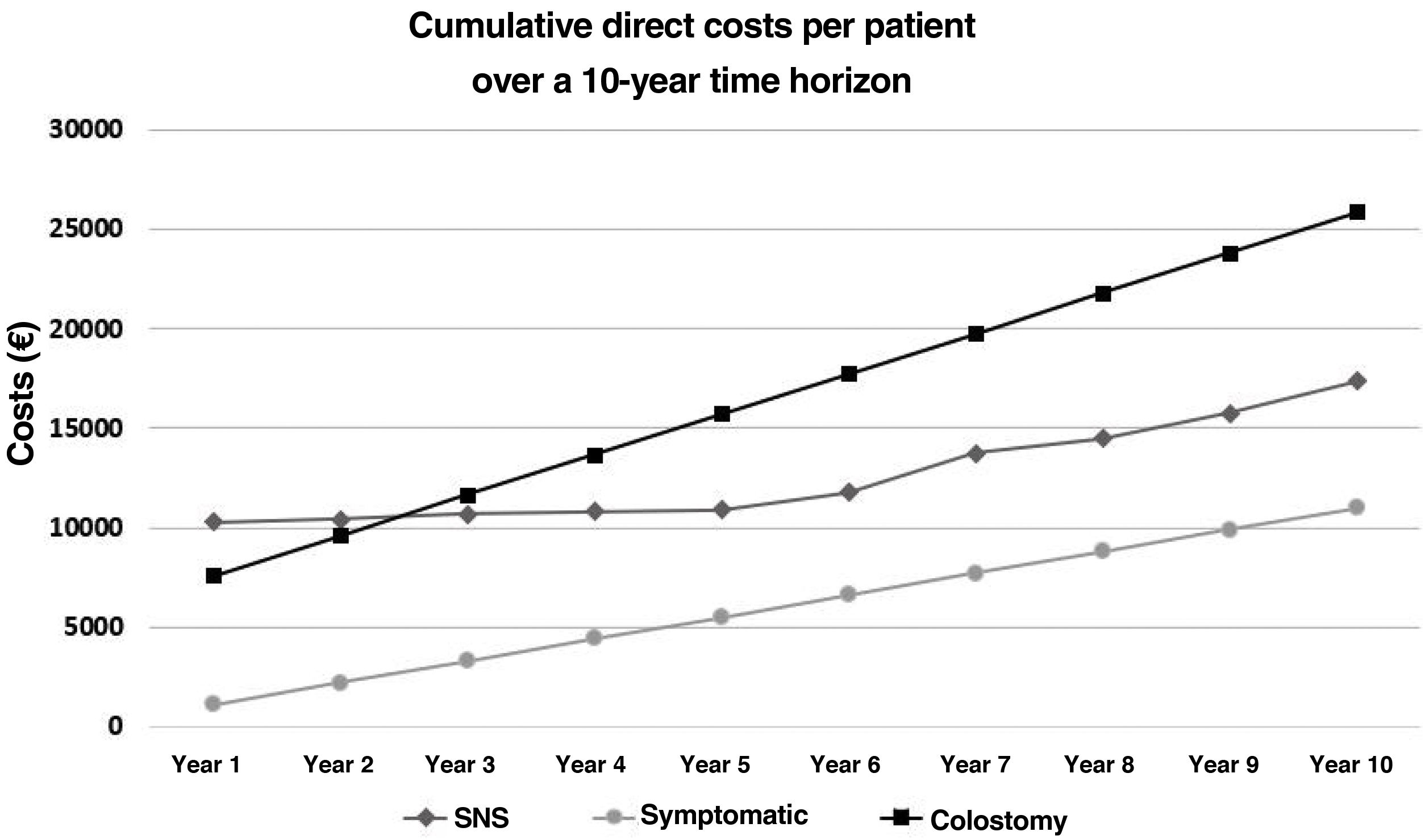
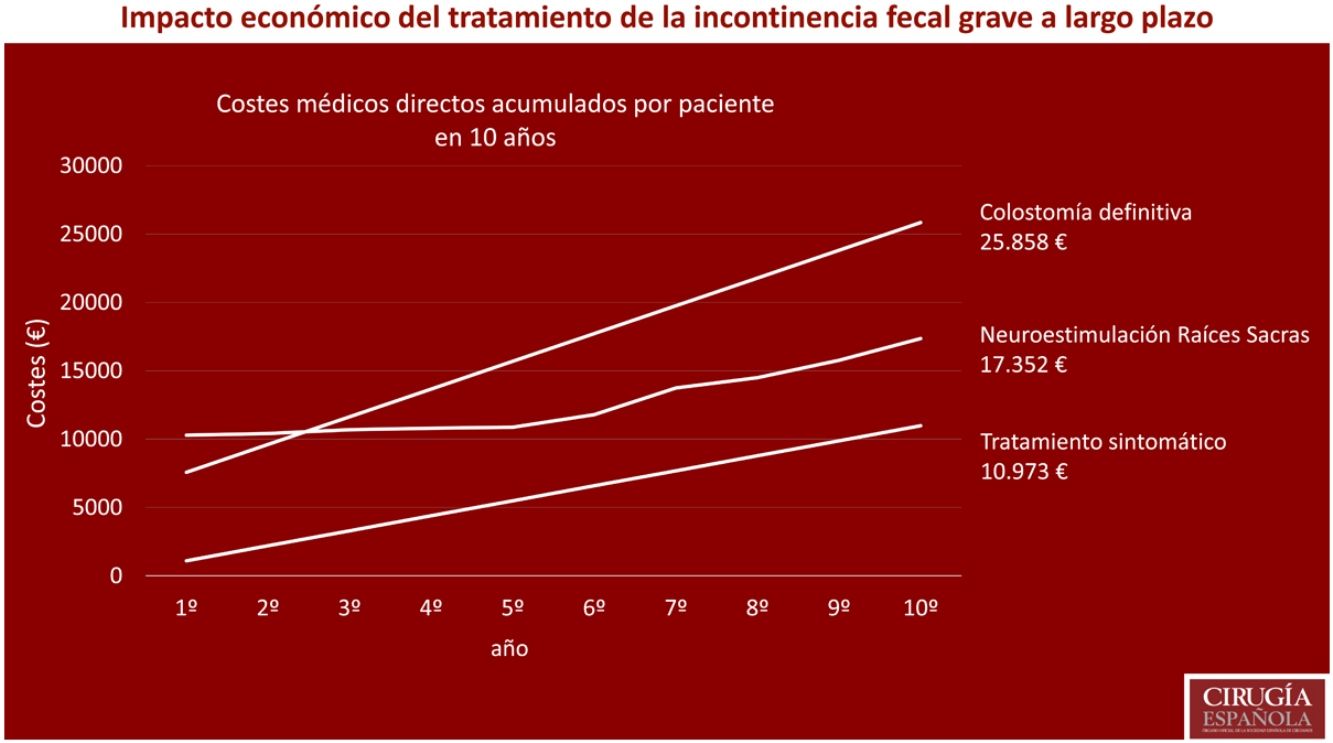
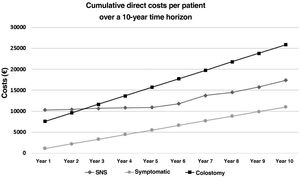
ResultsThe mean cumulative cost in 10 years per patient in each alternative was: € 10,972.9 symptomatic treatment (62% diapers); € 17,351.57 SNS (95.83% interventions; 81.6% devices); € 25,858.54 definitive colostomy (70.4% ostomy material and accessories).
ConclusionsManagement of severe fecal incontinence implies a great burden in economic terms. The colostomy is the alternative that generates the most direct cost, followed by SNS and symptomatic treatment.
Conocer el coste económico a largo plazo asociado al tratamiento de la incontinencia fecal grave mediante SNS frente al tratamiento conservador sintomático y la colostomía definitiva.
MétodoEstudio descriptivo pormenorizado de los costes del proceso asistencial (intervenciones, consultas, dispositivos, pruebas complementarias, hospitalización, etc.) de 3 alternativas de tratamiento de la incontinencia fecal empleando herramientas de gestión y contabilidad analítica del propio Servicio de Salud basadose en datos de actividad clínica. Se estimó, en cada caso, la frecuencia de uso de recursos sanitarios o la cantidad de productos dispensados en farmacias (medicación, pañales, material de ostomía, etc.). Se incluyeron costes derivados de situaciones adversas. Se incluyeron pacientes con incontinencia fecal grave, definida por una puntación superior a 9 en la escala de severidad de Wexner, en los que ha fracasado los tratamientos de primera línea. Se emplearon datos de una cohorte consecutiva de 93 pacientes a la que se realizó una SNS entre los años 2002 y 2016; de pacientes intervenidos de colostomía definitiva (n=2); hernia paraestomal (n=3); y estenosis de colostomía (n=1).
