It has been proved that a breast reconstruction after a mastectomy has a great psycho-social impact on patients. For this reason, it is increasingly done in a greater percentage of cases. There are two major groups of reconstructive techniques: a reconstruction with implants and a reconstruction with autologous tissue of the patient. In order to make a more objective assessment of the results, it is important to know how satisfied these patients are with the results. Therefore, we performed a study using Q-BREAST, the aim of which is to analyze the satisfaction of mastectomized patients according to the different surgical reconstruction techniques.
MethodsA retrospective, descriptive and observational study of patients reconstructed in our service from 2008 to 2011 was carried out. Patient satisfaction levels were compared according to the surgical technique used in breast reconstruction using the Q-BREAST test, which was mailed to them.
ResultsThere are no statistical differences in the levels of satisfaction in terms of age, type of mastectomy done, coadjutant treatment or existence of complications. Higher levels of satisfaction are observed in patients reconstructed with autologous tissue versus implants (P=.028).
ConclusionsPatients reconstructed with autologous tissue have higher levels of satisfaction than those reconstructed with implants.
La reconstrucción mamaria tras mastectomía ha demostrado tener un impacto psicosocial muy importante en las pacientes. Existen 2 grandes grupos de técnicas reconstructivas: la reconstrucción con implantes y la reconstrucción con tejido autógeno de la paciente. Para poder realizar una valoración más objetiva de los resultados es importante conocer la satisfacción que presentan las mismas, por lo que se decide realizar un estudio empleando el Q-BREAST cuyo objetivo es analizar la satisfacción de las pacientes mastectomizadas en función de las diferentes técnicas quirúrgicas de reconstrucción.
MétodosSe realiza un estudio retrospectivo, descriptivo y observacional de las pacientes reconstruidas en nuestro servicio del 2008 al 2011. Se comparan los niveles de satisfacción de las pacientes según la técnica quirúrgica empleada en la reconstrucción de mama mediante el empleo del test Q-BREAST, que se les envió por correo.
ResultadosSe obtiene una respuesta al Q-BREAST de 90 pacientes. No se encuentran diferencias estadísticas en los niveles de satisfacción en relación con la edad, el tipo de mastectomía realizada, el tratamiento coadyuvante y la existencia de complicaciones. Sí se observan unos niveles superiores de satisfacción en las pacientes reconstruidas con tejido autógeno frente a los implantes (p=0,028).
ConclusionesLas pacientes reconstruidas con tejido autógeno presentan niveles más altos de satisfacción que las reconstruidas con implantes.
Breast cancer is currently a disease of considerable interest given its high incidence in developed countries.1 Its surgical treatment has evolved from the radical mastectomy of Halsted2 to the current trend of performing breast-conserving surgery whenever possible. However, mastectomy is often necessary.
To minimize the psychological effect of the resulting change in breast shape,3 the possibility of breast reconstruction is offered to these patients. Breast reconstruction methods can be divided into 2 groups:
- –
Reconstruction with implants: either with direct prosthesis or in two stages with the use of an expander and subsequent replacement with a definitive prosthesis.
- –
Reconstruction with autogenous tissue: pedicle flaps (latissimus dorsi with or without underlying prosthesis) and distance flaps or “free flaps” require microsurgical techniques.
Since 1983, when the British National Health Service recommended the assessment of patient satisfaction in order to determine the quality of the health service provided,4 many surveys have proliferated to analyze the efficacy and effectiveness of healthcare interventions.
In 2007, Pusic et al.5 performed a systematic review of all the published questionnaires that were answered by patients after breast surgery. Of these, only the Breast-Related Symptoms Questionnaire (BRSQ), which assesses results after breast reduction, demonstrated adequate development and validation.
Therefore, these same authors published another article6 in which they presented a new questionnaire, the Q-BREAST, which made up for the shortcomings of the previous surveys and presented adequate development and validation.
After confirming this growing relevance that is given to the opinion of patients about their own surgical results, we decided to conduct a study using the Q-BREAST, which aims to analyze the satisfaction of mastectomy patients according to different surgical reconstruction techniques.
Methods- a.
