Thromboelastography (TEG) provides an in vivo assessment of viscoelastic clot strength in whole blood compared with a conventional coagulation test (CCT), which may not reflect the influence of platelets. The aim of this study was to compare TEG vs CCT in trauma patients stratified by mechanism of injury (MOI) and pre-existing coagulation status.
MethodsA retrospective, observational study of 230 polytrauma patients admitted to a University Hospital Level 1 Trauma Center, with TEG and CCT on admission stratified by MOI: multiple trauma (MT), isolated traumatic brain injury (TBI) or MT+TBI. Statistical analysis included correlation between TEG and CCT in all groups and a subgroup analysis of anticoagulated patients. Data were analyzed with ANOVA, Spearman and lineal regression when appropriate. Statistical significance was accepted at P<.05.
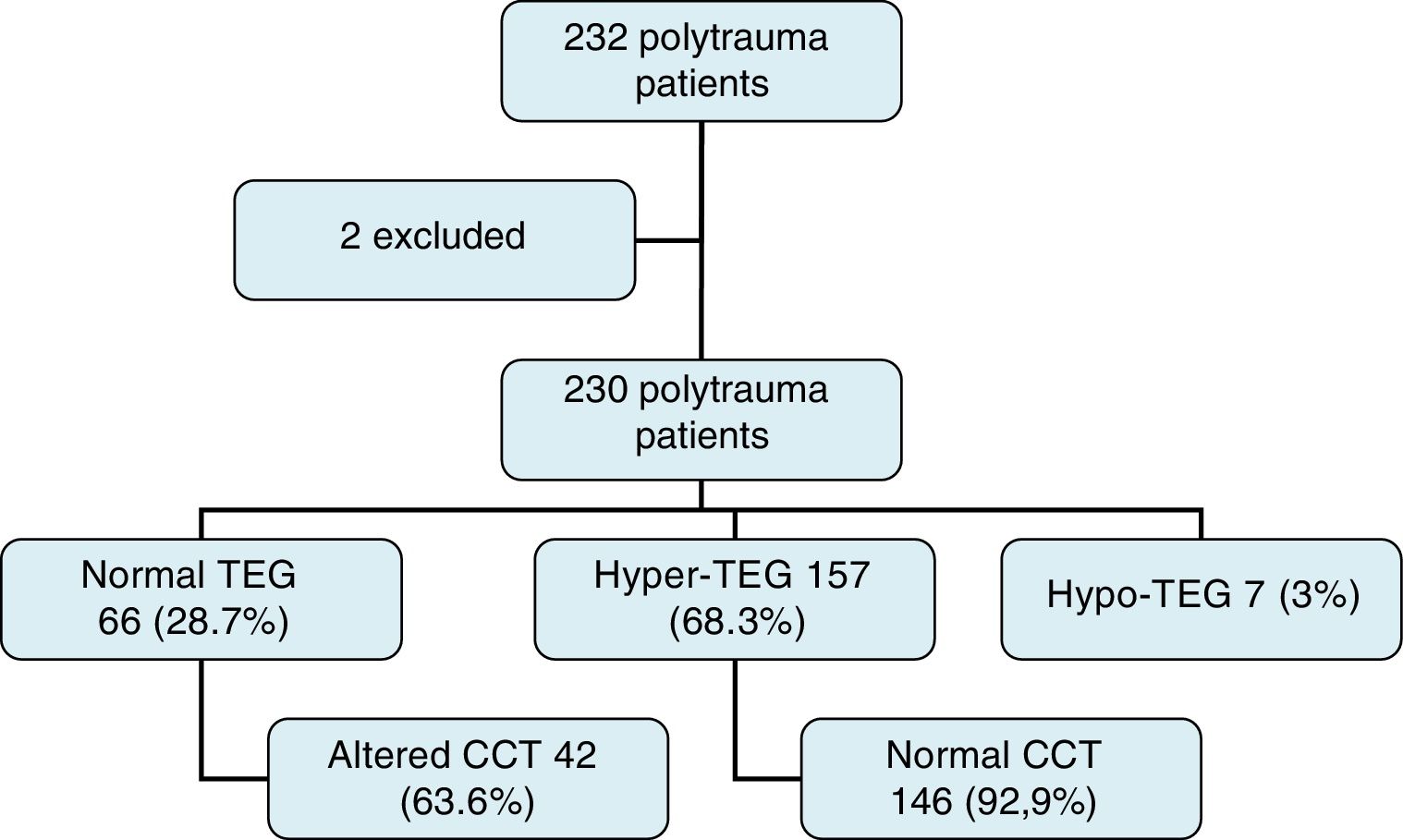
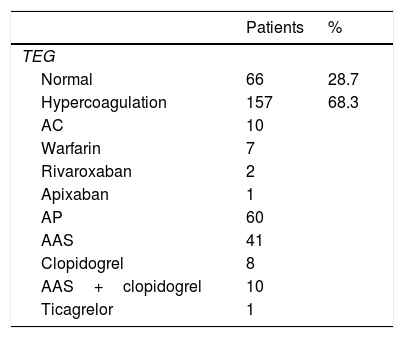
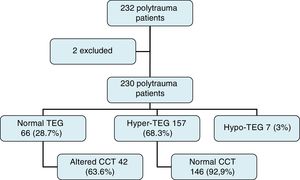
ResultsTEG was normal in 28.7%, hypercoagulable in 68.3% and hypocoagulable in 7%. There was no difference in TEG status among the groups. The coagulation status was not affected by age, ISS or shock. The CCT was abnormal in 63.6% of patients with normal TEG. Normal or hypercoagulable-TEG was found in 21 of 23 patients on Coumadin who had elevated international normalized ratio (INR) and in 10 of 11 patients on NOAC. An analysis of the 23 patients on Coumadin stratified by INR showed a normal or hypercoagulable-TEG in 21 of 23 patients. Only two patients had a hypocoagulable-TEG. Mortality was 5.2% (58.3% severe TBI).
ConclusionsTEG is more useful than CCT in polytrauma patients, including patients on anticoagulants. TBI could increase the incidence of hypercoagulability in trauma. CCT are not useful from the standpoint of treatment.
TEG mide in vivo la potencia viscoelástica de la coagulación en sangre total; comparado con los TCC, estos no reflejan la influencia plaquetaria. Nuestro objetivo fue comparar TEG vs TCC en pacientes politraumáticos estratificados por mecanismo lesional (ML) y estado previo de coagulación.
MétodosEstudio retrospectivo y observacional de 230 pacientes politraumáticos, en un Hospital Universitario Nivel 1 de Trauma, realizándose TEG y TCC a su llegada. Los pacientes se dividieron según ML: multitraumatismo (MT), traumatismo craneoencefálico (TCE) aislado y MT+TCE. Se analizó la correlación entre TEG-TCC en todos los grupos y un análisis de subgrupo de los pacientes anticoagulados, utilizándose ANOVA, Spearman y regresión lineal según correspondía. Se definió la significación estadística como p<0,05.