ResultadosEl coste medio acumulado en 10 años por paciente en cada alternativa fue: 10972,9 € tratamiento sintomático (62% pañales); 17.351,57 € para la SNS (95,83% intervenciones; 81.6% dispositivos); y 25.858,54 € para la colostomía definitiva (70.4% material de ostomía).
ConclusionesEl manejo de la incontinencia fecal grave implica un gran impacto en términos económicos. La colostomía es la alternativa que más costes directos genera, seguido de la SNS y el tratamiento sintomático.
Health systems have limited resources to face the challenge of managing healthcare delivery.1 There are direct costs, related to prevention, diagnosis, treatment, follow-up, and care; and indirect costs, primarily related to lost productivity due to illness.2
With the current ageing population, the prevalence of faecal incontinence is expected to rise, and with it, the burden and economic impact on healthcare systems and society.
First-line treatment includes dietary changes, drugs and/or biofeedback, and surgical interventions (sphincteroplasty). If these fail, alternatives may be considered: sacral root neurostimulation (SNS), definitive colostomy or symptomatic conservative management (drugs, incontinence pads, etc.).
The aim of this study is to determine the long-term economic cost associated with the treatment of faecal incontinence using SNS versus symptomatic conservative management and definitive colostomy.
MethodsA descriptive study of the care process costs of 3 alternatives to treat faecal incontinence from a global perspective; we did not determine those bearing the costs, which in some cases will be the patient themselves and in others the Health Service. Data on clinical activity were provided to the Cost Control and Analysis Service of the Navarra Health Service, who individually assigned the direct medical costs (interventions, consultations, devices, complementary tests, hospitalisation, etc.). An average estimate was made of the frequency of use of health resources, or the quantity of products dispensed in pharmacies (medication, nappies, ostomy material, etc.), the costs of which were obtained from the Ministry of Health and Consumer Affairs, using 2018 rates.
The inclusion criteria were patients with severe incontinence, defined by a score of more than 9 on the Wexner severity scale,3,4 regardless of aetiology, and in whom conservative (biofeedback, pharmacological) or surgical (sphincteroplasty) treatment had failed.
A situation of permanent severe faecal incontinence was assumed in the evaluation of the costs of symptomatic treatment, and indirect costs were obtained from the medical literature.2 The study of the cost of SNS treatment used data from a consecutive cohort of 93 patients undergoing SNS between 2002 and 2016.5 Finally, costs were obtained for patients undergoing elective incontinence surgery for definitive colostomy (n=2), parastomal hernia (n=3), and colostomy stricture (n=1).
This is a descriptive study. Therefore, no inferential statistical methodology was applied to compare the groups. There was no hypothesis testing, nor was the sample size calculated to obtain statistical power.
Microsoft Excel and Tableau Reader software were used for data management and calculations.
ResultsSymptomatic treatmentIn our setting, we estimate that patients with severe faecal incontinence use 3 products for daytime use/day (€481.8/year) and 1 product for night-time use/day (€197.1/year), with an average cost in nappies of €678.9/patient-year.
Other protective pads, such as under pads, are often used, an estimated one every 3–4 days, at an average cost of €40/patient-year.
There are other devices, such as anal obturators or transanal irrigators, but as they are used by a minority they have not been included.
In addition to dietary changes, medication (faecal bolus-forming laxatives, antidiarrhoeals) is often recommended in guidelines based on experience and expert opinion.6 It was estimated that a patient with severe incontinence takes on average one loperamide tablet/day (€189.8/year) and one sachet of Plantago Ovata (€40.15/year), at an average cost of €229.95/patient-year.
Twelve consultations/year in primary care were estimated: 5 medical (€14.07/consultation), 5 nursing (€12.91/consultation), and 2 non-face-to-face (€6.77/consultation), with an average cost of €148.44/patient-year.
The average cost of symptomatic treatment of severe faecal incontinence in our study was €1,097.29/patient-year (€10,972.9 over 10 years). Sixty-two percent was for nappies, 21% for medication, 13% for consultations in primary care, and 4% for other incontinence pads. (Table 1).