Study design: we carried out a retrospective, descriptive, observational study that included all patients who had undergone breast reconstruction secondary to cancer surgery at the Reconstructive and Plastic Surgery Department of the Hospital Universitario Miguel Servet from January 1, 2008 until December 31, 2011. Excluded from the study were those patients who, at the time of data collection, had not yet completed the reconstructive process, presented active breast cancer disease, or had deceased.
- b.
Instrument for measurement: the satisfaction data were obtained with the Q-BREAST test, which is comprised of 2 general topics (or domains), with 3 subsections each:
- 1.
Patient satisfaction
- -
Satisfaction with the breast
- -
Satisfaction with the general result
- -
Satisfaction with the medical care
- -
- 2.
Patent quality of life
- -
Physical wellness
- -
Psychosocial wellness
- -
Sexual wellness
- -
- 1.
- c.
Field work: the Q-BREAST test was distributed by mail in May 2013, together with an informational letter explaining the study and an informed consent form, to all the patients of the study. A pre-paid envelope was included to mail the completed questionnaire. One month later, the patients who had not submitted the questionnaire were contacted by telephone, and they were encouraged to participate.
- d.
Variables for study: age, type of mastectomy, type of reconstructive surgery used, coadjuvant treatment and existence of complications.
The object of the study was the breast reconstruction performed and patient satisfaction. Because bilateral cases have frequently been treated with different reconstruction types, each of these patients have been considered 2 patients treated surgically for one breast.
Statistical AnalysisThe data obtained were input into an Excel spreadsheet and then imported to SPSS V20.0 for statistical analysis.
For the study of the variables that presented normal distribution, the Student's t test was for the comparison between 2 quantitative variables and the chi-squared for qualitative variables, using ANOVA techniques (analysis of univariate variance) if there was more than one independent variable.
In the case of variables of normal distribution that were divided into small groups, the normality within each group was recalculated with the Shapiro–Wilk test (for samples less than 50 cases) or the Kolmogorov–Smirnov test (for larger samples). Those who did not follow a normal distribution were interpreted with a non-parametric test.
