Traditionally, anterior accessory great saphenous vein insufficiency was managed by crossectomy and resection of varicose veins. The aim of this paper is to show the safety and efficacy of a new therapeutic strategy for anterior accessory great saphenous varicose veins.
MethodsThis non-randomised prospective study included 65 patients with varicose veins from the anterior accessory great saphenous vein. The novelty of the technique is to avoid the great saphenous vein crossectomy and perform just flebectomy of the visible veins. Venous duplex studies were performed preoperatively, a month and a year postoperatively. The clinical assessment was done by the Fligelstone scale.
ResultsThe baseline CEAP clinical classification was: 58% C2, 26% C3 and 15% C4–6. The new strategy was applied to all cases. Complications: 3 haematomas, 7 cases of asymptomatic partial anterior saphenous thrombosis. Reduction of the initial average diameter was from 6.4mm anterior saphenous to 3.4mm by one year (P<.001). At twelve months a forward flow is maintained in 82% of cases. Recurrence of varicose veins was 8%. All patients improved their clinical status based on the Fligelstone scale. Cases with saphenous diameter bigger than 7.5mm and obesity were identified as predictors of worse clinical and haemodynamic outcome.
ConclusionsThis modified surgical strategy for anterior saphenous varicose veins results in better clinical outcomes at one year postoperatively.
Tradicionalmente la insuficiencia de safena anterior se trataba mediante crosectomía y resección de los paquetes varicosos. El objetivo del trabajo es mostrar la seguridad y eficacia de una nueva estrategia terapéutica en las varices dependientes de la vena safena magna accesoria anterior.
MétodosEstudio prospectivo no ramdomizado que incluyó 65 pacientes con varices dependientes de la safena anterior con safena interna anterógrada. La modificación en la técnica consiste en hacer solamente flebectomía de los paquetes varicosos, sin ligar el cayado de la safena. Se realizó un estudio hemodinámico venoso preoperatorio, al mes y al año, y para la valoración clínica se utilizó la escala de Fligelstone.
ResultadosClasificación clínica basal CEAP: C2 58%, C3 26% y C4–6 15%. Complicaciones: 3 hematomas, 7 casos de trombosis parciales asintomáticas de safena anterior. Se observó una reducción del diámetro medio inicial de safena anterior de 6,4mm a 3,4mm al año (p<0,001). A los doce meses mantenían un flujo anterógrado el 82% de los casos. Hubo una recidiva de varices visibles en el 8% de los casos. Todos los pacientes han reflejado una mejoría clínica en la escala de Fligelstone. El diámetro de safena anterior mayor de 7,5mm y la obesidad se identifican como predictores de un peor resultado clínico y hemodinámico.
ConclusionesLa modificación de la estrategia quirúrgica sobre las varices dependientes de la safena anterior presenta un resultado clínico favourable al año de la intervención.
Chronic venous insufficiency (CVI) is a disease with a very high prevalence that requires surgical treatment in most cases. It is one of the most frequently performed scheduled surgeries in Spanish hospitals and has one of the largest waiting lists as well as very elevated healthcare costs.1,2
A review of the activity registry of the Spanish Society of Angiology and Vascular Surgery and an analysis of the last five years show how the surgical treatment of varicose veins surpasses 25,000 procedures annually, with a waiting list of some 14,000 patients.3–7
Surgical treatment for CVI has two modalities: ablation or destruction therapies (classic saphenectomy, endovenous laser ablation, radiofrequency, venous sclerosis, etc.), and haemodynamic treatments that preserve the saphenous veins like ambulatory conservative haemodynamic correction of venous insufficiency (CHIVA).
The CHIVA strategy has been developed over the past twenty years and is currently the second most frequent surgical method (after saphenectomy) for the surgical treatment of CVI.8 This treatment is a therapy designed for the needs of each patient according to the haemodynamic condition responsible for the venous insufficiency, while also preserving the saphenous axis. Most other similar publications and studies about this subject have been concerned with the great saphenous vein. Cases about the anterior accessory saphenous vein have been included amongst them, and the documentation about the anterior saphenous vein itself is limited.
The aim of this study is to evaluate the safety and efficacy of a modification of the standard CHIVA procedure in patients that present varicose veins related with the anterior accessory saphenous vein, without involving the great saphenous vein or the saphenofemoral junction.
