Duodenal injuries constitute a challenge to the trauma surgeon, mainly due to their retroperitoneal location. When identified, they present associated with other abdominal injuries. Consequently, they have an increased morbidity and mortality. At best estimates, duodenal lesions occur in 4.3% of all patients with abdominal injuries, ranging from 3.7% to 5%, and because of their anatomical proximity to other organs, they are rarely an isolated injury. The aim of this paper is to present a concise description of the anatomy, diagnosis, surgical management and treatment of complications of duodenal trauma, and an analysis of complications and mortality rates of duodenal injuries based on a 46-year review of the literature.
Las lesiones duodenales, debido a su localización retroperitoneal, constituyen un reto diagnóstico para el cirujano, de forma que son identificadas tardíamente y en consecuencia, se asocian a un aumento de la morbimortalidad. En las mejores estimaciones, las lesiones duodenales ocurren en un 4,3% de todos los pacientes con lesiones abdominales, en un rango de 3,7% a 5%, y además, debido a su proximidad anatómica con otros órganos, sus lesiones raramente se presentan en forma aislada. El objetivo de este trabajo es presentar una descripción concisa de la anatomía, diagnóstico, manejo quirúrgico y tratamiento de las complicaciones del trauma duodenal, y realizar un análisis de las complicaciones y de la mortalidad de las lesiones del duodeno en base a una revisión de la literatura de los últimos 46 años.
Duodenal injuries, due to their retroperitoneal location, are a diagnostic challenge to the surgeon; for this reason, they are identified in a late stage, and thus associated with increased morbidity and mortality.
The purpose of this paper is to present a brief description of the anatomy, diagnosis, surgical management and treatment of duodenal trauma complications, and to perform an analysis of the range of duodenal injury morbidity and mortality, based on an extensive review of the current literature.
Materials and MethodsA search was conducted in PubMed to find articles published in English in the last 46 years, from February 1968 to March 2014. Twenty-three case series on duodenal injuries were found. The English key words duodenal injury, duodenal injuries and duodenal trauma were used for the search.
Incidence of Duodenal InjuriesAccording to the best estimates, duodenal injuries occur in 4.3% of all patients with abdominal injuries, ranging from 3.7% to 5%. The proportion of duodenal injuries between male and female patients is 5–1, and the most affected age range is between 16 and 30 years (70%).1 In addition, the increase in the number of traffic accidents, as well as violence (knives and firearms) has led to a higher incidence in recent decades.
Mechanism of InjuryThe mechanisms of the injuries caused by penetrating trauma occur by a simple lesion in the duodenal wall when it is caused by a knife, and by the penetration and dissipation of kinetic energy from the projectile in the case of gunshot injuries.