The non-parametric test used in the comparison of 2 variables was the Mann–Whitney U test. When there were more than 2 independent variables, we used the Kruskall–Wallis test or the analysis of the range variance.
Results- a.
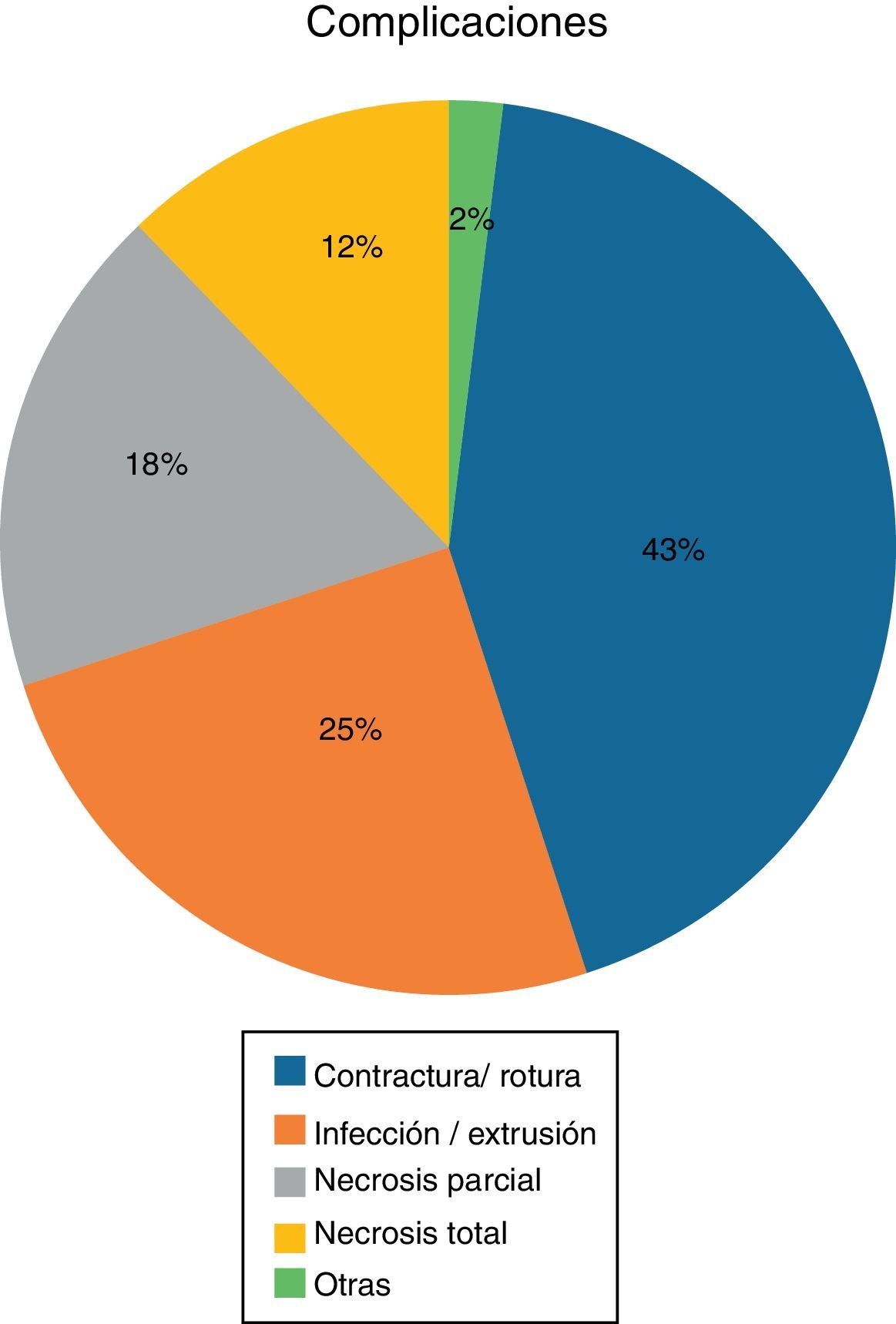
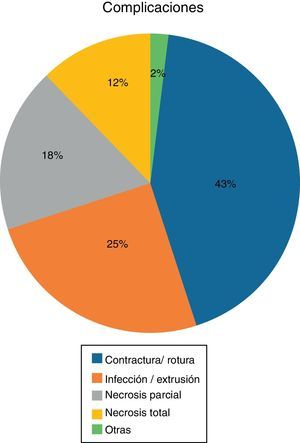
Degree of participation and description of the series: The rate of response was 60.7% as in the end a total of 90 patients responded to the letter out of the 143 included, 15 of which had bilateral reconstruction, so the total number of cases of breast reconstruction that responded to the Q-Breast was 105.Some of the patients who did not fill out the questionnaire explained that their reasons for not participating in the study included a desire to forget the entire traumatic oncologic-reconstructive process, or due to lack of time to respond.Patient age ranged from 29 to 77, with a mean of 49.2±9, which we divided into 3 groups: younger than 45, 45 to 55 and older than 55.In almost half of cases (46%), a modified radical mastectomy was used. In 29% of cases, simple mastectomy was done with an intraoperative sentinel lymph node study, and in the remaining 25% simple mastectomy was done exclusively or subcutaneous mastectomy with no associated sentinel lymph node surgery.According to the type of reconstruction done, 70% of the cases were reconstructed with implants and 30% with autogenous tissue.As for coadjuvant treatment, chemotherapy was administered in 64% of patients, chest wall radiotherapy over breast site in 25% and axillary in 13%. The percentage of patients who received hormone therapy was 74%.When we evaluated the coadjuvant treatment of each patient overall, only 6% did not need any type of coadjuvant treatment, while 9% received the 4 types of adjuvant treatment: chemotherapy, breast radiotherapy, axillary radiotherapy and hormone therapy. The most common treatment was chemotherapy plus hormone therapy (31%), followed by treatment with hormone therapy alone (20%).The rate of appearance of complications was 25%, divided according to Fig. 1.
- b.
Degree of satisfaction and overall quality of life: to assess the levels of patient satisfaction, data were used from the Q-BREAST questionnaire, meaning, the score obtained from each patient in the domain of “patient satisfaction”, the “quality of life” domain and in the weighted sum of both, which we call “total or overall satisfaction”.
- c.
