The overall 5-year survival rate for pancreatic cancer does not exceed 10%,1 and, despite the fact that surgery continues to be the only curative treatment, the survival rate of resected patients remains low, with a 5-year rate of no more than 25%.
The main causes of this poor prognosis are mainly due to the lack of early detection, rapid spread, and poor response to systemic treatments.2
Among the prognostic factors, lymph node involvement is one of the most relevant, although its preoperative study continues to be insufficient.3 Endoscopic ultrasound has a sensitivity for detection of lymphadenopathy superior to computed tomography (CT) and magnetic resonance imaging (MRI), ranging between 41% and 86%.4
In the absence of tools for proper lymph node staging, we believe that indocyanine green may play an important role in pancreatic cancer.
We present the case of a 78-year-old woman who was referred to our hospital after CT scan diagnosed a tumor in the head of the pancreas. The study was completed with gastroscopy and MRI, which confirmed the presence of a tumor measuring 1.7cm causing choledochal stenosis measuring 4cm in length and significant dilation of the extrahepatic bile duct. No pathological lymphadenopathies were detected in the preoperative study.
After being assessed by a multidisciplinary committee, a surgical intervention was indicated. A Whipple procedure (pancreaticoduodenectomy) and lymphadenectomy were performed with prior detection of the sentinel node lymph by fluorescence imaging and perilesional injection of indocyanine.5
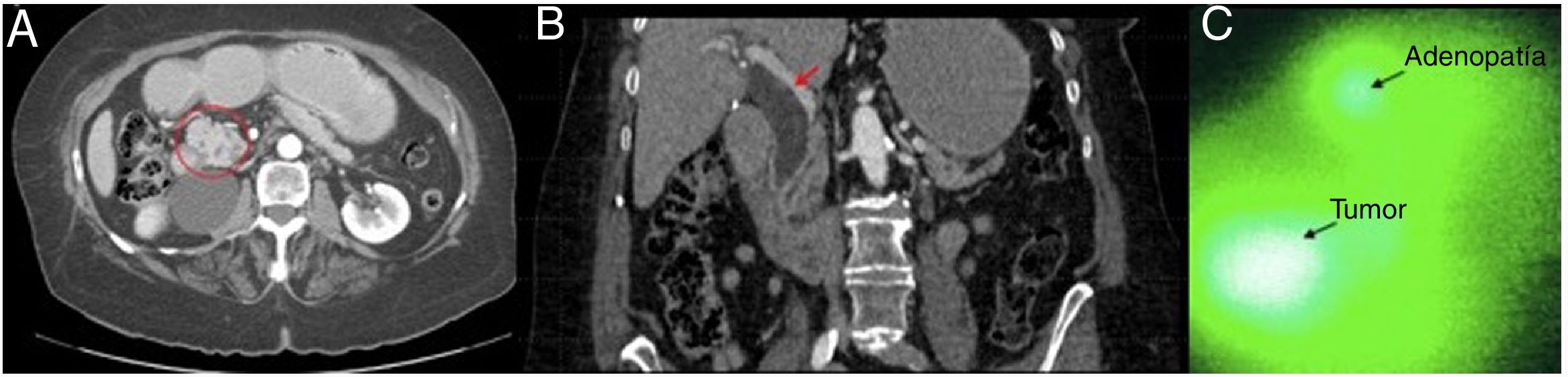
The technique entailed preparing a diluted solution of 25mg of indocyanine green in 10cc of saline.6 During the procedure, once the Kocher maneuver had been performed, 1cc of saline was injected near the surface of the tumor to create a wheal to facilitate the diffusion of the dye. Subsequently, 1cc (2.5mg) of the prepared indocyanine green solution was injected in the wheal created. After injection, the fluorescence image was emitted and processed, and fluorescence vision was maintained for 4min. Within a few seconds, we observed the presence of 2 foci of uptake (primary tumor and lymph node), which captured the green dye with greater intensity than the rest of the tissue (Fig. 1).
Lymphadenopathy (A) Axial CT scan: tumor in the head of the pancreas (marked with a circle); (B) Coronal CT scan: dilation of the bile duct (red arrow) caused by a tumor in the head of the pancreas; (C) Intraoperative image with indocyanine green dye of a tumor in the head of the pancreas, with synchronous uptake of a common hepatic artery lymph node. The images indicated with an arrow correspond to the actual green color that arises from the fluorescent effect created with indocyanine.
Lower arrow: pancreatic head tumor (ductal adenocarcinoma); upper arrow: lymphadenopathy of the common hepatic artery chain.
The largest mass corresponded with the tumor of the head of the pancreas, and the second, located at the top of the image, was associated with a lymphadenopathy found in the lymph node chain of the common hepatic artery, which was resected and marked with a suture to be processed histologically. After 4min, we continued with the rest of the surgical procedure, without incident.
The definitive pathology report confirmed the presence of a well-differentiated ductal adenocarcinoma of the head of the pancreas, with free resection margins and associated lymphovascular and perineural invasion. In terms of lymph node involvement, 13 lymph nodes were isolated, and it was confirmed that the only node positive for tumor invasion was the node that captured the indocyanine green during the procedure, stage pT1N1.
The use of indocyanine green for the detection of the sentinel lymph node is more widespread in other types of tumors, such as gastric cancer6 or breast cancer.7 In pancreatic cancer, however, its usefulness and applicability have yet to be demonstrated.8,9
Lymph node involvement is one of the most important prognostic factors, and the reality is that locoregional recurrence in patients with pancreatic adenocarcinoma undergoing surgery with curative intent remains an unsolved problem.
Extended lymph node dissection has not been shown to be superior to standard lymphadenectomy in terms of overall survival,10 and recurrence rates after surgery continue to be high (1, 2, and 5-year rates of 56.7%, 76.6%, and 84.1%, respectively11).
The multiple lymphatic drainage pathways raise the possibility that there is no dominant sentinel node12 and that, to achieve optimal oncological results, it is necessary to perform systematic lymphadenectomy. However, there are no validated studies that demonstrate or refute the existence of the sentinel node in pancreatic cancer.
In recent years, the use of fluorescence imaging has increased significantly in hepatobiliary and pancreatic surgery, but there are no comparative studies that define its intraoperative applicability for lymph nodes.13 The complexity of the pathways for lymphatic dissemination of pancreatic adenocarcinoma makes it a difficult-to-define terrain, in which technological advances can play a fundamental role helping us to clarify these lymphatic routes.
In this context, we believe that the use of intraoperative indocyanine green for the detection of the sentinel node using fluorescence imaging can help outline the involved lymph node territory, thereby achieving better targeted lymph node dissection.
Please cite this article as: Matallana C, Pardo F, Espín F, Cremades M, Cugat E. Detección del ganglio centinela en el cáncer de páncreas mediante imagen de fluorescencia. Cir Esp. 2020;98:301–303.