Direct medical costs of symptomatic treatment.
| Cost/unit (€) | Total costs (€)/year | |
|---|---|---|
| Nappies | 678.9 (61.87%) | |
| Daytime use (600−900ml) (n=1095) | .44 | 481.8 |
| Rectangular night | .37 | |
| Anatomical day | .38 | |
| Anatomical night | .54 | |
| Elastic anatomical day | .39 | |
| Elastic anatomical night | .54 | |
| Night-time use (900–1200ml) (n=365) | .54 | 197.1 |
| Rectangular night | .37 | |
| Rectangular super night | .51 | |
| Anatomical night | .54 | |
| Anatomical super night | .63 | |
| Elastic anatomical night | .54 | |
| Elastic anatomical super night | .63 | |
| Other pads (n=100) | .4 | 40 (3.64%) |
| Medication | 229.95 (20.96%) | |
| Loperamide (n=365) | .52 | 189.8 |
| Plantago Ovata (n=365) | .11 | 40.15 |
| Healthcare | 148.44 (13.53%) | |
| Medical face-to-face (n=5) (7.8min) | 14.07 | 70.35 |
| Medical non-face-to-face (n=2) (3.75min) | 6.77 | 13.54 |
| Nursing (n=5) (7.24min) | 12.91 | 64.55 |
| Average annual cost, € | 1097.29 | |
| Indirect costs of faecal incontinence | ||
| Loss of productivity (source: Deutekom et al.2and Xu et al.9). | 1,200 |
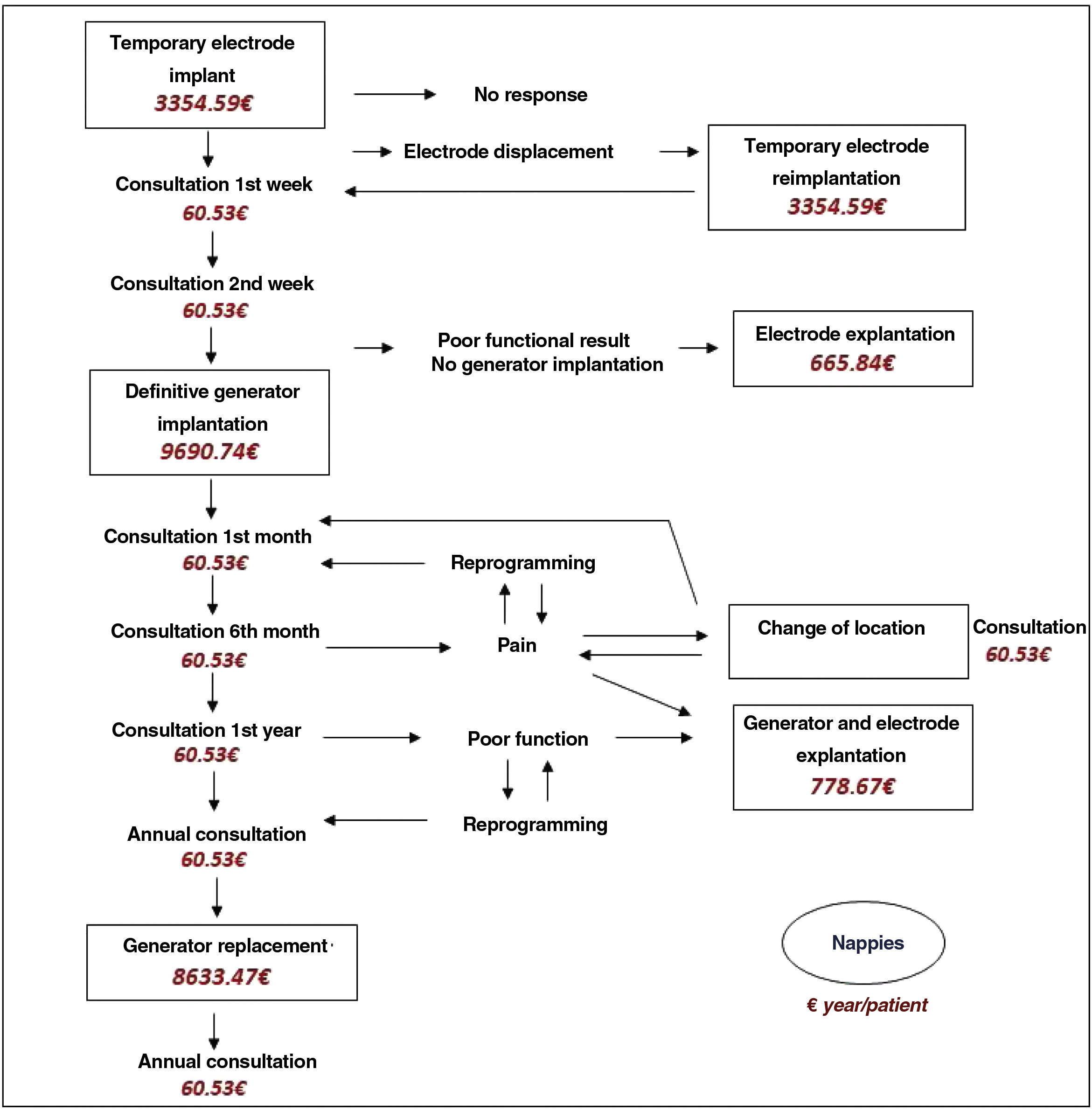
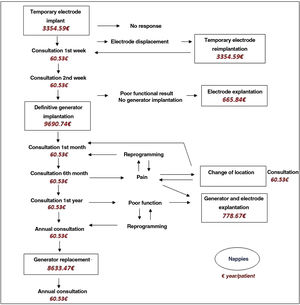
Typical interventions include electrode implantation, definitive generator implantation, and generator replacement. The cost of interventions secondary to adverse events, such as electrode displacement, pain, or poor functional results, was considered. The usual consultation pathway includes a visit in the first and second week after electrode implantation, the first and sixth month after generator implantation, at one year and annual consultations thereafter (Fig. 1).
Nappies are used in a minority of these patients, regular use estimated in 10% (one nappy/day), and sporadic use in 20% (one nappy/week).
The total direct medical costs for SNS of the 93 patients with a mean follow-up of 78.1 months (SD 35.4; range 1–161) amounted to €1,153,816.01. The cost of the interventions accounted for 95.83% (81.6% in devices), and definitive generator implantation was the costliest of the total (53.5%), followed by electrode implantation (28.2%), and generator replacement (14.1%). A breakdown of all costs is shown in Table 2.
Direct medical costs of sacral nerve stimulation.
| Routine interventions | ||
|---|---|---|
| Intervention | Individual costs (€) | Total costs (€) |
| Temporary electrode implant (n=93) | 3354.59 | 311,976.87 (27.04%) |
| Operating theatre costs (68min) | ||
| Prosthesis | ||
| SNS electrode | 1,948.7 | 181,229.1 |
| Percutaneous approach kit | 273.22 | 25,409.46 |
| Surgeon | 99.55 | 9,258.15 |
| Anaesthetist | 92.87 | 8,636.91 |
| Nursing and other costs | 805.8 | 74,939.4 |