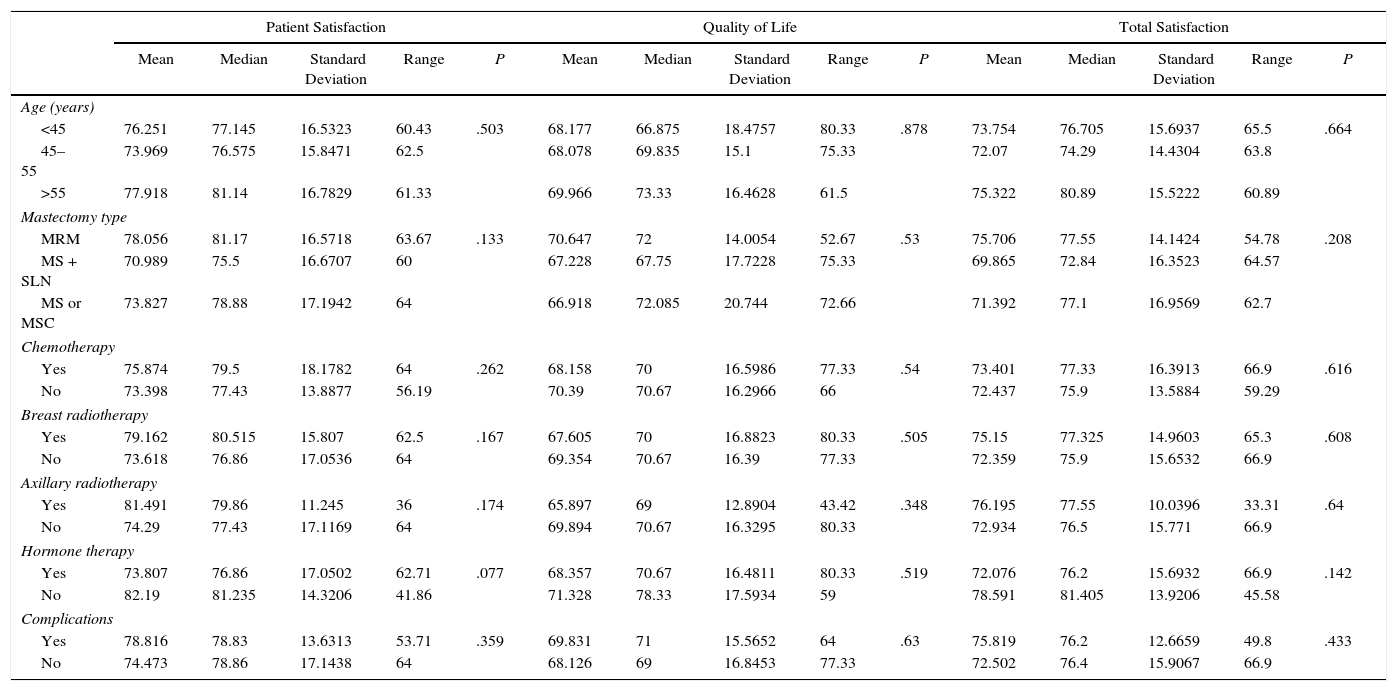
Assessment of satisfaction according to variables not related with reconstruction: no significant differences were found in the total levels of patient satisfaction according to age (P=.6), type of mastectomy (P=.2), coadjuvant treatment: chemotherapy (P=.61), breast radiotherapy (P=.61), axillary radiotherapy (P=.64) and hormone therapy (P=.14) or complications (P=.43) (Table 1).
Table 1.Measures of Central Tendency, Range and P Value of Overall Variables: Age, Type of Mastectomy, Coadjuvant Treatment and Complication.