The mechanism is more complex in the case of blunt injuries, when both ends may be blunt, and duodenal injuries are a consequence of crushing or compression. Crush injuries usually occur when a direct force is applied against the abdominal wall and transmitted to the duodenum, which is then projected against the spinal column, on which it lies, for example, when the steering wheel impacts the epigastrium. They also occur when acceleration and deceleration forces act on the mobile and non-mobile portions of the duodenum, such as during a fall from a great height.2–7
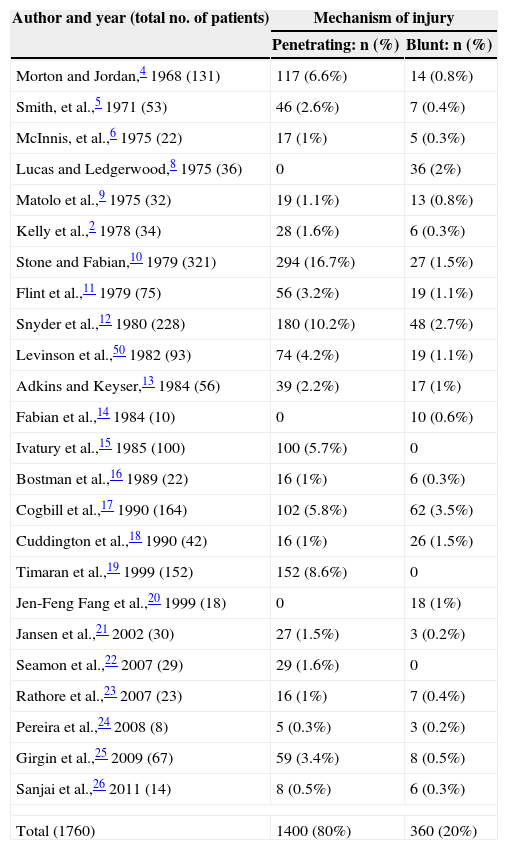
The mechanism of penetrating injury is the most common cause of duodenal trauma. In a review of the literature encompassing 24 series published during the last 46 years (1968–2014), 1760 cases of duodenal injury were identified. Out of these, 1400 (80%) occurred as a result of penetrating trauma, while 360 (20%) occurred as a consequence of blunt trauma.2–26 The range of penetrating abdominal injuries was 3.9:1 (Table 1). Among the 1400 penetrating injuries, 1135 (81%) were caused by gunshots and 257 (19%) by stabbings. Among blunt trauma, the most frequent mechanism was car crash, with a total of 306 patients (85%).
Mechanism of Duodenal Injury.
| Author and year (total no. of patients) | Mechanism of injury | |
|---|---|---|
| Penetrating: n (%) | Blunt: n (%) | |
| Morton and Jordan,4 1968 (131) | 117 (6.6%) | 14 (0.8%) |
| Smith, et al.,5 1971 (53) | 46 (2.6%) | 7 (0.4%) |
| McInnis, et al.,6 1975 (22) | 17 (1%) | 5 (0.3%) |
| Lucas and Ledgerwood,8 1975 (36) | 0 | 36 (2%) |
| Matolo et al.,9 1975 (32) | 19 (1.1%) | 13 (0.8%) |
| Kelly et al.,2 1978 (34) | 28 (1.6%) | 6 (0.3%) |
| Stone and Fabian,10 1979 (321) | 294 (16.7%) | 27 (1.5%) |
| Flint et al.,11 1979 (75) | 56 (3.2%) | 19 (1.1%) |
| Snyder et al.,12 1980 (228) | 180 (10.2%) | 48 (2.7%) |
| Levinson et al.,50 1982 (93) | 74 (4.2%) | 19 (1.1%) |
| Adkins and Keyser,13 1984 (56) | 39 (2.2%) | 17 (1%) |
| Fabian et al.,14 1984 (10) | 0 | 10 (0.6%) |
| Ivatury et al.,15 1985 (100) | 100 (5.7%) | 0 |
| Bostman et al.,16 1989 (22) | 16 (1%) | 6 (0.3%) |
| Cogbill et al.,17 1990 (164) | 102 (5.8%) | 62 (3.5%) |
| Cuddington et al.,18 1990 (42) | 16 (1%) | 26 (1.5%) |
| Timaran et al.,19 1999 (152) | 152 (8.6%) | 0 |
| Jen-Feng Fang et al.,20 1999 (18) | 0 | 18 (1%) |
| Jansen et al.,21 2002 (30) | 27 (1.5%) | 3 (0.2%) |
| Seamon et al.,22 2007 (29) | 29 (1.6%) | 0 |
| Rathore et al.,23 2007 (23) | 16 (1%) | 7 (0.4%) |
| Pereira et al.,24 2008 (8) | 5 (0.3%) | 3 (0.2%) |
| Girgin et al.,25 2009 (67) | 59 (3.4%) | 8 (0.5%) |
| Sanjai et al.,26 2011 (14) | 8 (0.5%) | 6 (0.3%) |
| Total (1760) | 1400 (80%) | 360 (20%) |
The duodenum, by virtue of its anatomic proximity to other important organs, is rarely injured alone. The occurrence of multiple associated injuries is the rule, not the exception. Isolated duodenal injuries are usually seen in the form of duodenal haematoma.
