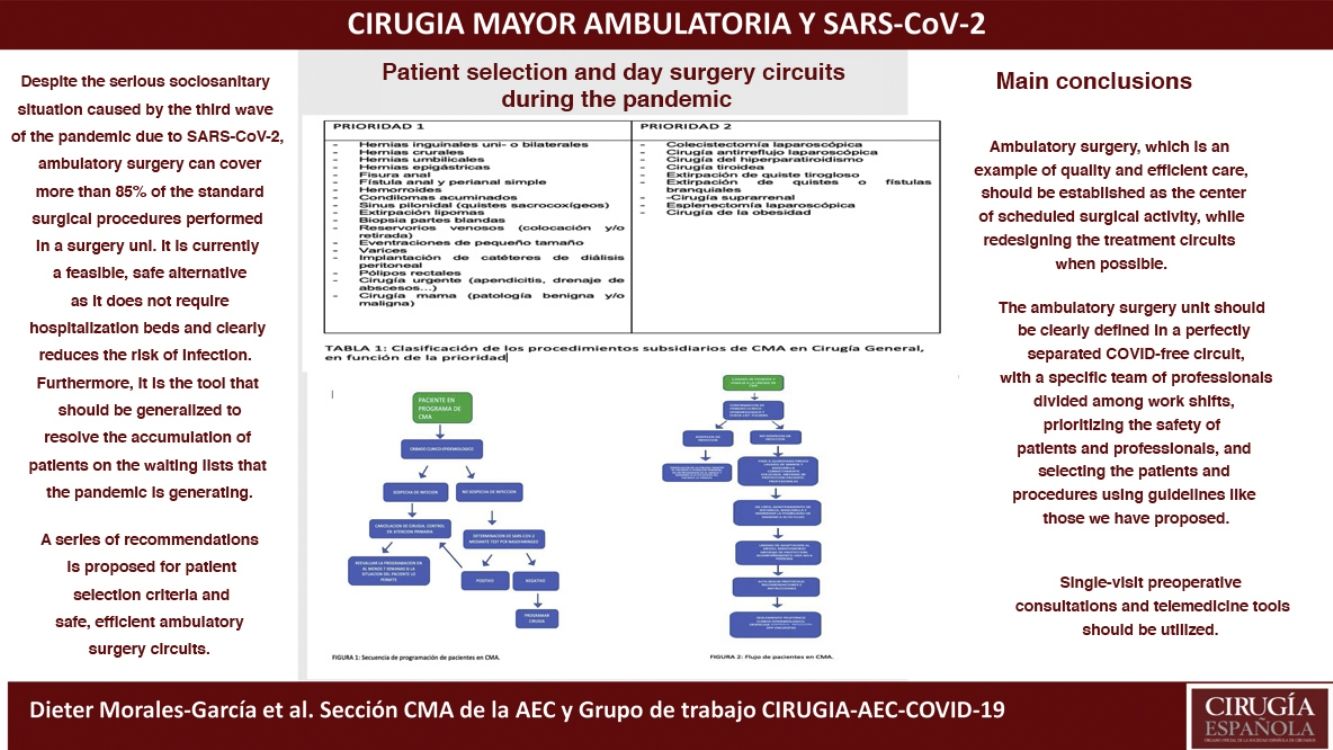
The current situation of the SARS-CoV-2 pandemic has paralyzed non-urgent and/or oncological surgery in many hospitals in our country with what it means for the health of citizens who are awaiting a surgical procedure. Outpatient Surgery can afford more than 85% of the surgical procedures that are performed in a surgical department and is presented as a feasible and safe alternative at the present time since it does not require admission and decreases clearly the risk of infection. In addition, it is the tool that should be generalized to solve the accumulation of patients on the waiting list that the pandemic is generating, so it seems appropriate that the Ambulatory Surgery section of the Spanish Association of Surgeons present a series of recommendations for the implementation of outpatient surgery in these exceptional circumstances that we have to live.
La situación actual de la pandemia por SARS-CoV-2 tiene paralizada la cirugía no urgente y/o oncológica en muchos hospitales de nuestro país con lo que esto conlleva para la salud de los ciudadanos que están pendientes de una intervención quirúrgica. La Cirugía Mayor Ambulatoria puede abarcar en su cartera de servicios mas del 85% de los procedimientos quirúrgicos que se realizan en un servicio de cirugía y se presenta como una alternativa factible y segura en el momento actual ya que no precisa de camas de ingreso y disminuye claramente el riego de infección. Además, es la herramienta que debería de generalizarse para solucionar la acumulación de pacientes en lista de espera que la pandemia esta generando, por lo que parece oportuno que desde la sección de Cirugía Mayor Ambulatoria de la Asociación Española de Cirujanos se presenten una serie de recomendaciones para la implementación de la misma en estas circunstancias excepcionales que nos toca vivir.