Patient Satisfaction Quality of Life Total Satisfaction Mean Median Standard Deviation Range P Mean Median Standard Deviation Range P Mean Median Standard Deviation Range P Age (years) <45 76.251 77.145 16.5323 60.43 .503 68.177 66.875 18.4757 80.33 .878 73.754 76.705 15.6937 65.5 .664 45–55 73.969 76.575 15.8471 62.5 68.078 69.835 15.1 75.33 72.07 74.29 14.4304 63.8 >55 77.918 81.14 16.7829 61.33 69.966 73.33 16.4628 61.5 75.322 80.89 15.5222 60.89 Mastectomy type MRM 78.056 81.17 16.5718 63.67 .133 70.647 72 14.0054 52.67 .53 75.706 77.55 14.1424 54.78 .208 MS + SLN 70.989 75.5 16.6707 60 67.228 67.75 17.7228 75.33 69.865 72.84 16.3523 64.57 MS or MSC 73.827 78.88 17.1942 64 66.918 72.085 20.744 72.66 71.392 77.1 16.9569 62.7 Chemotherapy Yes 75.874 79.5 18.1782 64 .262 68.158 70 16.5986 77.33 .54 73.401 77.33 16.3913 66.9 .616 No 73.398 77.43 13.8877 56.19 70.39 70.67 16.2966 66 72.437 75.9 13.5884 59.29 Breast radiotherapy Yes 79.162 80.515 15.807 62.5 .167 67.605 70 16.8823 80.33 .505 75.15 77.325 14.9603 65.3 .608 No 73.618 76.86 17.0536 64 69.354 70.67 16.39 77.33 72.359 75.9 15.6532 66.9 Axillary radiotherapy Yes 81.491 79.86 11.245 36 .174 65.897 69 12.8904 43.42 .348 76.195 77.55 10.0396 33.31 .64 No 74.29 77.43 17.1169 64 69.894 70.67 16.3295 80.33 72.934 76.5 15.771 66.9 Hormone therapy Yes 73.807 76.86 17.0502 62.71 .077 68.357 70.67 16.4811 80.33 .519 72.076 76.2 15.6932 66.9 .142 No 82.19 81.235 14.3206 41.86 71.328 78.33 17.5934 59 78.591 81.405 13.9206 45.58 Complications Yes 78.816 78.83 13.6313 53.71 .359 69.831 71 15.5652 64 .63 75.819 76.2 12.6659 49.8 .433 No 74.473 78.86 17.1438 64 68.126 69 16.8453 77.33 72.502 76.4 15.9067 66.9 MRM: modified radical mastectomy; MS + SLN: mastectomy + sentinel lymph node; MS or MSC: simple mastectomy or subcutaneous mastectomy.
- d.
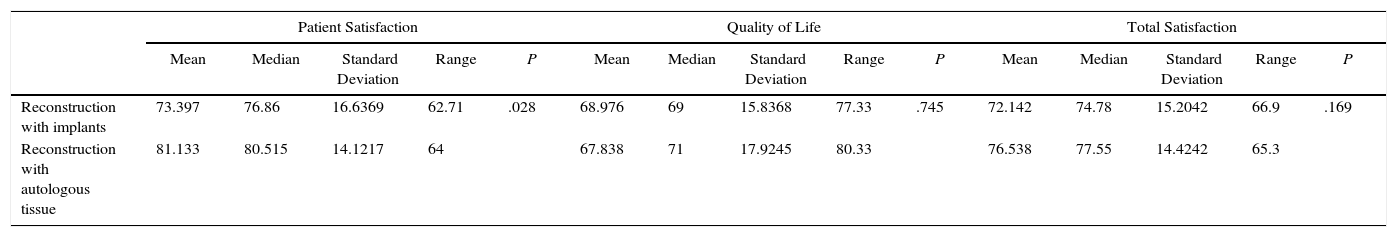
Assessment of satisfaction according to the type of reconstruction performed: when the breast reconstruction types were compared, a tendency was observed towards greater “total satisfaction” and “quality of life” in patients reconstructed with autogenous tissue versus reconstructions with implants (although the difference was not statistically significant: P=.74 and .16, respectively).However, when we compared “patient satisfaction”, there were significant differences, and the patients with autogenous tissue reconstruction were more satisfied than those with implants (P=.028) (Table 2).
Table 2.Measures of Central Tendency, Range and P Value According to the Type of Breast Reconstruction.
Patient Satisfaction Quality of Life Total Satisfaction Mean Median Standard Deviation Range P Mean Median Standard Deviation Range P Mean Median Standard Deviation Range P Reconstruction with implants 73.397 76.86 16.6369 62.71 .028 68.976 69 15.8368 77.33 .745 72.142 74.78 15.2042 66.9 .169 Reconstruction with autologous tissue 81.133 80.515 14.1217 64 67.838 71 17.9245 80.33 76.538 77.55 14.4242 65.3 - e.