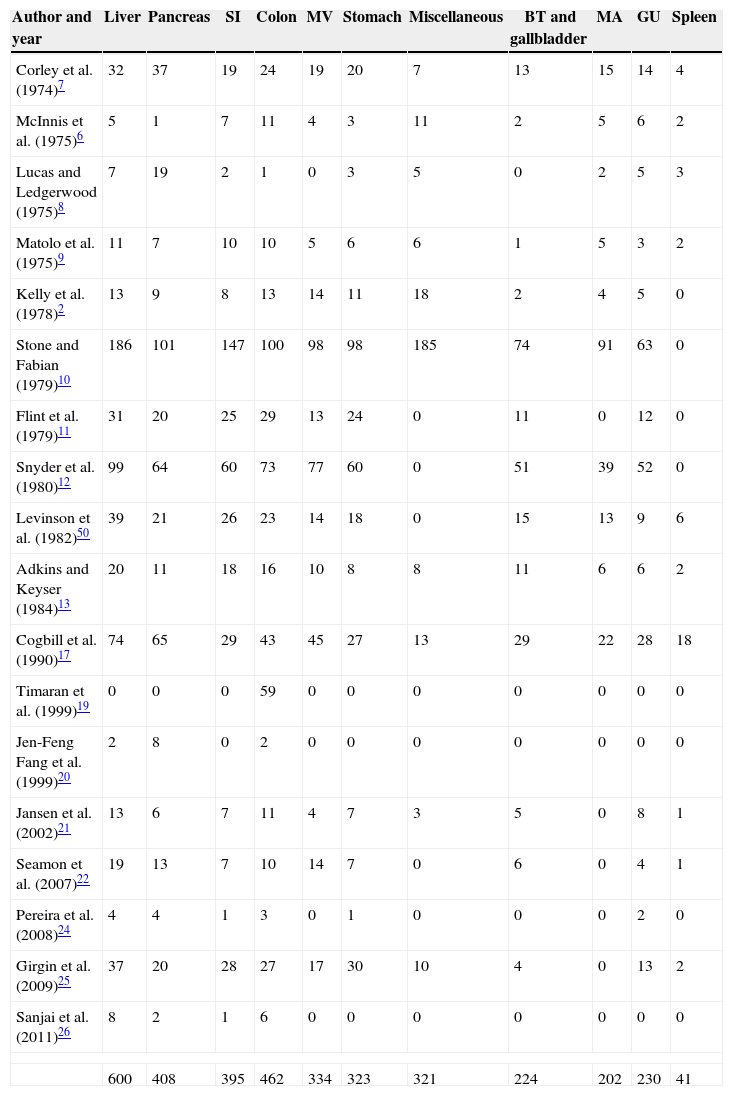
Among the 1760 patients with duodenal trauma, a total of 3540 associated injuries were identified (Table 2). The liver was the most commonly injured organ, with a total of 600 injuries occurring with a frequency of 17%. Other organs included the colon, with 462 (13%); the pancreas, with 408 (12%); the small intestine, with 395 (11%); the stomach, with 323 (9%) and vascular injuries (arterial and venous), with 536 (15%).3,4,6–13,17,19–22,24–26
Associated Injuries by Organs.