In February 2021, the world is still mired in the pandemic due to the SARS-CoV-2 virus. Spain in particular1 is suffering the consequences, as it is immersed in a third wave that is forcing us to suspend surgeries of all kinds (except emergencies) in many hospitals of our country. However, despite this serious situation, we cannot and should not forget that, in addition to COVID-19, many patients have surgical problems, etc, that have an even greater effect on their lives. Elective surgical activity must prioritize the safety of patients and healthcare professionals throughout the process2,3. However, as stated by Balibrea4, surgery must continue. We cannot let patients with non-COVID pathology be neglected, patients who have been waiting for months for a surgical intervention that in many instances affects their family life, social life and occupational life in addition to their health. Moving forward, this situation should make us reflect on all the possible lines of action5, and ambulatory surgery is a process that offers alternatives.
As doctors and as part of the society involved, we collaborate in the search for the most appropriate solutions in these times of urgency, in which all available resources have been made available to control the pandemic. As surgeons, we have developed our role in these special circumstances, with strategic, instrumental and personal support.
This has led to a profound change in healthcare activity, from the transfer of surgical hospital beds to care for patients admitted due to COVID-19, to establishing online consultations or teleconsultations to avoid infecting other patients, as well as the cancellation of scheduled surgeries, operating exclusively on individuals with urgent or serious oncological conditions that cannot be postponed. In certain cases, this has meant that patients have come to the Emergency Department in not exactly the best condition6.
The evidence existing to date, both on the infection and on the surgical approach to it, has been intensively and continuously shared and updated in a short space of time by the Spanish Association of Surgeons (AEC) and its divisions2,3,7–10, in permanent contact with other scientific societies11–16. This has made it possible to treat a large number of patients and has put the entire Spanish healthcare system to a great test of strength, and the response of all health professionals is being exceptional.
In this situation, there is much long-term scientific evidence to demonstrate that ambulatory surgery is a safe, effective and efficient system for resolving the processes included in the portfolio of services offered17–19.
From the Ambulatory Surgery Division of the AEC, on behalf of all the surgeons who perform day surgery in our country, we believe that this is an example of quality and efficiency of care that should be established as the center of scheduled surgical activity in these difficult times. Surgical treatment circuits and the function of services should be redesigned to achieve outpatient treatment rates in line with those established in our setting. This can and should be a priority solution to the great demand for surgery that lies ahead after the COVID-19 epidemic20,21.
The role of scientific societies in coordination with healthcare authorities is crucial in dealing with this pathology. When there is good coordination and receptivity, the suggestions of scientific societies, in this case the Spanish Association of Major Ambulatory Surgery (ASECMA) and its Board of Directors, have managed to improve the resolutions published in different government bulletins based on the existing evidence, providing solutions22,23 and giving day surgery the significant role it should play at this time.
From the outset, the AEC, its divisions and the Surgery-AEC-COVID-19 workgroup3, together with other societies (including ASECMA)15, have drawn up recommendations to be used as a guideline for the development of local protocols16. Following these recommendations and adapting them to the day surgery setting, we propose a series of actions to be able to safely continue operating with guaranteed safety for patients, which must be reviewed as the epidemic evolves.
Management of ambulatory surgery in SARS-CoV-2The ambulatory surgery unit must be clearly defined in a perfectly separated COVID-free environment, regardless of whether it forms part of the physical structure of the hospital or is an isolated unit15,16.
The management recommendations are as follows:
- 1
There must be a specific day surgery committee within the hospital’s COVID surgical committee, with representation of specialists and units involved in day surgery, who, as experts, advise on decision-making for ‘what, how and in what way’ while taking into account the epidemiological risk and the resources available. This sort of plan is very important at this time.
- 2
Similarly, the ambulatory surgery circuit must be clearly differentiated in the hospital (regardless of the unit type available), from the hospital access to the consultations and in the surgical area itself, as well as the location of the ambulatory surgery unit.
- 3
It is highly recommended that the consultation for surgery, nursing and anesthesia be simultaneous and on the same day that the patient is included on the surgical waiting list, in the so-called “one-step consultation”15.
- 4
Regarding the management of people, at this time it would be advisable to have a specific team from and for ambulatory surgery, in which the professionals could be distributed in work shifts in order to be able to immediately cover any contingency without negatively affecting treatment or continuity of care.
The selection of patients for ambulatory surgery based on medical, social or day surgery criteria, etc, is perfectly defined for each procedure within the different guidelines17,18, as well as in the intra-hospital protocols of each institution based on its portfolio of services.
In the current situation, we should be able to identify which patients and which pathologies require surgery, and with what level of priority. To this end, the guidelines of the American College of Surgeons (ACS) and the AEC can be used as a reference12,16,24,25, and also for oncology patients.
We must take into account the pathology that is the cause of the intervention, the procedure and the patient’s status. The AEC proposes a dynamic scale that defines 5 phases in the evolution of the COVID-19 pandemic as it waxes and wanes7.