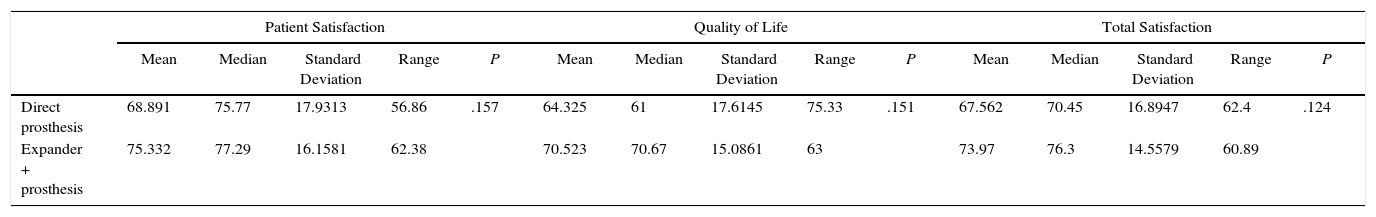
Assessment of satisfaction according to reconstruction type with implants: within the groups reconstructed with implants, 25% (18 patients out of 73) did so with the placement of a direct prosthesis and 75% (55 cases out of 73) with a 2-stage reconstruction: expander and later substitution with prosthesis.When we compared the levels of satisfaction between the two groups, we observed that, although all the levels of satisfaction are superior in the patients reconstructed in 2 stages (expander and prosthesis) versus those who were reconstructed with direct prosthesis; these differences were not statistically significant (“patient satisfaction” P=.15; “quality of life” P=.15 and “total satisfaction” P=.12).
- f.
Assessment of satisfaction according to the reconstruction type with autogenous tissue: out of the cases reconstructed with autogenous tissue, 34% (16 cases) were latissimus dorsi with prosthesis and the remaining 64% were exclusively autogenous tissue, divided in turn into latissimus dorsi without prosthesis (6.7%, 3 cases) and Transverse Rectus Abdominis Muscle flap (TRAM) and free flaps (57.8%-26 cases).After the statistical study, no significant differences were observed between the 3 types of “reconstruction with autogenous tissue” and the levels of satisfaction, including “patient satisfaction” (P=.69), “quality of life” (P=.22), and “total satisfactions” (P=.39) (Table 3).
Table 3.Measures of Central Tendency, Range and P Value According to Type of Reconstruction With Implants.
Patient Satisfaction Quality of Life Total Satisfaction Mean Median Standard Deviation Range P Mean Median Standard Deviation Range P Mean Median Standard Deviation Range P Direct prosthesis 68.891 75.77 17.9313 56.86 .157 64.325 61 17.6145 75.33 .151 67.562 70.45 16.8947 62.4 .124 Expander + prosthesis 75.332 77.29 16.1581 62.38 70.523 70.67 15.0861 63 73.97 76.3 14.5579 60.89
When performing the statistical study, prior to the assessment of satisfaction levels, we observed that several variables correlated with each other. A correlation was observed between the main variable of our study, the “type of reconstruction” performed and other variables such as the “type of mastectomy” (P=.001), treatment with chemotherapy (P=.005), with radiotherapy of the chest (P=.001) and with axillary radiotherapy (P=.0001).
These correlations indicate that the choice of reconstructive surgical technique is often determined by the type of previous mastectomy that has been performed and whether or not patients have received coadjuvant treatment. Thus, a positive correlation was observed between reconstructions with implants and a simple mastectomy and no coadjuvant treatment. Likewise, a positive correlation was found between reconstruction with autogenous tissue and a modified radical mastectomy and the administration of adjuvant treatment, chemotherapy or radiotherapy.
DiscussionSeveral studies7–9 have demonstrated the psychological impact that mastectomy causes in patients who present it. Therefore, if the oncological disease is controlled, breast reconstruction is offered by our service. Most of the reconstructions at our hospital are performed with implants, and 74% were performed with autogenous tissue. This percentage is similar to that observed in the United States in a study similar to ours, with a reconstruction rate with implants of 70% and with autogenous tissue of 30%.3
In our study, when comparing the levels of satisfaction between the 2 major types of reconstruction, implants versus autogenous tissue, we observed that the values of the 3 satisfaction variables (“patient satisfaction”, “quality of life” and “total satisfaction”) are superior in the reconstructed group with autogenous tissue. However, it is true that these differences were only statistically significant for the “patient satisfaction” variable (P=.028).