| Author and year | Liver | Pancreas | SI | Colon | MV | Stomach | Miscellaneous | BT and gallbladder | MA | GU | Spleen |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Corley et al. (1974)7 | 32 | 37 | 19 | 24 | 19 | 20 | 7 | 13 | 15 | 14 | 4 |
| McInnis et al. (1975)6 | 5 | 1 | 7 | 11 | 4 | 3 | 11 | 2 | 5 | 6 | 2 |
| Lucas and Ledgerwood (1975)8 | 7 | 19 | 2 | 1 | 0 | 3 | 5 | 0 | 2 | 5 | 3 |
| Matolo et al. (1975)9 | 11 | 7 | 10 | 10 | 5 | 6 | 6 | 1 | 5 | 3 | 2 |
| Kelly et al. (1978)2 | 13 | 9 | 8 | 13 | 14 | 11 | 18 | 2 | 4 | 5 | 0 |
| Stone and Fabian (1979)10 | 186 | 101 | 147 | 100 | 98 | 98 | 185 | 74 | 91 | 63 | 0 |
| Flint et al. (1979)11 | 31 | 20 | 25 | 29 | 13 | 24 | 0 | 11 | 0 | 12 | 0 |
| Snyder et al. (1980)12 | 99 | 64 | 60 | 73 | 77 | 60 | 0 | 51 | 39 | 52 | 0 |
| Levinson et al. (1982)50 | 39 | 21 | 26 | 23 | 14 | 18 | 0 | 15 | 13 | 9 | 6 |
| Adkins and Keyser (1984)13 | 20 | 11 | 18 | 16 | 10 | 8 | 8 | 11 | 6 | 6 | 2 |
| Cogbill et al. (1990)17 | 74 | 65 | 29 | 43 | 45 | 27 | 13 | 29 | 22 | 28 | 18 |
| Timaran et al. (1999)19 | 0 | 0 | 0 | 59 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Jen-Feng Fang et al. (1999)20 | 2 | 8 | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Jansen et al. (2002)21 | 13 | 6 | 7 | 11 | 4 | 7 | 3 | 5 | 0 | 8 | 1 |
| Seamon et al. (2007)22 | 19 | 13 | 7 | 10 | 14 | 7 | 0 | 6 | 0 | 4 | 1 |
| Pereira et al. (2008)24 | 4 | 4 | 1 | 3 | 0 | 1 | 0 | 0 | 0 | 2 | 0 |
| Girgin et al. (2009)25 | 37 | 20 | 28 | 27 | 17 | 30 | 10 | 4 | 0 | 13 | 2 |
| Sanjai et al. (2011)26 | 8 | 2 | 1 | 6 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 600 | 408 | 395 | 462 | 334 | 323 | 321 | 224 | 202 | 230 | 41 | |
BT: biliary tree; MA: major arteries; GU: genitourinary; SI: small intestine; MV: major veins.
To identify the most common anatomic location, 15 published series were reviewed.2,6,7,10–15,19,21,22,24–26 A total of 1042 patients were analysed. The most common duodenal injury sites were the second portion (36%), the third portion (18%) and the fourth portion (15%). The least common duodenal injury site was the first portion (13%), and injuries in multiple portions were found in 18%.
DiagnosisThe diagnosis of duodenal injury requires a high level of suspicion. Delayed diagnosis and management of these injuries results in increased morbidity and mortality rates. The diagnosis of duodenal injury is a great challenge after a blunt trauma. Information should include the haemodynamic condition of the patient, the condition in which the vehicle was found, the condition of the steering wheel, the direction of the force of the impact and the extrication path used to remove the victim from the vehicle, as well as in falls from a great height.27
When a patient undergoes secondary examination, it must be remembered that the retroperitoneal location of the duodenum usually precludes early detection of injury by physical examination, which is characterised by minimal findings. Signs of defence, abdominal rigidity and absence of bowel sounds indicate intra-abdominal injury and lead to a surgical procedure. Severe testicular pain and priapism have also been reported in association with duodenal injury, due to pain transmission through the sympathetic fibres running along the gonadal vessels.28
Laboratory tests provide little help in the early diagnosis of duodenal injuries. The serum amylase level is usually considered a possible indicator of duodenal injury; however, due to its low sensitivity and specificity, it must not be used as an indicator of exploratory laparotomy.29 On the other hand, the serum amylase level has a predictive value in the case of patients admitted for observation. Lucas and Ledgerwood8 suggested that the serum amylase level should be determined at 6-h intervals. A persistently elevated amylase level may be of prognostic significance in detecting duodenal injury.