The Ambulatory Surgery Division proposes establishing surgical priorities based on the following factors:
- 1
In the current situation, criteria such as priority at the time of inclusion (standard, preferential and urgent) should be used to indicate the surgery of patients who have been included preferentially or urgently, which is done based on strictly objective criteria, as well as the current situation of the patient, which may have changed since their inclusion on the waiting list.
- 2
Surgical activity will be determined by the phase of the pandemic in which we find ourselves.
- 3
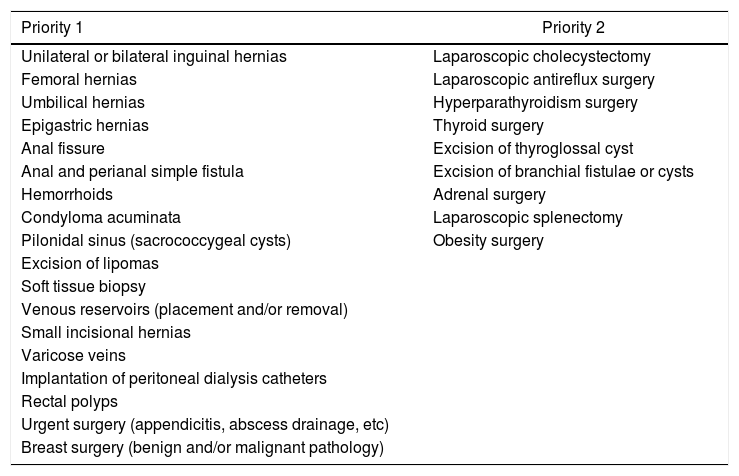
Table 1 proposes a prioritization of interventions based on diagnosis, such as ‘priority 1’ or ‘priority 2’ diagnoses. This is basically done according to the degree of complexity and depending on whether the surgical intervention can be performed with an anesthetic technique that does not require instrumental manipulation of the airway. Also, we must not forget that, although day surgery encompasses moderately complex procedures, more and more complex patients are now being treated, and surgeries are being performed with greater difficulty.
Table 1.Classification of General Ambulatory Surgery procedures, listed by priority.
Priority 1 Priority 2 Unilateral or bilateral inguinal hernias Laparoscopic cholecystectomy Femoral hernias Laparoscopic antireflux surgery Umbilical hernias Hyperparathyroidism surgery Epigastric hernias Thyroid surgery Anal fissure Excision of thyroglossal cyst Anal and perianal simple fistula Excision of branchial fistulae or cysts Hemorrhoids Adrenal surgery Condyloma acuminata Laparoscopic splenectomy Pilonidal sinus (sacrococcygeal cysts) Obesity surgery Excision of lipomas Soft tissue biopsy Venous reservoirs (placement and/or removal) Small incisional hernias Varicose veins Implantation of peritoneal dialysis catheters Rectal polyps Urgent surgery (appendicitis, abscess drainage, etc) Breast surgery (benign and/or malignant pathology) - 4
In the current situation, the immediate incorporation of new procedures (not previously included, or no previous experience) in the portfolio of services is not recommended, but this will depend on each center and day surgery team.
- 5
The patient’s risk, classified according to predictive factors for 30-day mortality11, may be high: male patients, >70 years, with significant associated comorbidity (American Society of Anesthesiologists [ASA] classification III or IV) and in need of major surgery for oncological pathology; or moderate in the remaining situations13,16. By definition, the risk of ambulatory surgery procedures is moderate or low.
- 6
In the case of cancer patients in alert stage III, we should operate on those individuals whose treatment cannot be delayed because their survival could worsen within the next three months, prioritizing patients who cannot undergo neoadjuvant treatment and those that do not require prolonged stays in intensive care, which would not be necessary for ambulatory surgery.
- 7
Priority will be given to those patients who present locally advanced neoplasms with associated complications. In alert scenario II, all types of cancer patients can be operated on, following the prioritization described16.
- 8
For oncology patients who are candidates for outpatient surgery, such as those with breast cancer or dermatological tumors, specific scales should be used to determine the patient’s global status and complete the prioritization assessments for the procedure, especially that of the Eastern Cooperative Oncology Group (ECOG).
- 9
For the reintroduction of activity in the unit, initially ASA 1 and 2 patients under 60/65 years of age should preferably be included, while avoiding, if possible, patients under treatment with immunosuppressants or corticosteroids15.
- 10
Initially, it is not recommended to include patients who are institutionalized (nursing homes, penitentiary institutions, or elderly care centers). However, as soon as institutionalized elderly patients are vaccinated (which is foreseeable in the short-term, depending on the vaccination criteria of the ministry26), these patients could be included preferentially for ambulatory surgery.
In order to offer the best service and care to patients, healthcare professionals must be adequately protected12,27–29.
For effective protection, the following recommendations should be followed:
- 1
The supply of and replacement of personal protective equipment (PPE) must be guaranteed for all staff involved in the ambulatory surgery process.