MethodsThis prospective study commenced in January 2010 with the inclusion of the first patients who presented with varicose veins of the anterior accessory saphenous vein.
Selected PatientsIdentification of the anterior saphenous vein was done in accordance with the recommendations and consensus guidelines for ultrasound examination and the denomination of the superficial venous system that the International Union of Phlebology published in 2006. According to this consensus, the anterior accessory saphenous vein (AASV) is an ascending venous segment parallel to the great saphenous vein (GSV) in the thigh that is found within its own fascial compartment. There are two ultrasound signs (the “eye sign” and the “alignment sign”) that allow for its identification and differentiation from the GSV.9
The ultrasound examination was done with a linear multi-frequency transducer (Esaote Technos, Genoa, Italy) with the patient standing, at which time the saphenofemoral junction, saphenopopliteal junction, deep venous system, saphenous veins and related varicose veins were observed. The Doppler examination allowed us to assess the permeability and competence of the vessels examined, as well as the presence of reflux and the distribution in venovenous shunts. Reflux was defined as a flow that was inverse to the physiological flow for more than 0.5s. We took measurements of the length and diameter of the AASV at its midpoint and of the diameter of the GSV 15cm from its origin. We completed the study with a Reflux Elimination Test (RET) of the AASV, described by Zamboni.10 The venovenous shunts described for the GSV by the European CHIVA Society at the conference in Teupitz in 2002 were adapted to the AASV region.11
The inclusion criteria used were as follows:
- -
Patients with CVI of the AASV with positive RET and anterograde GSV.
- -
Acceptance of surgery and signed informed consent form.
The exclusion criteria were:
- -
Patients with CVI of the AASV and GSV.
- -
Patients with deep venous insufficiency.
- -
Negative RET test in the AASV.
- -
Patients with limitations to walk normally.
- -
Patients who refused to give their informed consent.
- -
Patients with a saphenous diameter>8.5mm.
A registry of epidemiological data was created, including: sex, age, pregnancies, body mass index, and CEAP classification.
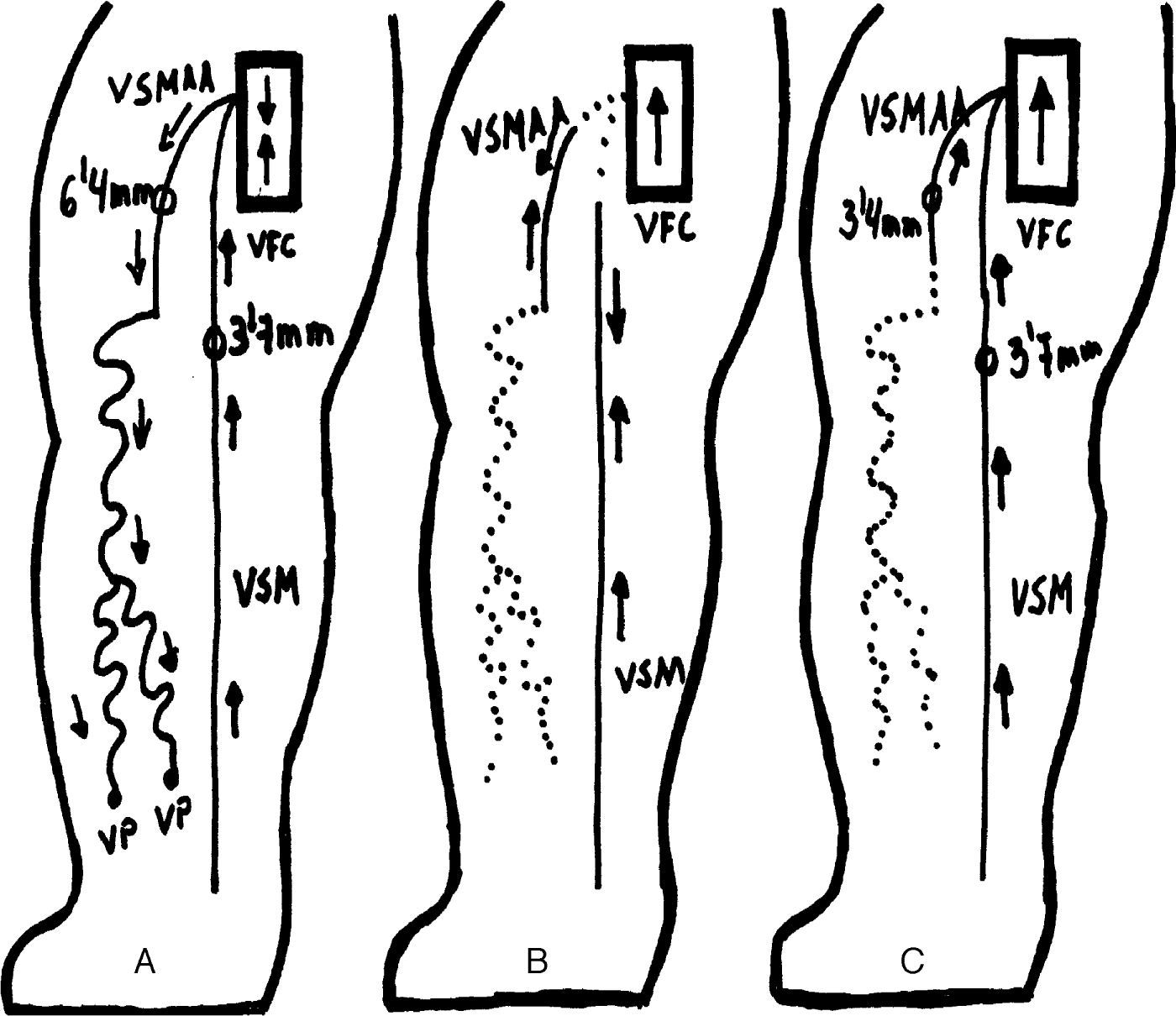
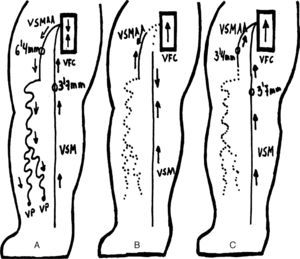