| UCMA (Major outpatient surgery unit) (201min) | 134.45 | 12,503.85 |
| Definitive generator implant (n=61) | 9690.74 | 591,135.1 (51.23%) |
|---|---|---|
| Operating theatre costs (44min) | ||
| Prosthesis | ||
| Generator | 7,840.27 | 478,256.47 |
| Programmer | 1,067.4 | 65,111.4 |
| Surgeon | 51.14 | 3,119.54 |
| Anaesthesia | 68.51 | 4,179.11 |
| Nursing and other costs | 547.84 | 33,418.24 |
| UCMA (155min) | 115.58 | 7,050.38 |
| Generator replacement (n=18) | 8633.47 | 155,402.46 (13.47%) |
|---|---|---|
| Operating theatre costs (44min) | ||
| Prosthesis | ||
| Generator | 7,840.27 | 141,124.86 |
| Surgeon | 44.19 | 795.42 |
| Anaesthetist | 67.2 | 1,209.6 |
| Nursing and other costs | 571.42 | 10,285.56 |
| UCMA (154min) | 110.39 | 1,987.02 |
| Adverse event interventions | ||
|---|---|---|
| Intervention | Individual costs (€) | Total costs (€) |
| Electrode explantation (n=29) | 665.84 | 19,309.36 (1.67%) |
| Operating theatre costs (38min) | ||
| Surgeon | 54.74 | 1,587.46 |
| Anaesthetist | 57.08 | 1,655.32 |
| Nursing and other costs | 458.16 | 13,286.64 |
| UCMA (153min) | 95.86 | 2,779.94 |
| Electrode implantation (n=3) | 3354.59 | 10,063.77 (.87%) |
|---|---|---|
| Operating theatre costs (68min) | ||
| Prosthesis | ||
| SNS electrode | 1,948.7 | 5,846.1 |
| Percutaneous approach kit | 273.22 | 819.66 |
| Surgeon | 99.55 | 298.65 |
| Anaesthetist | 92.87 | 278.61 |
| Nursing and other costs | 805.8 | 2,417.4 |
| UCMA (201min) | 134.45 | 403.35 |
| Change of generator location (n=7) | 1548.58 | 10,840.06 (.94%) |
|---|---|---|
| Operating theatre costs (53min) | ||
| Prosthesis | ||
| Extension cable | 564.86 | 3,954.02 |
| Surgeon | 82.46 | 577.22 |
| Anaesthetist | 89.66 | 627.62 |
| Nursing and other costs | 737.5 | 5,162.5 |
| UCMA (110min) | 74.1 | 518.7 |
| Generator and electrode explantation (n=9) | 778.67 | 7008.03 (.61%) |
|---|---|---|
| Operating theatre costs(38min) | ||
| Surgeon | 51.01 | 459.09 |
| Anaesthetist | 55.87 | 502.83 |
| Nursing and other costs | 481.14 | 4,330.26 |
| UCMA (315min) | 190.65 | 1,715.85 |
| Surgeon consultation (n=690) | 60.53 | 41,765.7 (3.62%) |
|---|---|---|
| Nappies (n=17,540.6) | .36 | 6,314.62 (.55%) |
| Daytime rectangular | .37 | |
| Daytime anatomical | .32 | |
| Daytime elastic anatomical | .39 | |
| Total sample costs, € | 1153.816.01 |
Over 10 years, in an ideal scenario without adverse situations, the cost would be €13,832.22, to which should be added €8633.47 for generator replacement at around 7–8 years, totalling €22,465.69. The average cost would be €2246.57/patient-year. From the data from our series, over 10 years the average cumulative cost was €17,351.57/patient, and €16,831.10/patient without taking complications into account.