ResultadosCoagulación según TEG: normal (28,7%), hipercoagulación (68,3%) e hipocoagulación (3%). No hubo diferencias en parámetros de coagulación por TEG entre grupos. La coagulación no estaba afectada por edad, ISS o presencia de shock. Los TCC estaban alterados en 63,6% pacientes con TEG normal. La TEG fue normal o hipercoagulación en 21/23 pacientes anticoagulados con warfarina e INR elevado, y en 10/11 pacientes anticoagulados con NAO. TEG fue normal o hipercoagulación en 21/23 pacientes anticoagulados con warfarina, estratificado por INR (2 pacientes), y 2 pacientes presentaron TEG con hipocoagulación. La mortalidad fue del 5,2% (58,3% TCE severo).
ConclusionesTEG es más útil que los TCC en pacientes politraumáticos, incluyendo a pacientes anticoagulados. El TCE podría aumentar la incidencia de hipercoagulabilidad en traumatismos. Los TCC no son útiles des del punto de vista terapéutico.
Thromboelastography (TEG) was first described by Hartert1 in Germany in 1948, as a way to assess alterations in coagulation factors. It was introduced in the United States in the 1980s for its usefulness in liver transplantation2 and progressively began to be used in other areas, such as cardiothoracic surgery,3 aortic surgery4 and, finally, in surgical patients, in general.5
Very shortly after tissue aggression, polytrauma patients are affected by what is called trauma-induced coagulopathy.6 This state of hypo- or hypercoagulability cannot be easily detected with a conventional coagulation test (CCT), which include international normalized ratio (INR), prothrombin time (PT) and partial thromboplastin time (PTT). For this reason, TEG began to be used in the management of polytrauma patients, showing results compatible with hypo- or hypercoagulability, while CCT was normal.7 Obtaining this type of information is of utmost importance in the management of polytrauma patients, and even more important in patients under treatment with conventional anticoagulants, such as warfarin or new oral anticoagulants (NOA), as it may allow us to conduct individualized treatments aimed at restoring hemostasis.