Surgical ProcedureThe modification of the CHIVA strategy consisted of disconnection and removal of the tertiary network from the AASV, interrupting the venovenous shunt and forcing anterograde flow through the AASV itself, without operating on the main leak point located at the saphenofemoral junction (Fig. 1). The surgery was conducted as part of the major outpatient surgery programme at our hospital. A strategic incision was made to disconnect the varicose vein network of the AASV and afterwards multiple complementary incisions were made to eliminate the varices. Local anaesthesia was used, with postoperative wrapping and low molecular weight heparin at prophylactic doses (bemiparin 2500–3500units/day) for 10 days, following known criteria.8
Patient mapping with varicose tributaries of the saphenous vein: (A) baseline situation of AASV-related varicose veins; (B) CHIVA cure 1+2 (traditional), non-haemodynamic approach: crossectomy of the saphenofemoral junction and disconnection of the varicose veins from the AASV and extensive phlebectomy; (C) haemodynamic CHIVA cure (innovative procedure): disconnection of the varices from the AASV and extensive phlebectomy.
The duration of surgery was variable and basically depended on the phlebectomy done, although it was always less than 90min.
Follow-upThe first follow-up visit was one month later, and patients were checked for the presence of clinical and haemodynamic complications (deep vein thromboses or saphenous thromboses) as well as the presence of reflux in the AASV. After one year, ultrasound studies were conducted in the same manner.
Treatment was considered haemodynamically successful when there was a reduction in the diameter of the AASV, which became anterograde and lost reflux. Treatment was considered a haemodynamic failure when the AASV presented reflux, the GSV had increased in size or presented reflux, or there was thrombosis of the femoral vein.
Twelve months later, the efficacy of the procedure was determined with the assessment of the clinical results by means of the Fligelstone scale and the absence of recurrences.12 Patient satisfaction was assessed using a numeric scale from 1 to 10.
Study Variables and Statistical AnalysisThe predictive variables that were contemplated included age, sex, excess weight (BMI>25), reoperation of varices, length of AASV (longer or shorter than 10cm), diameter of the GSV (75th percentile greater than 7.5mm) and type of haemodynamic shunt (type 3 or type 5). We have considered variables resulting from haemodynamic success or failure (anterograde flow or reflux), saphenous vein thrombosis and the presence of varicose recurrence, all one year later.