- 2
Early detection of active SARS-CoV-2 infection among staff is necessary to provide safe care for patients and prevent them from becoming vectors of SARS-CoV-2. Therefore, it is recommended to follow the protocols of the Preventive Medicine Services and Occupational Risk Prevention Services of each hospital16. These activities range from providing adequate and correct information about the disease to all staff and the prioritization of screening tests to the clinical follow-up of all staff who could be positive and all their contacts, in accordance with the recommendations of the Ministry of Health or the administrations of the Spanish ‘autonomous communities themselves.
- 3
During the pandemic, preoperative screening for active SARS-CoV-2 infection is recommended for all patients who are scheduled to undergo elective surgery15,16,27,28,30,31.
- 4
The choice of tests included in the screening protocol in the form of polymerase chain reaction (PCR), antigens, imaging tests, etc, will vary depending on the epidemiological alert scenario and following the AEC scale as well as the epidemiology of the region or province, through the cumulative incidence of cases diagnosed with SARS-CoV-2 infection in the last 14 days.
- 5
Depending on the epidemiological scenario, all patients will have a PCR test within 72 h of the scheduled date for surgery. The patient will not be allowed in the unit until the result of the PCR is provided.
- 6
Each unit must establish the patient circuit for the PCR test and evaluation of the result before surgery.
- 7
Like other scientific societies, we recommend that the patient and their companion rigorously maintain distancing measures from the day of the preoperative PCR until the date of their surgery to reduce the risk of infection15,16.
- 8
In phase I alert, the epidemiological situation is considered favorable, and practically normal surgical activity can be carried out, maintaining the safety measures agreed upon with preventive medicine. In this situation, and in patients with intermediate risk and surgery, PCR will be omitted9. In the case of a patient with a positive PCR, as in cases of suspicious symptoms of COVID-19 disease during screening, surgery will be suspended and postponed for at least seven weeks, provided that the pathology and the patient’s status allow32. The patient will be referred to the primary care doctor, who will establish the appropriate confinement and treatment measures15,16.
- 9
Patients with negative PCR may be scheduled for surgery without the requirement of additional preoperative tests15,16.
The ambulatory surgery consultation can be a second, successive or even the first consultation, in which the patient is added to the surgical waiting list, based on their diagnosis.
Recommendations for the consultation follow:
- 1
During the COVID-19 pandemic, “single-visit outpatient surgery consultations are encouraged”, at which time the surgeon will assess the patient, the patient is added to the waiting list, the anesthesiologist and CMA nursing staff evaluate the patient, and preoperative tests are done15,32.
- 2
In order to avoid unnecessary visits to the hospital and for the sake of epidemiological screening, a preoperative teleconsultation is used33,34 for simple screening and subsequent scheduling of the multiple consultation visit to the hospital in the case of first visits, or as a single teleconsultation in successive ones. Therefore, it is necessary to establish a system of communication with the patient (email/telephone/e-consultation) that guarantees compliance with data protection laws.
- 3
In this teleconsultation, through a simple questionnaire (Appendix B, Addendum I) and in the event that one or more of the answers is affirmative, the consultation (or the surgery, if already scheduled) is postponed for a minimum period of seven weeks. The patient is referred to the Primary Care doctor, who will establish the appropriate isolation and follow-up measures.
- 4
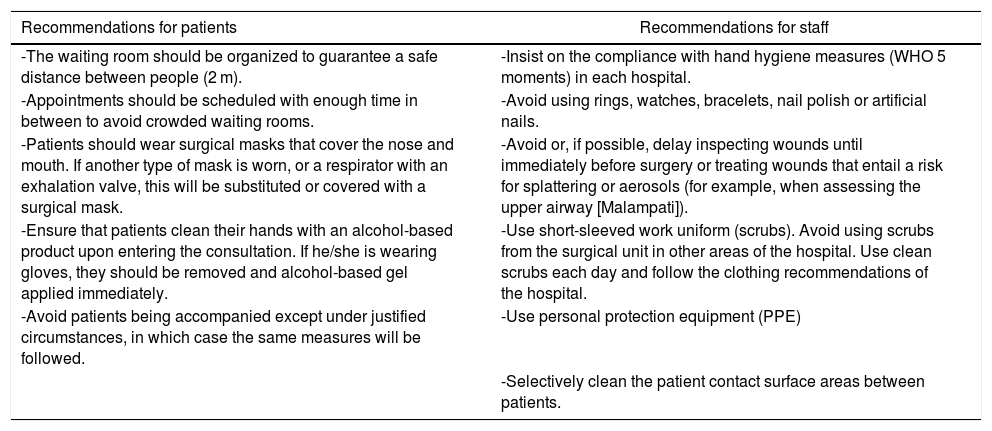
In the in-person consultation, a series of recommendations must be followed by both patients and healthcare professionals (Table 2) to guarantee the safety of all15,16.
Table 2.Recommendations for patients and staff in the ambulatory surgery consultations.