On the other hand, with the advent of NAO and antiplatelet agents8 (AP), the number of anticoagulant treatments available is increasing, the majority of which are not analytically monitored with CCT. It is in this type of patients where TEG can be of greater help, although there are some studies that speak of limited use in patients with NAO.9
Currently, there are two ways to conduct a dynamic study of clot formation: TEG (TEG®) and thromboelastometry (ROTEM®). Both produce a graphic evaluation of the kinetics of clot formation in all its phases (initiation, propagation, formation and dissolution).10 A recent meta-analysis10 on the use of TEG® and ROTEM® in patients with bleeding has shown a reduction in mortality, need for transfusion of blood products, bleeding and presence of renal failure requiring dialysis. In addition, no differences were found between TEG and ROTEM.
The aim of this study was to analyze TEG parameters in patients with multiple trauma and to observe its correlation with CCT results, in addition to observing the differences in polytrauma patients treated with oral anticoagulants (warfarin and NAO).
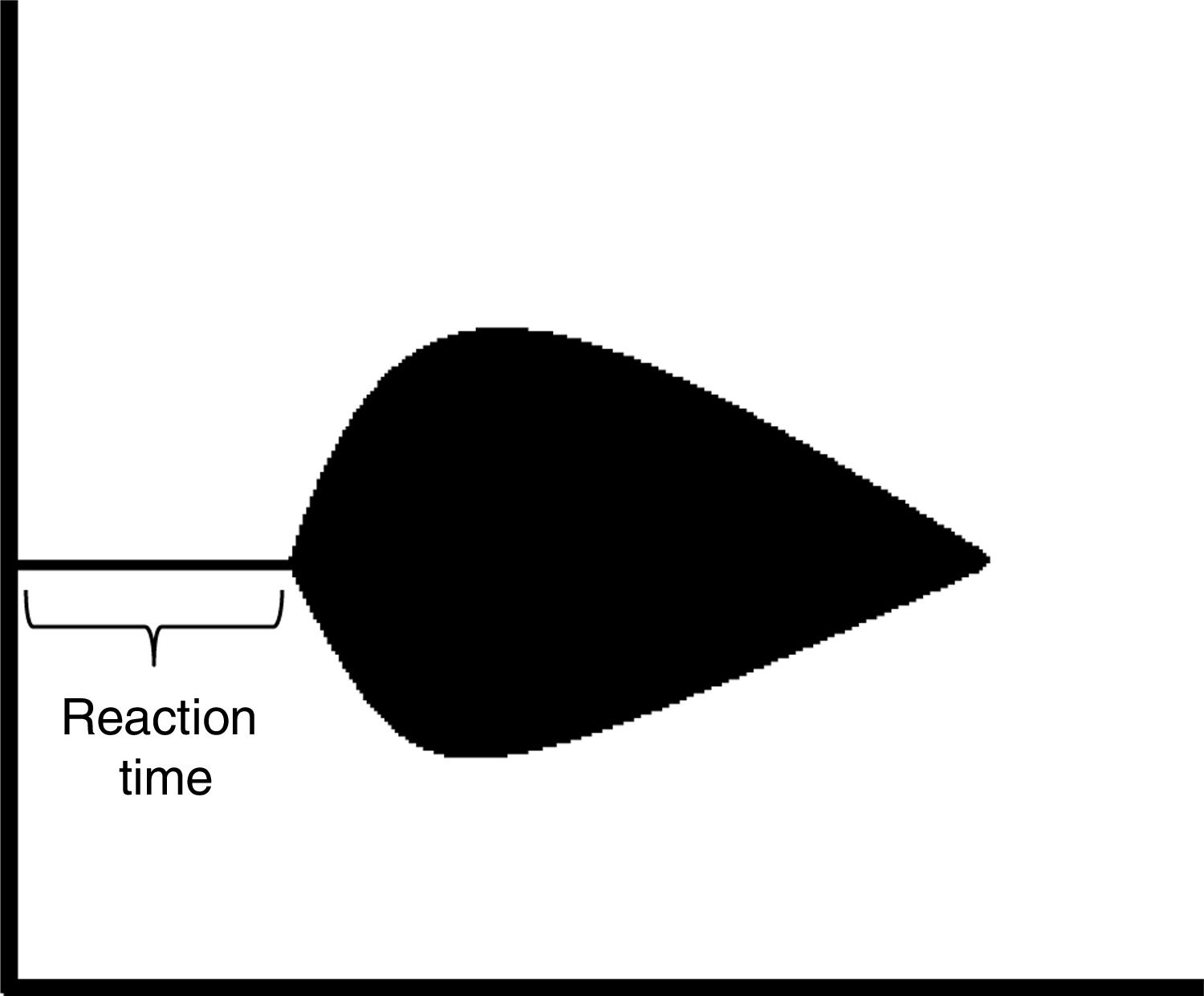
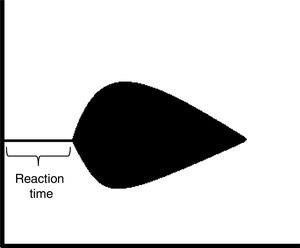
MethodsThis is a retrospective, observational study of 230 polytrauma patients admitted to NYU Winthrop Hospital, Level 1 Trauma Center verified by the American College of Surgeons, located in Mineola (Long Island), New York, USA. The study period was from January 1, 2016 to December 31, 2016. Variables were recorded for TEG (using the TEG® Haemonetics Corp., Braintree, MA, USA) and CCT (INR, PT and PTT) as continuous variables of all the patients diagnosed with multiple trauma (as a code, alert or consultation), upon