The data were processed statistically with SPSS v21 software. To determine whether there was a relationship between certain variables and the presence of recurrence, saphenous vein thrombosis and haemodynamic failure, the corresponding analyses were completed. For qualitative variables, Fisher's exact test or the chi-squared test were used. For quantitative variables, prior to the analysis normality was checked with the Shapiro–Wilk test. For the variables that followed a normal distribution, Student's test was applied; when this was not verified, the non-parametric Mann–Whitney U test was applied. The multivariate analysis was conducted by means of nominal logistic regression.
ResultsDemographic DataThe 12-month follow-up was completed by 65 patients, who were predominantly female: 58 women and 7 men. Mean age was 46. A previous internal saphenectomy had been done in 6 (9%) patients. The female subjects had an average of 2 prior pregnancies. Twenty-six (40%) patients were overweight. CEAP distribution was class II in 27 (41%) cases, class III in 20 (31%) and classes IV, V or VI in 18 (28%) cases, with four open ulcers.
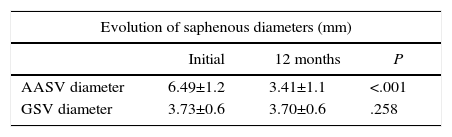
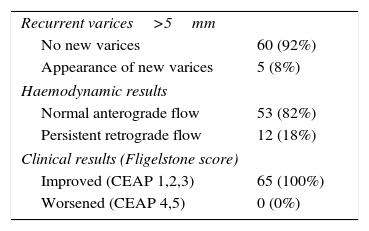
Haemodynamic ResultsData were collected for ultrasound and haemodynamic parameters. The most frequent type of venovenous shunt described in the AASV was type III (50, 77%) followed by type V (14, 22%) and only one case of IIa (1%). The new CHIVA strategy applied in all the cases was haemodynamic. The AASV was less than 10cm in 33 cases (51%), and greater than 10cm in the 32 (49%) remaining cases. The mean starting diameter of the AASV was 6.4mm; after 12 months, this had been reduced to 3.4mm, with a mean reduction of 3mm. The GSV diameter was not modified (Table 1). A favourable haemodynamic result was observed in 53 (82%) patients, while reflux persisted in the AASV in 12 (18%) cases (Fig. 2).
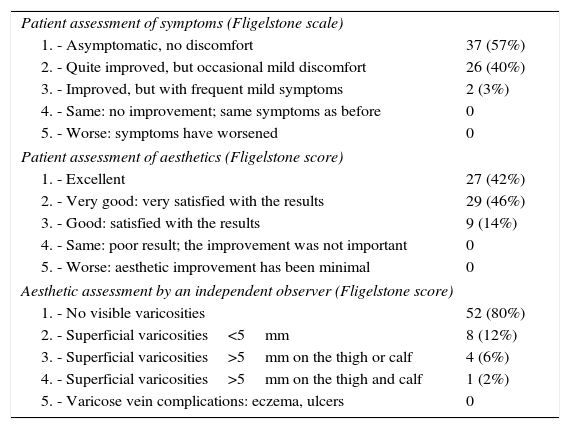
The application of the Fligelstone scale showed clinical and aesthetic improvement in all patients (Tables 2 and 3). A search for clinical recurrence revealed 5 (8%) cases of recurrent varices larger than 5mm.
Symptomatic and Aesthetic Assessment 12 Months After Surgery of the 65 Patients in Follow-up.
| Patient assessment of symptoms (Fligelstone scale) | |
| 1. - Asymptomatic, no discomfort | 37 (57%) |
| 2. - Quite improved, but occasional mild discomfort | 26 (40%) |
| 3. - Improved, but with frequent mild symptoms | 2 (3%) |
| 4. - Same: no improvement; same symptoms as before | 0 |
| 5. - Worse: symptoms have worsened | 0 |
| Patient assessment of aesthetics (Fligelstone score) | |
| 1. - Excellent | 27 (42%) |
| 2. - Very good: very satisfied with the results | 29 (46%) |
| 3. - Good: satisfied with the results | 9 (14%) |
| 4. - Same: poor result; the improvement was not important | 0 |
| 5. - Worse: aesthetic improvement has been minimal | 0 |
| Aesthetic assessment by an independent observer (Fligelstone score) | |
| 1. - No visible varicosities | 52 (80%) |
| 2. - Superficial varicosities<5mm | 8 (12%) |
| 3. - Superficial varicosities>5mm on the thigh or calf | 4 (6%) |
| 4. - Superficial varicosities>5mm on the thigh and calf | 1 (2%) |
| 5. - Varicose vein complications: eczema, ulcers | 0 |
Clinical Results After 12 Months.