Recommendations for patients Recommendations for staff -The waiting room should be organized to guarantee a safe distance between people (2 m). -Insist on the compliance with hand hygiene measures (WHO 5 moments) in each hospital. -Appointments should be scheduled with enough time in between to avoid crowded waiting rooms. -Avoid using rings, watches, bracelets, nail polish or artificial nails. -Patients should wear surgical masks that cover the nose and mouth. If another type of mask is worn, or a respirator with an exhalation valve, this will be substituted or covered with a surgical mask. -Avoid or, if possible, delay inspecting wounds until immediately before surgery or treating wounds that entail a risk for splattering or aerosols (for example, when assessing the upper airway [Malampati]). -Ensure that patients clean their hands with an alcohol-based product upon entering the consultation. If he/she is wearing gloves, they should be removed and alcohol-based gel applied immediately. -Use short-sleeved work uniform (scrubs). Avoid using scrubs from the surgical unit in other areas of the hospital. Use clean scrubs each day and follow the clothing recommendations of the hospital. -Avoid patients being accompanied except under justified circumstances, in which case the same measures will be followed. -Use personal protection equipment (PPE) -Selectively clean the patient contact surface areas between patients. WHO: World Health Organization.
- 5
The patient’s medical records should reflect whether the consultation was in-person or not. The interview must be recorded in the medical record, indicating that the patient has been informed of the characteristics of the intervention, the associated risks, the patient’s acceptance to participate in it and the consent given by the patient.
- 6
It would be highly efficient and useful to have an electronic signed informed consent (IC), since this would avoid the circulation of paper documents through different departments, although organizing the signature of the IC form will depend on each unit according to its characteristics. Many hospitals are including a specific consent form regarding the current COVID pandemic situation as an addendum to the IC.
- 7
In the case of patients who have had COVID-19 disease, both the decision of their outpatient surgery and the request for additional preoperative tests will be decided on in an individual manner15.
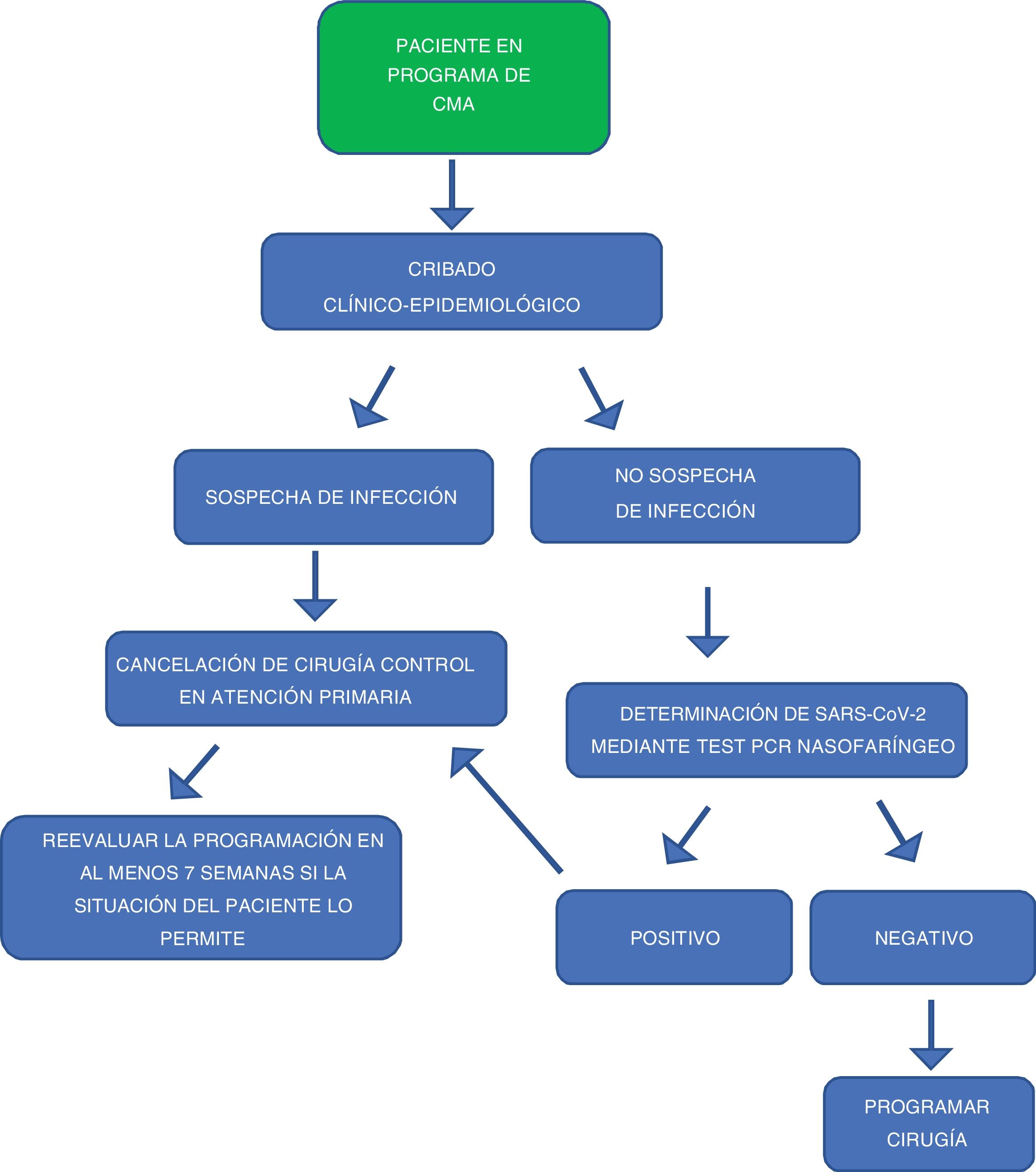
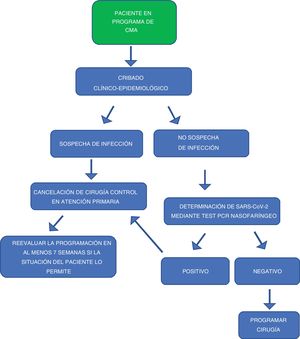
Fig. 1 shows the sequence for including patients on the ambulatory surgery waiting list.