Abdominal X-ray is useful only if it is positive, the presence of gas surrounding the right kidney being one of its characteristic signs. With wide experience in the use of serial gastrointestinal X-ray examination, Felson and Levin30 described the “coil spring sign”, found in the gastrointestinal barium X-ray, which could be diagnostic of intramural duodenal haematoma.
In 1974, Corley, et al.,7 published a series of 17 patients with duodenal rupture in blunt trauma, and evaluated the radiographic findings as to the presence of intraperitoneal free air. These researchers suggested that positive radiographic findings in abdominal plates appeared more commonly in patients with penetrating trauma than in those who suffered blunt trauma. These radiographic findings have also been documented by Stone and Fabian.10
The best method to visualise retroperitoneal organs without an operation is a computed tomography (CT) scan with oral and intravenous contrast. Despite the fact that the use of CT scanning is limited to stable patients, it has proved capable of showing retroperitoneal ruptures of the duodenum, apart from visualising retroperitoneal organs, detecting injuries of the hollow viscera and quantifying intraperitoneal free blood.
Retroperitoneal perforation of the duodenum can be visualised in the CT scan as the leakage of intestinal contents into the lesser sac. These perforations are typically contained and located in this cavity, but occasionally may be in communication with the peritoneal cavity through the foramen of Winslow and produce pneumoperitoneum. In these cases, an examination with Gastrografin® (Bristol-Myers Squibb, Evansville, IN) could reveal the perforation site. In most patients, the contrast medium should be administered slowly through a nasogastric tube so that the duodenal bulb is filled properly, and its distal end should preferably be in the gastric fundus.
The ideal patient position is the right lateral decubitus position. If no leakage is observed, the patient should be placed in the supine position and X-rays repeated, including stomach and duodenum. The test is completed by placing the patient in the left lateral position, which allows better visualisation of the antrum and duodenum. The best method to visualise the retroperitoneal organs is CT scanning with intravenous and intraluminal contrast.31
In a review conducted by Ballard et al.,32 which included 30 patients with duodenal blunt trauma, 18 underwent CT scanning as a method for diagnosing duodenal injury, and in most cases (15 patients), it was performed within the first 4h after admission. The presence of intraperitoneal fluid was the most common finding, 11 cases being reported (73%), followed by the detection of duodenal haematoma in 6 (40%) and pneumoperitoneum in 5 (33%). Moreover, in four patients (27%) with complete duodenal rupture, the CT scan was interpreted as normal. These authors conclude that the “pathognomonic” findings of duodenal trauma, such as the presence of retroperitoneal air and contrast extravasation, only occur in a minority of cases.
Hofer and Cohen33 have described two patients with duodenal perforation secondary to blunt abdominal trauma. The CT scan showed thickening of the duodenal wall, interruption of the contrast medium flow and presence of extraluminal gas and fluid as consistent findings of duodenal injury. The authors conclude that administration of oral contrast maximises CT findings.
Diagnostic peritoneal lavage (DPL), although quite obsolete, can help rule out associated intra-abdominal injuries.7,9
Surgical Management of Duodenal InjuriesThe immediate control of bleeding from vascular structures or solid organs, such as the kidney or spleen, must be the gold standard manoeuvre in abdominal trauma surgery, followed by an immediate control of gastrointestinal contamination. The next step in a trauma laparotomy must consist of a thorough examination of the abdominal cavity. The entire duodenum, including its four portions, must be carefully explored. Findings suspicious of the presence of a duodenal injury include duodenal subcutaneous emphysema, bile in the duodenal wall, free biliary fluid, the presence of retroperitoneal haematoma around the duodenum or a perirenal haematoma. The duodenum must be mobilised through a Kocher manoeuvre, a Cattell and Braasch manoeuvre, or both. These manoeuvres must enable the visualisation of all the anterior and posterior walls of the four portions of the duodenum.