| Recurrent varices>5mm | |
| No new varices | 60 (92%) |
| Appearance of new varices | 5 (8%) |
| Haemodynamic results | |
| Normal anterograde flow | 53 (82%) |
| Persistent retrograde flow | 12 (18%) |
| Clinical results (Fligelstone score) | |
| Improved (CEAP 1,2,3) | 65 (100%) |
| Worsened (CEAP 4,5) | 0 (0%) |
Overall patient assessment of the treatment defined by the numerical scale showed that none of the patients gave our performance poor marks. Their evaluations were predominantly positive, with an excellent average score of 9.4.
ComplicationsThree (5%) haematomas were detected, none of which required surgical treatment. There were no deaths, hospitalisations, deep venous or symptomatic superficial thromboses, infections or episodes of neuritis. Early ultrasound tests detected 7 (11%) partial thromboses of the AASV, although no patients reported spontaneous symptoms requiring emergency room attention.
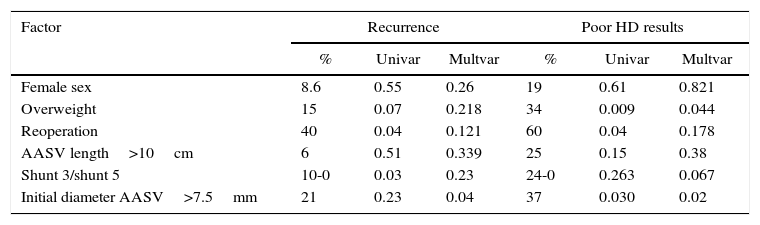
Analysis of the ResultsThe statistical analysis used to determine whether there was a correlation between the variables and the presence of clinical recurrence, saphenous thrombosis and the haemodynamic results showed no statistically significant association with sex, prior intervention, length of the AASV or shunt type. In contrast, the initial diameter of the AASV>7.5mm and excess weight were statistically significant as factors associated with a poor haemodynamic result, without showing significance for clinical recurrence (Table 4).
Analysis of Factors Related With the Results of Recurrence and Poor Haemodynamic Results After 12 Months.
| Factor | Recurrence | Poor HD results | ||||
|---|---|---|---|---|---|---|
| % | Univar | Multvar | % | Univar | Multvar | |
| Female sex | 8.6 | 0.55 | 0.26 | 19 | 0.61 | 0.821 |
| Overweight | 15 | 0.07 | 0.218 | 34 | 0.009 | 0.044 |
| Reoperation | 40 | 0.04 | 0.121 | 60 | 0.04 | 0.178 |
| AASV length>10cm | 6 | 0.51 | 0.339 | 25 | 0.15 | 0.38 |
| Shunt 3/shunt 5 | 10-0 | 0.03 | 0.23 | 24-0 | 0.263 | 0.067 |
| Initial diameter AASV>7.5mm | 21 | 0.23 | 0.04 | 37 | 0.030 | 0.02 |
This table shows the different factors that have been studied with regards to recurrence variables after 12 months and poor haemodynamic results (according to the criteria established in Table 3). The percentages represent the presence of each factor. The univariate analysis was done with the chi squared or Fisher text, and the P reached for each test is shown. For the multivariate analysis, a nominal logistic regression model was followed, and P values are also included.
AASV: anterior accessory saphenous vein.
HD: haemodynamic.