Major ambulatory surgery unit and operating roomEach unit, depending on its characteristics and resources, must assess the spaces and circuits in order to maintain safe distances in all phases of the process2.
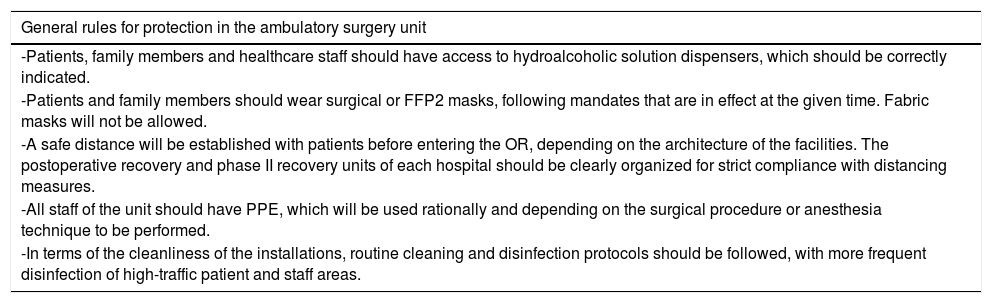
The general protection standards of the ambulatory surgery unit are expressed in Table 3.
General rules for protection in the ambulatory surgery unit.
| General rules for protection in the ambulatory surgery unit |
|---|
| -Patients, family members and healthcare staff should have access to hydroalcoholic solution dispensers, which should be correctly indicated. |
| -Patients and family members should wear surgical or FFP2 masks, following mandates that are in effect at the given time. Fabric masks will not be allowed. |
| -A safe distance will be established with patients before entering the OR, depending on the architecture of the facilities. The postoperative recovery and phase II recovery units of each hospital should be clearly organized for strict compliance with distancing measures. |
| -All staff of the unit should have PPE, which will be used rationally and depending on the surgical procedure or anesthesia technique to be performed. |
| -In terms of the cleanliness of the installations, routine cleaning and disinfection protocols should be followed, with more frequent disinfection of high-traffic patient and staff areas. |
When the patient arrives at the hospital, it is necessary to confirm that the clinical-epidemiological survey is available in the medical records along with the negative PCR result as well as the verification of the IC. The patient’s temperature is taken, and an identification bracelet will be placed on his/her wrist. Some scientific societies15 recommend that the patient’s accompanying family member also complete the clinical-epidemiological screening survey.
Ambulatory surgery unit waiting room- 1
Both the patient and family member must wear a surgical mask throughout their stay in the hospital.
- 2
It is recommended to limit the patient to a single companion, who should wait outside the surgical ward to avoid crowding the area.
- 3
The chairs in the waiting rooms of the day surgery units must be 2 m apart.
- 4
Screens are also recommended to inform the patients.
The patient’s personal belongings should be stored in the locker or other pre-determined space and handled only when they are going to be used in order to leave surfaces uncluttered to allow for frequent cleaning and sanitizing. The patient must inform the healthcare personnel if the/she has experienced any changes or symptoms related to the COVID-19 infection.
Before taking the patient to the operating room, the nursing staff must complete a checklist to verify the following items15:
▪The patient is correctly identified by the bracelet and is correctly wearing a mask.
▪Patient temperature
▪Negative clinical-epidemiological screening
▪Negative PCR result
▪Signed IC form (procedure and specific COVID-19)
▪Compliance with preoperative instructions (fasting, etc)
The operating room should be specific and exclusive for day surgey, and the following general guidelines should be followed.
- 1
An attempt will be made to prioritize surgical techniques that do not require anesthetic procedures that manipulate the airway, based on the criteria put forth in the patient selection section28,30,32 and for the types of interventions proposed in Table 1.
- 2
For surgical or anesthetic procedures that are likely to generate aerosols, it is necessary to use PPE.