arrival. The state of hyper- or hypocoagulability was defined according to the TEG reaction time (R) (Fig. 1). R<5s was considered hypercoagulability (hyper-TEG), R>10s hypocoagulability (hypo-TEG) and R from 5 to 10s was coagulation in normal range (normal-TEG). Data were collected for demographics, comorbidities, mechanism of injury (MI), Injury Severity Score (ISS), suspected hypovolemic shock (defined as arterial blood pressure [BP] lower than 105mmHg in patients over 65 years of age and BP below 95mmHg in patients aged 65 or younger), use of anticoagulants (AC, warfarin or NAO) and use of AP. The patients were divided into three groups according to MI: multiple trauma (MT) (injury to two or more systems, excluding traumatic brain injury [TBI]), TBI and MT+TBI.
The primary objective was to compare TEG vs CCT in polytrauma patients, stratified by MI and previous coagulation state. The statistical analysis included a correlation between the TEG and CCT results in all groups, in addition to a subgroup analysis of patients on anticoagulant therapy. The data were analyzed with ANOVA, Spearman and linear regression, as appropriately. Statistical significance was defined as P<.05.
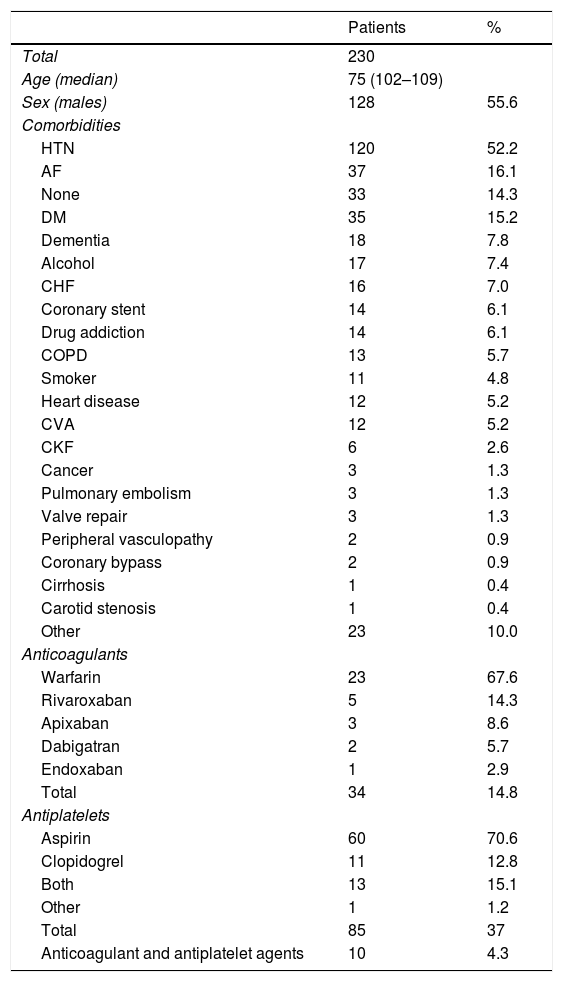
ResultsA total of 232 polytrauma patients were identified. Two were excluded due to incomplete information, so that a total of 230 patients were included (Fig. 2). 55.6% were male, with a median age of 75 years (9–102). The most frequent comorbidities were hypertension, atrial fibrillation and diabetes mellitus (Table 1). A total of 129 patients were in some type of treatment with AP (n=85), AC (n=34) or both (n=10). The most frequent oral AC was warfarin and the most frequent AP, aspirin (Table 1).