The AASV is responsible for 11% of the varices of the extremities, 10%–43% of recurrent varicose veins and poorer results after treatment, according to some authors.13–17
The classic treatment for varicose veins originating in the groin with distribution in the region of the anterior saphenous vein involves standard crossectomy of the saphenofemoral junction, with ligature and disconnection of all the tributaries, including the AASV and GSV, as well as internal saphenectomy, to reduce the number of recurrences. In the last decade, several authors have treated the AASV exclusively, without removing or operating on the healthy GSV. In a study from 2001, Prinz recommended that, in cases of AASV-related varices with a competent GSV, standard crossectomy should be done of the saphenofemoral junction with removal of the initial cm of the AASV as well as the GSV, plus complementary phlebectomy, while leaving intact the rest of the GSV.18 In 2011, Theivacumar used a treatment with endovenous laser in patients with AASV varicose veins with a minimal length of 10cm and a diameter of 3mm, without affecting the GSV, with good results.19
Careful haemodynamic mapping of the AASV varices allowed us to design this treatment in which we disconnect the venovenous shunt and eliminate the varicose network, without the need to operate in the groin with closure of the saphenofemoral junction, thus respecting the GSV. Crossectomy is avoided and the GSV is preserved for future material in case revascularisation bypass were ever needed.
In our series, the GSV was not modified by our actions and was maintained anterograde in all cases. Meanwhile, the AASV remained with anterograde flow in 82% of the cases. Currently, there are no studies about haemodynamic surgery that have described this type of treatment in AASV-related varices.
In our approach, we have assumed the treatment proposed for the GSV by Zamboni more than a decade ago, which support performing haemodynamic surgery in patients with a positive RET test in the GSV after the interruption of the venovenous shunt by compression of the R3. In the first series from 2001, the patients who were treated in this manner presented a GSV with anterograde flow in 85% of cases after 6 months. The second series presented a three-year follow-up with anterograde saphenous vein flow of 18% in the cases that presented incompetence of the ostial valve and 86% in those with competent ostial valves. In 2003, Escribano presented six-month results for anterograde flow of only 12%.10,20,21
Saphenous vein thrombosis was one of the complications that we feared. We used low-molecular-weight heparin for one month to minimise this risk. One month later, 7 partial AASV thromboses were detected, although they were asymptomatic and did not persist after one year. The clinical complications presented were local haematomas, which resolved spontaneously with no problems. These results coincide with the study about CHIVA surgery complications published by our group some years ago, and they provide evidence about the safety of this therapeutic modality.8
The clinical results have been favourable in all cases, including patients that have presented recurrence, with very high patient satisfaction. We have not found statistically significant associations between most variables and the presence of recurrence, saphenous vein thrombosis or haemodynamic failure. We have found, however, that excess weight and AASV diameter>7.5mm are associated with poorer haemodynamic results. In these cases and in the future, we would consider other therapeutic options.
The limitations of our study include the small number of cases and a follow-up period that is still short. It is useful to observe that the potential thrombosis of the AASV with extension to the saphenofemoral junction and the common femoral vein, which could be associated with this treatment variation for AASV-related varicose veins, did not occur. Nor did we observe a high number of recurrences. Furthermore, the percentage of complications was low and patient satisfaction high.
It is possible that this technique is not the technique of choice for patients with an anterior saphenous vein larger than 7.5mm or in very obese patients.
This new haemodynamic treatment method for AASV varicose veins presents successful haemodynamic and clinical results 12 months later, with high patient satisfaction. It is safe, and complications are local and benign. It enables us to correct AASV-related varices without having to operate on the saphenofemoral junction or the GSV, which continues to function correctly and is potentially useable for revascularisation surgery.
FundingNo institutional funding was received for the elaboration of this study.
Authorship/CollaboratorsNMF: design, data collection, analysis, writing, critical review and approval.
JPLP: design, analysis, writing, critical review and approval.
CLE: analysis, writing, critical review and approval.
FJMG: design, data collection and approval.
ERD: writing critical review and approval.
Conflict of InterestsThe authors declare having no conflict of interests.
The content of this article is original and has not been submitted for consideration at any other publication, either in its entirety or partially. Preliminary results of this study were presented at the 30th Conference of the Andalusian Society of Angiology and Vascular Surgery in 2013 and included in the supplement of the scientific journal Actualidad Médica that was published in relation to the conference: Actual Med 2013; 98: (789). Supl. 13–16.
Please cite this article as: Maldonado-Fernández N, Linares-Palomino JP, López-Espada C, Martínez-Gámez FJ, Ros-Díe E. Resultados clínicos de una nueva estrategia quirúrgica (CHIVA modificado) en el tratamiento de las varices dependientes de la vena safena magna accesoria anterior. Cir Esp. 2016;94:144–150.