- 3
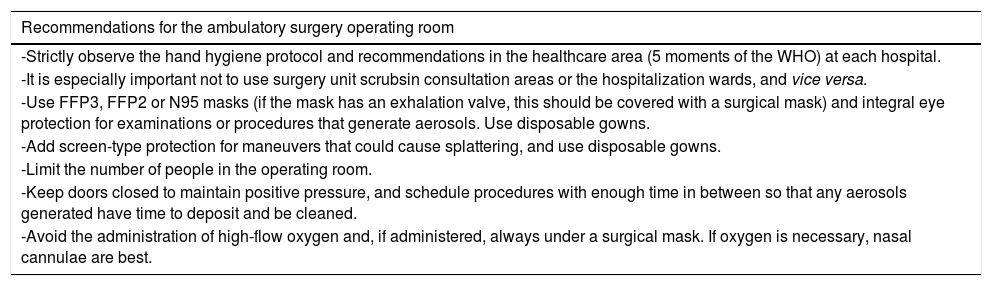
Table 4 lists a series of specific measures to be used in the operating room.
Table 4.Recommendations for the ambulatory surgery operating room.
Recommendations for the ambulatory surgery operating room -Strictly observe the hand hygiene protocol and recommendations in the healthcare area (5 moments of the WHO) at each hospital. -It is especially important not to use surgery unit scrubsin consultation areas or the hospitalization wards, and vice versa. -Use FFP3, FFP2 or N95 masks (if the mask has an exhalation valve, this should be covered with a surgical mask) and integral eye protection for examinations or procedures that generate aerosols. Use disposable gowns. -Add screen-type protection for maneuvers that could cause splattering, and use disposable gowns. -Limit the number of people in the operating room. -Keep doors closed to maintain positive pressure, and schedule procedures with enough time in between so that any aerosols generated have time to deposit and be cleaned. -Avoid the administration of high-flow oxygen and, if administered, always under a surgical mask. If oxygen is necessary, nasal cannulae are best. WHO: World Health Organization.
Recommendations for the post-anesthesia care unit (PACU) are as follows:
- 1
Patients will continue to wear a mask in the PACU at safe distances from each other.
- 2
As in the operating room, high-flow oxygen administration should be avoided.
- 3
Venturi masks should be avoided, as they diffuse the spread of droplets if the patient coughs and favor the potential aerosolization of the virus.
- 4
The PACU, like the operating room and the phase II unit, should be specific for ambulatory surgery patients.
Patients must continue to wear masks, and a safety distance must be maintained between patients. It would be preferable if the patient were alone.
Information to relativesA specific circuit must be defined to inform family members while avoiding crowded waiting rooms. Some hospitals have established a real-time information system using applications for mobile devices by which family members are informed of the beginning, duration and completion of the surgical intervention in real time. In times like these that bring about the opportunity for change, it would be highly desirable for the use of devices like these (as well as the electronic signature of the IC) to become generalized in all hospitals in our country.
At homeAt discharge, the patient’s family support should be evaluated at discharge, which ideally will also have been considered in the preoperative evaluation.
Regular follow-up of the patient will be carried out, with special emphasis on social distancing measures and notification of any complication regarding the patient’s process or the appearance of any symptom related to COVID-1915,31.
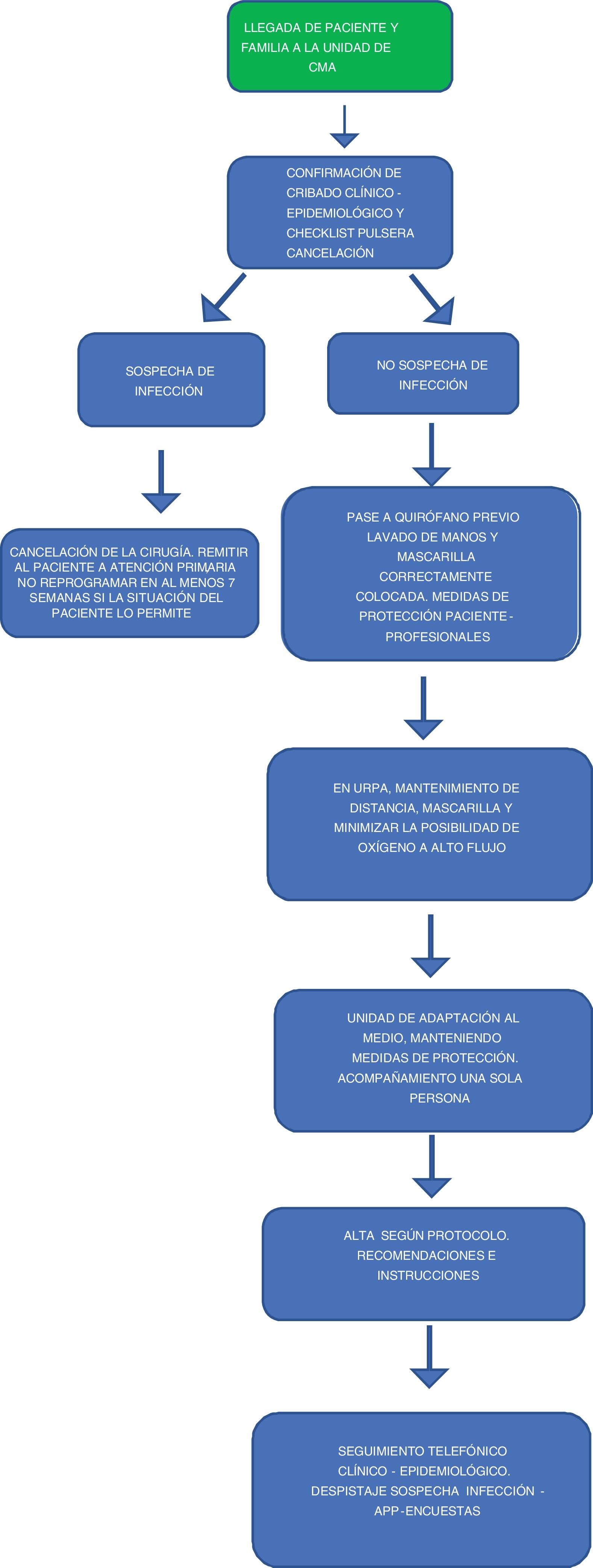
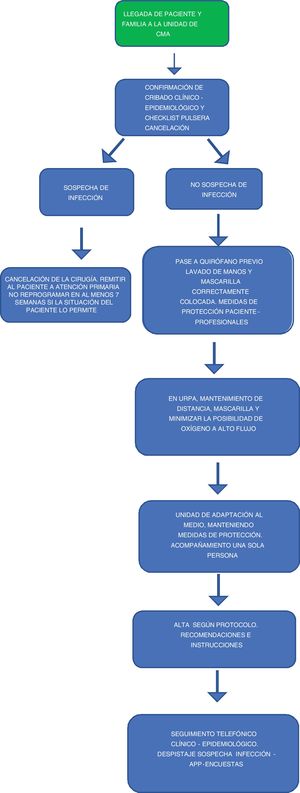