Clinical Data.
| Patients | % | |
|---|---|---|
| Total | 230 | |
| Age (median) | 75 (102–109) | |
| Sex (males) | 128 | 55.6 |
| Comorbidities | ||
| HTN | 120 | 52.2 |
| AF | 37 | 16.1 |
| None | 33 | 14.3 |
| DM | 35 | 15.2 |
| Dementia | 18 | 7.8 |
| Alcohol | 17 | 7.4 |
| CHF | 16 | 7.0 |
| Coronary stent | 14 | 6.1 |
| Drug addiction | 14 | 6.1 |
| COPD | 13 | 5.7 |
| Smoker | 11 | 4.8 |
| Heart disease | 12 | 5.2 |
| CVA | 12 | 5.2 |
| CKF | 6 | 2.6 |
| Cancer | 3 | 1.3 |
| Pulmonary embolism | 3 | 1.3 |
| Valve repair | 3 | 1.3 |
| Peripheral vasculopathy | 2 | 0.9 |
| Coronary bypass | 2 | 0.9 |
| Cirrhosis | 1 | 0.4 |
| Carotid stenosis | 1 | 0.4 |
| Other | 23 | 10.0 |
| Anticoagulants | ||
| Warfarin | 23 | 67.6 |
| Rivaroxaban | 5 | 14.3 |
| Apixaban | 3 | 8.6 |
| Dabigatran | 2 | 5.7 |
| Endoxaban | 1 | 2.9 |
| Total | 34 | 14.8 |
| Antiplatelets | ||
| Aspirin | 60 | 70.6 |
| Clopidogrel | 11 | 12.8 |
| Both | 13 | 15.1 |
| Other | 1 | 1.2 |
| Total | 85 | 37 |
| Anticoagulant and antiplatelet agents | 10 | 4.3 |
CVA, cerebrovascular accident; DM, diabetes mellitus; COPD, chronic obstructive pulmonary disease; AF, atrial fibrillation; HTN, hypertension; CHF, congestive heart failure; CRF, chronic renal failure.
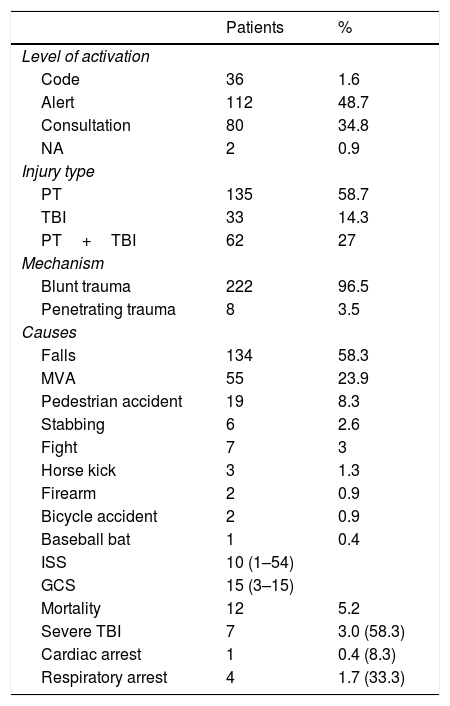
The characteristics of the injuries are shown in Table 2. The most frequent activation level was alert (112 patients). The majority of patients presented MT (58.7%), and blunt trauma was present in 96.5% of the patients, with the most frequent causes being falls (58.3%) and car incidents (23.9%). Twelve patients died, representing 5.2% of the total, and 58.3% of these due to severe TBI. The average ISS was 14±9.58 (Table 2).
Information About Trauma Injuries.
| Patients | % | |
|---|---|---|
| Level of activation | ||
| Code | 36 | 1.6 |
| Alert | 112 | 48.7 |
| Consultation | 80 | 34.8 |
| NA | 2 | 0.9 |
| Injury type | ||
| PT | 135 | 58.7 |
| TBI | 33 | 14.3 |
| PT+TBI | 62 | 27 |
| Mechanism | ||
| Blunt trauma | 222 | 96.5 |
| Penetrating trauma | 8 | 3.5 |
| Causes | ||
| Falls | 134 | 58.3 |
| MVA | 55 | 23.9 |
| Pedestrian accident | 19 | 8.3 |
| Stabbing | 6 | 2.6 |
| Fight | 7 | 3 |
| Horse kick | 3 | 1.3 |
| Firearm | 2 | 0.9 |
| Bicycle accident | 2 | 0.9 |
| Baseball bat | 1 | 0.4 |
| ISS | 10 (1–54) | |
| GCS | 15 (3–15) | |
| Mortality | 12 | 5.2 |
| Severe TBI | 7 | 3.0 (58.3) |
| Cardiac arrest | 1 | 0.4 (8.3) |
| Respiratory arrest | 4 | 1.7 (33.3) |
MVA, motor vehicle accident; GCS, Glasgow Coma Score; ISS, Injury Severity Score; PT, polytrauma; TBI, traumatic brain injury.