This could be due to a more natural appearance of the resulting breast, which undergoes the typical changes of the effect of time, similar to other tissues, such as ptosis or volume change due to weight gain or loss. And this similarity of appearance, together with a natural feel of the reconstructed breast that resembles the previous breast, makes the patient accept it as part of her body and feel more satisfied.
Our results coincide with the report by Alderman et al.,10 who observed higher levels of satisfaction in patients reconstructed with abdominal flaps versus implants. Similarly, Tonseth et al.11 obtained higher levels of satisfaction and an improvement in interpersonal relationships as well as a higher score on the visual analogue scale of the aesthetic results in patients reconstructed with Deep Inferior Epigastric Perforator flap (DIEP) versus reconstructions with implants.
Comparable results were obtained by Saulis et al.12 and Yueh et al.,13 who included reconstruction with latissimus dorsi in their comparison. Saulis et al. found no difference in satisfaction between the reconstruction with abdominal autogenous tissue or with latissimus dorsi, results similar to those of our study. However, in his study, Yueh et al. observed greater satisfaction in those reconstructed with abdominal flaps (DIEP and TRAM) than those reconstructed with latissimus dorsi.
In our study, when we compared only the patients reconstructed with implants, greater satisfaction was observed in patients with two-stage reconstructions compared to those who were reconstructed with a direct prosthesis. Although this difference was not statistically significant, this higher level in the 3 satisfaction variables supports two-stage reconstruction in cases of reconstruction with implants. This may be due to the fact that, despite needing 2 surgeries and tissue expansion time, the definitive prosthesis outcome is more natural since the breast groove can be better located and the tissues better adapt to the prosthesis.
The remaining variables, such as age, type of mastectomy performed, coadjuvant treatment, existence of complications and types of autogenous reconstruction, did not present statistically significant differences in terms of satisfaction levels.
In addition, in our study we observed a correlation between different variables, which we recognize as a study limitation. This correlation is positive between reconstruction with autogenous tissue and having undergone a more aggressive mastectomy (modified radical mastectomy) or having received coadjuvant treatment.
We believe that this is due to the fact that most of the time the reconstruction is done with autogenous tissue (which is a more complex surgical technique and requires longer operating room occupancy) for patients who comply with the aforementioned variables (modified radical mastectomy with coadjuvant treatment, mainly radiotherapy of the chest wall over the mammary bed), since it leaves scar tissue that is poor in quality for the placement of an implant.
Therefore, it is possible that these correlations influence actual levels of satisfaction. It is understandable that having undergone more aggressive breast cancer surgery and received coadjuvant treatment, with the associated side effects, could negatively influence the patient's overall perception of her disease and treatment.
Therefore, if we avoided this correlation that a priori can negatively influence patient satisfaction, the levels of satisfaction after reconstruction with autogenous tissue would be higher than those obtained. To do so, we would have to expand the number of cases to be able to make a comparison between the group reconstructed with prosthesis and the group with autogenous tissue, previously eliminating these possible confounding factors.
Hence, we conclude that reconstruction with autogenous tissue should be offered to a greater percentage of patients, regardless of the variables or the longer surgical time, as this procedure provides a higher level of satisfaction than reconstruction with implants.
Finally, within the group reconstructed with implants, given that we have observed greater satisfaction (although not statistically significant) in patients reconstructed with expanders and subsequent replacement by definitive prosthesis compared to those who received a prosthesis directly, we prefer recommending two-stage breast reconstruction.
Authors’ contributionLucía Gómez-Escolar Larrañaga: study design, data collection, article composition.
Julio Delgado Martínez: analysis and interpretation of the results and approval of the final version.
José María Miguelena Bobadilla: study design and critical review.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Larrañaga LG, Martínez JD, Bobadilla JM. Valoración de la satisfacción en pacientes mastectomizadas con reconstrucción mamaria según la técnica quirúrgica empleada. Cir Esp. 2017;95:594–600.