Definitive colostomyThe costs for admission and consultations, in the absence of complications, were €7586.11 in the first year, and subsequently €2030.27/patient/year. The cost of €5071.2/patient for admission and intervention and the annual cost of ostomy material of €1820.3/patient are striking. Patients can use irrigation systems to regulate and delay bowel movements; the average cost of both options has been estimated (Table 3).
Direct medical costs of definitive colostomy.
| First year costs | ||
|---|---|---|
| Procedures | Cost/unit (€) | Total costs (€) |
| Preoperative study | 206.41 (2.72%) | |
| Electrocardiogram | 31 | 31 |
| Chest X-ray | 20.58 | 20.58 |
| Blood test | 154.83 | 154.83 |
| Admission and complication-free intervention | 5071.2 (66.85%) | |
|---|---|---|
| Hospital ward | ||
| Stay (58 days) | 257.26 | 1,492.1 |
| Visits to surgeon (7.5) | 46.96 | 352.2 |
| Operating theatre (200min) | ||
| Surgeon | 240 | 240 |
| Anaesthetist | 307.1 | 307.1 |
| Nursing and other costs | 2391.7 | 2391.7 |
| Other | ||
| Laboratory, radiology, URPA (Post Anaesthesia Recovery Unit), drugs | 116 | 116 |
| Consultations | 488.2 (6.43%) | |
|---|---|---|
| Specialist care | ||
| Doctor (14.6min) (n=2) | 60.53 | 121.06 |
| Stomatherapist (33.2min) (n=6) | 52.39 | 314.34 |
| Primary care | ||
| Doctor face-to-face (7.8min) (n=1) | 14.07 | 14.07 |
| Nursing (7.24min) (n=3) | 12.91 | 38.73 |
| Routine ostomy material | 1708.14 (22.52%) | |
|---|---|---|
| Without irrigation | ||
| One piece (2.5 bags/day) | 2.23 | 2,009.7 |
| 2-3 pieces (2.5 bags/day; one baseplate/1–3 days) | 1.67; 4.27 | 1,636.08 |
| With irrigation | 1,593.4 | |
| Irrigation system (n=3) | 41.82 | 125.56 |
| Sleeves (n=150) | 1.71 | 256.9 |
| Obdurator (n=120) | 4.23 | 507.48 |
| Stoma bag covers (n=360) | 1.95 | 703.56 |
| Ostomy accessories | 112.16 (1.48%) | |
|---|---|---|
| Adjustable belt (n=1) | 3.11 | 3.11 |
| Adhesive remover product (wipes, spray) (n=3) | 19.78 | 59.34 |
| Skin protection products (paste, powders, moulds) (n=3) | 16.17 | 49.71 |
| Mean cost | 7586.11 |
| Costs in subsequent years | ||
|---|---|---|
| Procedures | Cost/unit (€) | Total costs (€) |
| Consultations | 209.97 (10.34%) | |
| Specialist care | ||
| Stomatherapist (33.2min) (n=3) | 52.39 | 157.17 |
| Primary care | ||
| Face-to-face doctor (7.8min) (n=1) | 14.07 | 14.07 |
| Nursing (7.24min) (n=3) | 12.91 | 38.73 |
| Usual ostomy material | 1,708.14 (84.13%) | |
| Ostomy accessories | 112.16 (5.53%) | |
| Average cost | 2030.27 |