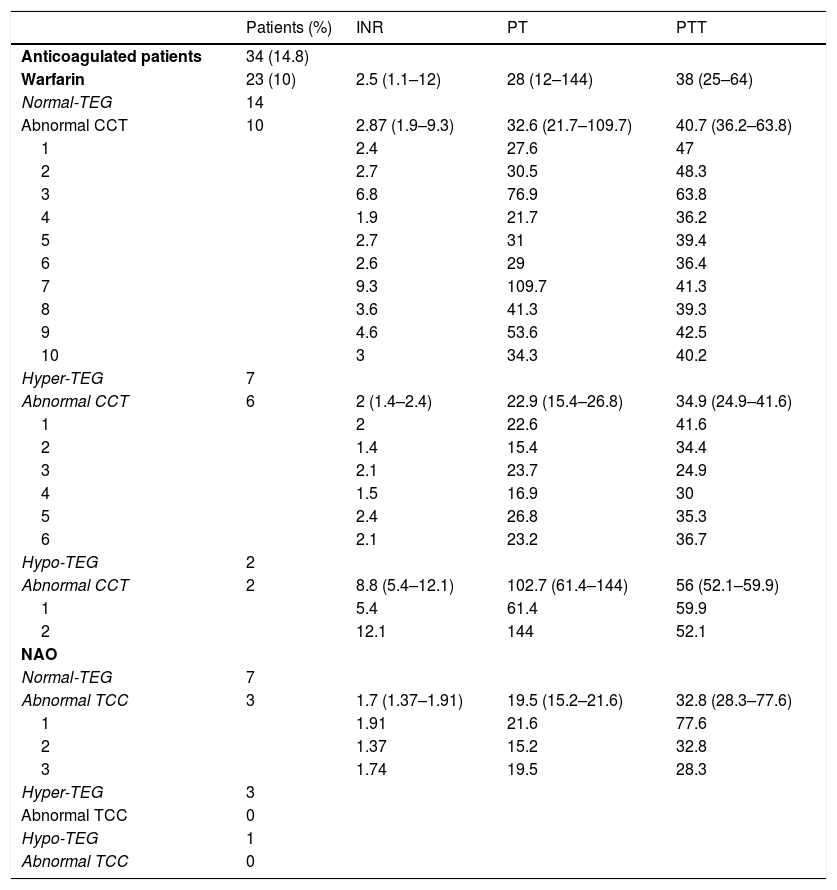
According to the TEG, the coagulation status was normal in 66 patients (28.7%), hypercoagulation in 157 (68.3%) and hypocoagulation in only 7 patients (3%) (Table 3) (Fig. 2). There were no differences in coagulation parameters by TEG among the three groups (P>.05). The coagulation status was not affected by age, ISS or the presence of shock. The CCT was altered in 42 of 66 patients (63.6%) with normal TEG, distributed as follows: 23 patients with altered PT or INR and 19 patients with altered PTT. Likewise, within the hyper-TEG group, 146 patients had normal CCT. Curiously, the TEG test was either normal or hypercoagulation in 21 of 23 patients treated with warfarin and high INR as well as 10 of 11 patients treated with NAO (Table 4). The analysis of the 23 patients with warfarin therapy, stratified by INR, showed normal TEG or hypercoagulation in 21/23 patients with an average INR of 2.9 (R: 1.9–9.3) in patients with normal TEG, and 2 (R: 1.4– 2.4) in patients with hyper-TEG (Table 4). Only two patients presented a TEG with hypocoagulation, with a mean INR of 8.8 (R: 5.4–12.1).
TEG and CCT Results in Patients With Anticoagulant Treatment.