Fig. 2 demonstrates the circuit of ambulatory surgery patients.
Training in ambulatory surgery units and SARS-CoV-2In the same way that training in the prevention of infection has become widespread, we cannot forget that medical residents and undergraduate students must continue to learn and complete their rotations21. In addition, medical training should include the use of new information technologies to make telemedicine and teleconsultation effective20,34,35. Another valuable tool is the use of social networks like Twitter as a means to discuss and share scientific evidence36, which is increasingly demonstrating the importance of global communication to defeat the virus.
Final considerationsAt this point in the pandemic, in which surgery must continue, ambulatory surgery is an example of quality, efficient medical care that should be established as the center of scheduled surgical activity, and care circuits should be redesigned around it.
The ambulatory surgery unit must be clearly defined as a perfectly separate COVID-free circuit, with a specific team of medical professionals who could be distributed in different work shifts. The safety of patients and staff must be prioritized, and patients and procedures should be selected through the use of guidelines that we have proposed.
“Single-visit” preoperative consultations should be encouraged and telemedicine tools promoted, without forgetting undergraduate/resident training and the great opportunities offered by new and developing communication technologies.
Coordinator of the workgroup:
Salvador Morales Conde, Hospital Universitario Virgen del Rocío, Sevilla
Members of the workgroup:
Estíbaliz Álvarez Peña, Hospital Universitario La Paz, Madrid
Mario Álvarez Gallego, Hospital Universitario La Paz, Madrid
José Manuel Aranda Narváez, Hospital regional Universitario, Málaga
Josep María Badia, Hospital General de Granollers, Barcelona
José María Balibrea, Hospital Clinic, Barcelona
Sandra García Botella, Hospital Clínico San Carlos, Madrid
Xavier Guiro, Hospital Parc Taulí, Barcelona
Eloy Espín Basany, Hospital Vall d’Hebron, Barcelona
Esteban Martín Antona, Hospital Clínico San Carlos, Madrid
Elena Martín Pérez, Hospital Universitario de la Princesa, Madrid
Sagrario Martínez Cortijo, Hospital de Talavera de la Reina, Toledo
Isabel Pascual Miguelañez, Hospital Universitario La Paz, Madrid
Lola Pérez Díaz, Hospital Gregorio Marañón, Madrid
José Luis Ramos Rodríguez, Hospital Universitario de Getafe, Madrid
Inés Rubio Pérez, Hospital Universitario La Paz, Madrid
Raquel Sánchez Santos, Complejo Hospitalario de Vigo, Vigo
Please cite this article as: Morales-García D, Docobo-Durantez F, Capitán Vallvey JM, Suarez-Grau JM, Campo-Cimarras ME, González-Vinagre S, et al. Consenso de la sección de cirugía mayor ambulatoria de la Asociación Española de Cirujanos sobre el papel de la cirugía mayor ambulatoria en la pandemia SARS-CoV-2. Cir Esp. 2022;100:115–124.