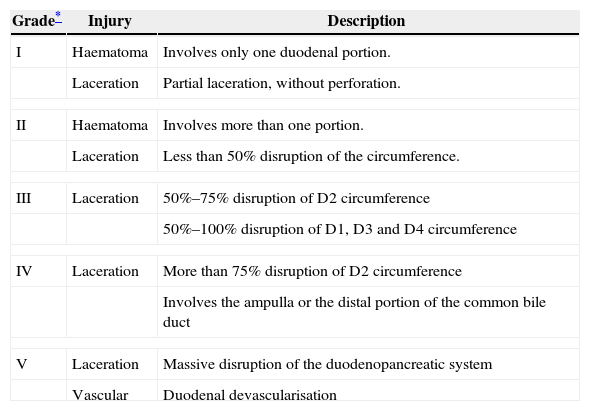
The American Association for the Surgery of Trauma in agreement with the Organ Injury Scale Committee (AAST-OIS) divided injuries into grades (Table 3).34
Duodenal Injury Scale (AAST-OIS).
| Grade* | Injury | Description |
|---|---|---|
| I | Haematoma | Involves only one duodenal portion. |
| Laceration | Partial laceration, without perforation. | |
| II | Haematoma | Involves more than one portion. |
| Laceration | Less than 50% disruption of the circumference. | |
| III | Laceration | 50%–75% disruption of D2 circumference |
| 50%–100% disruption of D1, D3 and D4 circumference | ||
| IV | Laceration | More than 75% disruption of D2 circumference |
| Involves the ampulla or the distal portion of the common bile duct | ||
| V | Laceration | Massive disruption of the duodenopancreatic system |
| Vascular | Duodenal devascularisation | |
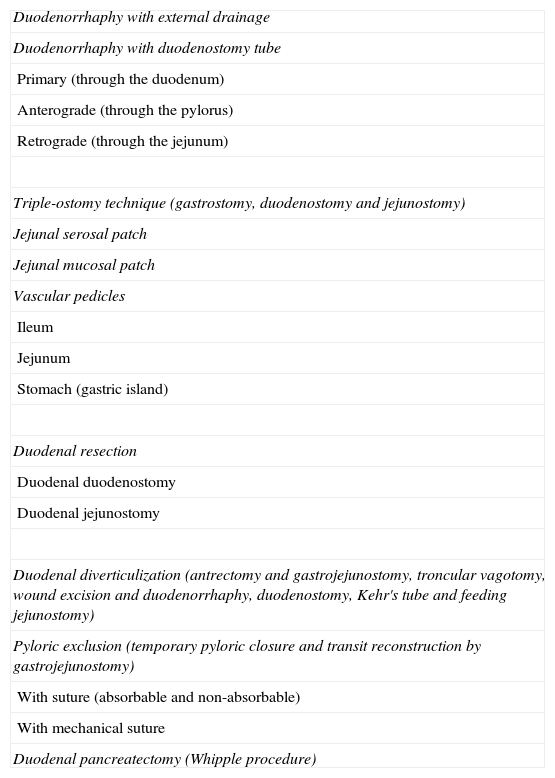
The trauma surgeon must be able to handle different surgical procedures based on injury complexity (Table 4). Controversies have been raised in relation to the use of adjacent manoeuvres to protect the duodenal closure. One of these manoeuvres is the tube duodenostomy technique, which is divided into three types: (a) primary, where the tube is inserted in an orifice different from the wound; (b) anterograde, where the duodenum is decompressed by passing a tube through the pylorus towards the duodenum and (c) retrograde, where the tube is passed through the jejunostomy site.