The average cost for planned repair of a parasternal hernia is €6274.45/patient; surgical remodelling of stoma stricture €2070.25/patient; and treatment per episode of irritant dermatitis €120.95/patient. It has been estimated that 50% develop hernia, of which 13% undergo surgery7; 10% develop stenosis, 50% of which are repaired; and 50% suffer irritant dermatitis.8
The average cumulative cost without complications over 10 years is €25,858.54/patient (70.4% in ostomy material and accessories); if the indicated complications are considered, the average cumulative cost would be €26,408.8/patient.
Definitive colostomy is the alternative that generates the highest long-term expenditure, followed by SNS and symptomatic treatment (Fig. 2).
DiscussionFaecal incontinence implies impaired quality of life and significant social and individual economic costs, which increase with the severity of symptoms.2,9
Studies evaluating clinical outcomes and costs of different treatments have limitations: lack of standardisation of procedures, series of few patients, short follow-ups, and great methodological variation in economic evaluations.10 Accurate knowledge of costs is essential to relate them to clinical effectiveness data and to assess the most efficient measures for a health system. It can also be of interest to clinicians, who are often unaware of these data. The purpose of this descriptive study is to determine costs and to serve as a basis for future cost-effectiveness analyses to aid decision-making.
We included patients in whom first-line therapies failed and who continue to have severe faecal incontinence (regardless of aetiology). According to 2 studies,3,4 a score above 9 on the Wexner scale would be the cut-off point at which there is a greater impact on quality of life. In these cases, treatment with SNS, definitive colostomy, or symptomatic treatment alone could be considered. We did not include posterior tibial neurostimulation and bulking agents, as they are not available in our service portfolio. Sphincteroplasty was considered a first-line treatment.
Published data on the direct medical costs of symptomatic treatment are scarce and variable, ranging from €534 to €1,917/patient-year,2,9,11–13 and €1097 in our study. We must highlight the importance of absorbent products, mainly nappies, which in our study come to €719/year and account for two thirds of the direct costs. In the literature, the cost range for nappies and other absorbent products is €163–840/patient-year.2,9,11–13
Healthcare costs will depend on the frequency with which each patient seeks consultation. In our study we calculated 12 visits/year to the primary care doctor or nurse, although some studies estimate more than 20 visits,2 with published costs varying between €128 and €398/year.