| Patients (%) | INR | PT | PTT | |
|---|---|---|---|---|
| Anticoagulated patients | 34 (14.8) | |||
| Warfarin | 23 (10) | 2.5 (1.1–12) | 28 (12–144) | 38 (25–64) |
| Normal-TEG | 14 | |||
| Abnormal CCT | 10 | 2.87 (1.9–9.3) | 32.6 (21.7–109.7) | 40.7 (36.2–63.8) |
| 1 | 2.4 | 27.6 | 47 | |
| 2 | 2.7 | 30.5 | 48.3 | |
| 3 | 6.8 | 76.9 | 63.8 | |
| 4 | 1.9 | 21.7 | 36.2 | |
| 5 | 2.7 | 31 | 39.4 | |
| 6 | 2.6 | 29 | 36.4 | |
| 7 | 9.3 | 109.7 | 41.3 | |
| 8 | 3.6 | 41.3 | 39.3 | |
| 9 | 4.6 | 53.6 | 42.5 | |
| 10 | 3 | 34.3 | 40.2 | |
| Hyper-TEG | 7 | |||
| Abnormal CCT | 6 | 2 (1.4–2.4) | 22.9 (15.4–26.8) | 34.9 (24.9–41.6) |
| 1 | 2 | 22.6 | 41.6 | |
| 2 | 1.4 | 15.4 | 34.4 | |
| 3 | 2.1 | 23.7 | 24.9 | |
| 4 | 1.5 | 16.9 | 30 | |
| 5 | 2.4 | 26.8 | 35.3 | |
| 6 | 2.1 | 23.2 | 36.7 | |
| Hypo-TEG | 2 | |||
| Abnormal CCT | 2 | 8.8 (5.4–12.1) | 102.7 (61.4–144) | 56 (52.1–59.9) |
| 1 | 5.4 | 61.4 | 59.9 | |
| 2 | 12.1 | 144 | 52.1 | |
| NAO | ||||
| Normal-TEG | 7 | |||
| Abnormal TCC | 3 | 1.7 (1.37–1.91) | 19.5 (15.2–21.6) | 32.8 (28.3–77.6) |
| 1 | 1.91 | 21.6 | 77.6 | |
| 2 | 1.37 | 15.2 | 32.8 | |
| 3 | 1.74 | 19.5 | 28.3 | |
| Hyper-TEG | 3 | |||
| Abnormal TCC | 0 | |||
| Hypo-TEG | 1 | |||
| Abnormal TCC | 0 |
Normal PT: 10–12s; normal INR: 0.9–1.2; normal PTT: 26–36s; abnormal PT: >12s; abnormal INR: >1.2; abnormal PTT: >36s.
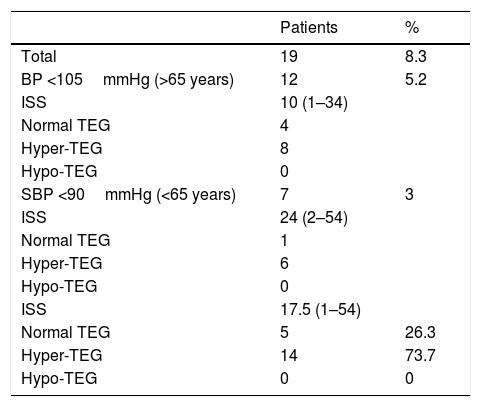
In the group of patients with hypovolemic shock (Table 5), 14 of 19 patients presented hyper-TEG (73.7%), and only five patients had a TEG compatible with normality. The ISS was higher than in the remaining groups, with a median of 17.5 (R: 1–54).
TEG Results in Patients in Shock.
| Patients | % | |
|---|---|---|
| Total | 19 | 8.3 |
| BP <105mmHg (>65 years) | 12 | 5.2 |
| ISS | 10 (1–34) | |
| Normal TEG | 4 | |
| Hyper-TEG | 8 | |
| Hypo-TEG | 0 | |
| SBP <90mmHg (<65 years) | 7 | 3 |
| ISS | 24 (2–54) | |
| Normal TEG | 1 | |
| Hyper-TEG | 6 | |
| Hypo-TEG | 0 | |
| ISS | 17.5 (1–54) | |
| Normal TEG | 5 | 26.3 |
| Hyper-TEG | 14 | 73.7 |
| Hypo-TEG | 0 | 0 |
Hyper-TEG: R<5s; Hypo-TEG: R>10s; normal TEG: R=5–10s.
TEG, thromboelastography; ISS, Index Severity Score; SBP, systolic blood pressure.
The subgroup of patients with TBI was analyzed, since this was the major cause of mortality in our sample. A total of 95 patients presented with TBI: in 33 as the only MI, and in 62 in the context of MT. Mild TBI was the most frequent (GCS 13–15), with 27 in the TBI alone group and 46 in the TBI+MT group. When the TEG results in this patient subgroup were analyzed, the presence of hyper-TEG was observed in 70 of 95 patients with TBI (73.6%). Hypo-TEG was only detected in two patients with TBI.