Surgical Techniques and Procedures to Repair Duodenal and Duodenopancreatic Injuries.
| Duodenorrhaphy with external drainage |
| Duodenorrhaphy with duodenostomy tube |
| Primary (through the duodenum) |
| Anterograde (through the pylorus) |
| Retrograde (through the jejunum) |
| Triple-ostomy technique (gastrostomy, duodenostomy and jejunostomy) |
| Jejunal serosal patch |
| Jejunal mucosal patch |
| Vascular pedicles |
| Ileum |
| Jejunum |
| Stomach (gastric island) |
| Duodenal resection |
| Duodenal duodenostomy |
| Duodenal jejunostomy |
| Duodenal diverticulization (antrectomy and gastrojejunostomy, troncular vagotomy, wound excision and duodenorrhaphy, duodenostomy, Kehr's tube and feeding jejunostomy) |
| Pyloric exclusion (temporary pyloric closure and transit reconstruction by gastrojejunostomy) |
| With suture (absorbable and non-absorbable) |
| With mechanical suture |
| Duodenal pancreatectomy (Whipple procedure) |
In 1979 Stone and Fabian10 introduced the use of the duodenostomy tube as “triple ostomy” (gastrostomy, duodenostomy and jejunostomy). They included 237 patients and only 1 case of duodenal fistula was registered when the duodenostomy tube was used, compared to 8 patients with fistula when it was not used.
In comparison, Ivatury et al.,35,36 found an increase in the occurrence of duodenal fistula and complications in those patients subject to duodenal decompression.
Snyder et al.,12 did not find significantly statistical differences among 101 patients treated with duodenorrhaphy and decompression (9 fistulas, 9%) and 89 patients treated with duodenorrhaphy alone (5 fistulas, 6%).
Since the 1960s, the use of mucosal or serosal patches appeared as a tool within the range of surgical options in duodenal trauma, given that experimental models had shown that the apposition of serous membrane of mobilised jejunal loop to seal full-thickness, non-reconstructible duodenal injuries induced mucous coat in six to eight weeks.37–39 In the 1970s, advances in experimental models, which used, on the one hand, pedunculated jejunal mucosal flaps anastomosed to the defect with double-layer technique,39 and on the other hand, a “pedunculated gastric island” from the greater curvature supplied by the gastroepiploic vessels.40 In the 1990s, the use of pedunculated flaps of the transversus abdominis muscle, which showed good healing in the models, was published in another experimental series.41 However, no studies have been conducted with sound evidence justifying its use in patients with duodenal trauma.
If the entire duodenal circumference has been devitalised, a segmental resection and an end-to-end duodenal anastomosis may be carried out. The resection of the first, third and fourth portions of the duodenum is not associated with a high risk of vascular involvement. The limiting step in the resection of the second portion is attributed to the arterial arcade shared with the pancreas.
Patients with severe duodenal injuries must be considered candidates for complex duodenal repair, such as duodenal diverticulization or pyloric exclusion. Such injuries include those caused by blunt or penetrating trauma, involving more than 75% of the wall, the first and second portions of duodenum, those associated with a delayed repair of more than 24h and those associated with a pancreatic injury, common bile duct injury or both. The main purpose of these procedures is to exclude the duodenum from the passage of gastric contents, to allow time for duodenal repair and to prevent suture line dehiscence. For such purpose, a temporary pyloric closure and transit reconstruction are performed by a gastrojejunostomy. The pyloric exclusion has the advantage of preventing antral resection.
The original duodenal diverticulization was described by Berne et al.42 in 1968. The procedure includes antrectomy and gastrojejunostomy, troncular vagotomy, wound excision and duodenorrhaphy, duodenostomy, Kehr's tube and feeding jejunostomy.
Duodenopancreatectomy for complex duodenal injury was first suggested by Thal and Wilson43 in 1964. Indications to perform a Whipple procedure include massive, uncontrollable bleeding of the head of pancreas or adjacent vascular structures, or isolated or combined non-reconstructible injuries in the duodenum, the head of pancreas and the common bile duct.44
In their 126-month study on duodenopancreatectomy, Asensio and Petrone44 reported their series of 18 patients, out of which one underwent a thoracotomy in the emergency room and was alive upon arrival at the operating room where she/he died. In the 17 remaining patients, a survival of 67% was recorded, compared to 64%–67% shown in literature, considering the severity of injuries, the significant blood loss and the large number of associated abdominal vascular injuries.