In addition, patients require regular medication, with costs ranging from €88 to €350 per year,2,9,13 comparable to the €230 calculated in our study. Some studies include costs related to personal hygiene, cosmetics, diet, laundry, and transport, among others.2,9,12
Lastly, indirect costs, which are difficult to quantify and are often not considered, also have a significant economic impact, and allow analysis of the problem from a social perspective. Due to their illness, patients are less productive or efficient at work, may need to be absent from work more frequently and/or require more help at home due to loss of domestic productivity.2,9 In the literature, only three studies have evaluated these costs, ranging from €1262 to €1361/patient-year,2,9,13 which may represent more than half of the total cost for patients with faecal incontinence.2
SNS can now be considered an established technique in the treatment algorithm for faecal incontinence. Despite its connotation as an expensive technique, few studies have evaluated its cost. Our study analyses a relatively large series5 compared to similar studies and the extensive follow-up enables better assessment of long-term costs. However, in contrast to studies using the more imprecise methodology of coding in diagnosis groups,13–16 our study is based on specific management and analytical accounting tools of the Health System itself, which provide detailed information on the origin of the costs. In general, publications focus on the cost of interventions up until definitive implantation, including expenses for devices, personnel, and hospitalisation, but do not consider the costs of complications or replacement of the device when the battery runs out. Furthermore, in some centres the technique is not performed as major outpatient surgery, but on an inpatient basis, and therefore calculations vary. The estimated costs of electrode implantation range from €744 to €6430/patient, and those of definitive implantation between €6430 and €12,371, in our study they are €3476 and €9691, respectively. Despite the variability of published results, the range of total costs for the sum of both procedures is narrower, between €11,514 and €15,616,13–20 comparable to our result of €13,167. As in our study, the different publications note that devices generate the highest cost. There is only one study that includes the costs of interventions due to complications and generator replacement.20
Colostomy may be a last resort when other treatments fail. Although it solves incontinence, it has negative consequences: secondary costs of stoma care, psychological problems, impaired quality of life, and complications.7,19 Therefore, it is a less common treatment. The few studies published on its costs are heterogeneous and use diagnosis groups, with the disadvantage of not knowing whether the stoma is temporary or permanent, or whether it has been performed on an elective or emergency basis. In fact, cost studies of colostomy in the context of emergency colon surgery, specifically for tumour obstruction, are more common, comparing it or not comparing it with other therapeutic alternatives. Despite this, there is some work that calculates the costs of colostomy in the context of faecal incontinence.14,19–21 According to our study, the initial first-year cost of an uncomplicated elective definitive colostomy is €7586.11; published articles show a range between €2437 and €14,609.14,19–21 Subsequently, we calculated a cost of €2,030.27/year, slightly lower than that reported by other authors, ranging from €2164 to €5339.14,19–21 This high figure may be explained by a significant increase in the prescription of ostomy devices in recent years22–25 related to the increased age of the population, more active lifestyles, demand for a better quality of life, technological innovation, and ease of access.22,25 In our study, we found that ostomy equipment and accessories are the elements generating the highest cost for a colostomised patient, accounting for 70.4% of the total cost over 10 years. The estimated cost of ostomy material and accessories is €1820.3/year, the range in the literature being from €1250 to €3000.8,23–26 It is essential to highlight the role of the stomatherapist, as follow-up from the outset, and then in consultation. It ensures that the patient adapts well to managing their stoma, and helps reduce the number of days of hospitalisation and prevent complications, lowering costs.7,8,22,27,28 The cost of €237.8/year for consultation care in our study can be extrapolated to the estimated €218 in the first 3 months after the intervention in a study by the Spanish Society of Expert Stoma Therapy Nurses.8 Finally, we must anticipate costs for possible complications, since at least half the patients will suffer a complication to varying degrees.7,29 Few studies have assessed this point. One estimates the cost of para-stomal hernia at €4034,30 while others estimate a range of €25 to €372 as the cost for skin problems.25,26
To conclude, failure of first-line treatments for faecal incontinence has great economic impact. The direct costs of symptomatic treatment are mainly for nappies, and although they are lower than the direct costs of the other alternatives, they can be considered the option that generates the most expenditure if we include indirect costs. SNS involves a significant initial cost, but thereafter the increase is smaller. Finally, definitive colostomy is the costliest treatment in the long term, due to ostomy material.
The strengths of the study are the detailed knowledge of costs and the availability of a large number of SNS patients, as well as a long follow-up making it possible to determine future costs. The lack of a large number of colostomy patients and calculations based on estimates of material or consultation costs for symptomatic and colostomy treatment are a limitation.
Further multi-centre studies with appropriate designs and precise tools to calculate costs will be needed in the future. Therefore, by pooling clinical data, the measures that are more cost-effective for a healthcare system can be assessed and inefficient or potentially cost-saving elements identified.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: de Miguel Valencia MJ, Margallo Lana A, Pérez Sola MÁ, Sánchez Iriso E, Cabasés Hita JM, Alberdi Ibáñez I, et al. Impacto económico del tratamiento a largo plazo de la incontinencia fecal grave. Cir Esp. 2022;100:422–430.