DiscussionTEG provides complete coagulation studies for polytrauma patients. It measures the viscoelastic properties of blood in a dynamic manner, including all the phases of coagulation and fibrinolysis and also takes into account the role of platelets in hemostasis, unlike CCT. For this, 0.36mL of total blood is required, which is placed in a vial with kaolin (activating the coagulation cascade) and an angled pin is in contact with it. The changes in physical characteristics for clot formation is translated to a graph for subsequent interpretation.11
In this study, we compared the TEG (according to R time) and CCT results in 230 polytrauma patients. We observed that TEG allowed us to detect a state of hypercoagulability in the majority of our patients (68.3%), even if they were being treated with AC or AP. In contrast, CCT did not detect any hypercoagulability states in any of the patients. No differences were observed in the coagulation results of TEG or CCT, nor in the MI or the ISS.
It should be noted that, in 66 patients with normal TEG, 42 had altered CCT, 23 altered PT or INR, and 19 patients altered PTT. This may be due to the fact that a high number of these patients were in treatment with AC and AP, and these can cause variability in the CCT results. In addition, TEG-kaolin was used in our study, which uses the intrinsic pathway of coagulation to a greater degree and is less sensitive than warfarin,9 which could contribute to these results. There are other factors that can alter the viscoelastic test results, making their results normal. Some examples include hypothermia, acidosis, von Willebrand disease, inhibition or dysfunction of platelets and certain NAO.12 Within the group of patients with suspected hypovolemic shock, it is noteworthy that none of them presented TEG results compatible with hypocoagulation, as might be expected since these patients have a high probability of bleeding. In contrast, the vast majority of them (73.7%) had hypercoagulation TEG. This phenomenon and, as in the remaining patients, the predominance of a hypercoagulable state could be explained by the presence of trauma-induced coagulopathy, since it is known that patients with mild polytrauma (ISS<15) tend more toward states of hypercoagulation, while patients with higher ISS usually present with states of hypocoagulation and hyperfibrinolysis.13
An analysis was conducted of the patients with TBI, since this group had the most prevalent cause of mortality in our series. When TEG parameters were analyzed, we observed that these were identical to the remaining patients and, therefore, there were no differences in terms of coagulation status, which would justify increased mortality.
The TEG only showed parameters for hypocoagulation in seven patients. Out of these, only two were in treatment with AC, and these patients presented the most altered CCT: INR 8.8 (R: 5.4–12.1), PT 102.7 (61.4–144) and PTT 56 (52.1–59.9). Thus, in patients under CA treatment who present hypocoagulation parameters in CCT, but normal TEG, this is possibly due to alterations of the AC drugs themselves; therefore, they can be reversed with the respective antidotes. In contrast, in patients with severely elevated PTT, INT and PT as well as TEG compatible with hypocoagulation, we can attribute these changes to trauma-induced coagulopathy, and it is this type of patients who may need blood products for reversal. In this group, there were no patients in hypovolemic shock, so, in the remaining five patients, hypocoagulation could be attributed to the polytrauma itself.
In 2014, a consensus was reached in Philadelphia on the use of viscoelastic tests in the resuscitation of polytrauma patients.12 Similar to our study, one of its conclusions was that only viscoelastic tests are able to detect a hypercoagulation state. In addition, other conclusions were that the transfusion of blood products would be contraindicated in patients with hypercoagulability and that only viscoelastic tests are able to detect hyperfibrinolysis states.
Another advantage to the use of TEG for treatment is that it is aimed at polytrauma patients. A systematic review published in 201514 concluded that within the group of patients with TEG compatible with hypocoagulation are those who will require a greater number of transfusions; also, patients with fibrinolysis will have a higher mortality rate. Likewise, the same review included cost-effectiveness studies, which concluded that viscoelastic tests provide a savings in the cost of polytrauma patient care, mostly due to the savings of transfusions.
The TEG test is more useful than CCT in polytrauma patients, including patients being treated with warfarin or NAO. TBI could increase the incidence of hypercoagulability in trauma. It can be concluded that CCT is not useful from a therapeutic point of view and should be abandoned as a standard study to evaluate coagulation. More research is required to better manage patients with abnormal CCT and TBI but with normal TEG or hypercoagulation, in view of the medical–legal consequences associated with the non-treatment of abnormal CCT.
Conflicts of InterestThe authors have no conflicts of interest to declare.
Please cite this article as: Tur Martínez J, Petrone P, Axelrad A, Marini CP. Comparación entre tromboelastografía y test de coagulación convencionales: ¿deberíamos abandonar los test de coagulación convencional en el paciente politraumatizado? Cir Esp. 2018;96:443–449.
Presented orally and distinguished as one of the three best studies at the 21st Annual Meeting of Surgery of the AEC, 18–20 October, 2017, in Malaga, Spain.