MorbidityDuodenal lesions are also associated with a high morbidity rate; complications are mainly represented by fistulas resulting from surgical repair failure due to suture line dehiscence, and are occasionally represented by duodenal obstruction. In a review of the latest 7 series,19–25 with a total of 341 patients, a morbidity rate of 22% was observed. Fifty-one (51) cases of intra-abdominal abscess (15%), 21 of duodenal fistula (6%), 3 of duodenal obstruction (0.9%) and 2 cases of recurrent pancreatitis (0.5%) were reported. Fakhry et al.,45 in a multicentre retrospective study comprising 318 patients with duodenal trauma recorded a morbidity rate of 27.1%.
MortalityMortality secondary to trauma with duodenal involvement may be divided into early and late. Early deaths are caused by exsanguination, usually resulting from associated major vascular injuries, while late deaths are caused by sepsis, duodenal fistula and multiple organ failure. The overall mortality rate reported in recent series was 5.3%–30%.2–14
Factors known to increase the mortality rate include associated pancreatic injury2–10 and common bile duct injury. The most important associated factor for determining duodenal injury mortality may be the delay in injury recognition and repair time. Snyder et al.,12 reported a mortality of 50% in patients who underwent delayed surgery, with a fistula incidence of 50%. In 1975 Lucas and Ledgerwood8 suggested that a delay in diagnosis and treatment greater than 24h may increase mortality from 11% to 40%.
In a paper on the experience in Los Angeles County and the University of Southern California Trauma Centre, correlation between mortality and duodenal injury grade according to the AAST-OIS classification was the following: grade i: 1/12 (8.3%); grade ii: 9/48 (18.7%); grade iii: 16/57 (27.6%); grade iv: 4/13 (30.8%) and grade v: 10/17 (58.8%).46
Special SituationsThe most common cause of duodenal rupture is the epigastric impact of the steering wheel. The best way to establish the diagnosis is by CT with oral or intravenous contrast, or by serial gastrointestinal X-ray examination. The consequences of duodenal rupture are accompanied by a fistula onset rate of up to 50%,2–12 and mortality between 40% and 71%.2–8,12
Another type of duodenal injury requiring special consideration is intramural duodenal haematoma. This is usually caused by a blunt abdominal trauma and may occur in any part of the duodenum. Its incidence has been associated with coagulation disorders, anticoagulant therapy and alcohol abuse. Intramural duodenal haematomas occur as a consequence of vascular rupture inside the duodenal wall. Most of them are submucosal, but subserosal ones have also been reported in intramuscular areas.47 Patients with this condition initially require a nasogastric tube and parenteral nutrition. If the duodenal haematoma does not resolve within two to four weeks, surgery will be indicated.48–50
Duodenal injuries may also occur after endoscopic procedures, such as the upper gastrointestinal endoscopy and endoscopic retrograde cholangiopancreatography (ERCP). Bleeding from the ampulla of Vater after endoscopic sphincterotomy may occur and, although rarely, a surgical procedure may be required.
ConclusionOnce the need for a surgical procedure is established, duodenal injury extension and its relation to other structures should be carefully assessed and an adequate surgical treatment should be applied in each case, saving the more complicated techniques, such as diverticulization and pyloric exclusion, for the more complex injuries, while most injuries will only require simple techniques such as wound excision and duodenorrhaphy.
The high mortality rate related to duodenal trauma is affected mostly by the existence of associated injuries, among which penetrating injuries are the ones that involve greater intraoperatory blood loss and shock.
Conflicts of InterestThe authors declare that they do not have any conflicts of interest.
Please cite this article as: García Santos E, Soto Sánchez A, Verde JM, Marini CP, Asensio JA, Petrone P. Lesiones duodenales secundarias a traumatismo: revisión de la literatura. Cir Esp. 2015;93:68–74.