Chronic intestinal ischemia is a very rare condition, generally caused by occlusive atherosclerotic disease (95%). The main symptom is postprandial abdominal pain, and diagnosis is based on symptoms and angiographic examinations of arterial lesions. Massive intestinal infarction is the most important complication.
The patient is a 69-year-old male with a medical history that included active chronic smoking, left iliofemoral+left-right femoral-femoral bypass due to atherosclerosis in 1996, TURP for BPH and TURED because of a neoplasm one month earlier. The patient was hospitalized in order to study a poorly defined abdominal pain in the left iliac fossa that had made him come to the emergency department on several occasions over the course of the previous 2 months. The patient reported no alteration in bowel habit, although the family stated that he had lost an important amount of weight.
We ordered several tests in order to rule out any possible neoplastic processes. Abdominal CT demonstrated a nodule in liver segment III. The abdominal ultrasound results recommended extending the study with MRI. Given the non-specific mass, FNA was suggested, which was negative for malignant cells. At the same time, chest radiography showed nodules in the right lung; thoracic CT was ordered, which was normal.
It should be mentioned that, while hospitalized, the patient did not comply with the nil per os treatment and committed dietary transgressions without either the knowledge or consent of the medical personnel. As a result, it was very difficult for us to establish the diet/onset of pain correlation, which was triggered 15–60min after oral intake.
For this reason, we suspected possible intestinal ischemia. Abdominal aortoiliac CT angiography detected severe stenosis in the proximal end of the celiac trunk, complete obstruction of the proximal segment of the superior mesenteric artery and 70%–80% stenosis of the inferior mesenteric artery, which drained through the arc of Riolan. Colonoscopy showed the mucosa did not have an ischemic appearance, with isolated diverticula.
We arrived at the diagnosis of chronic intestinal ischemia affecting the 3 blood vessels.
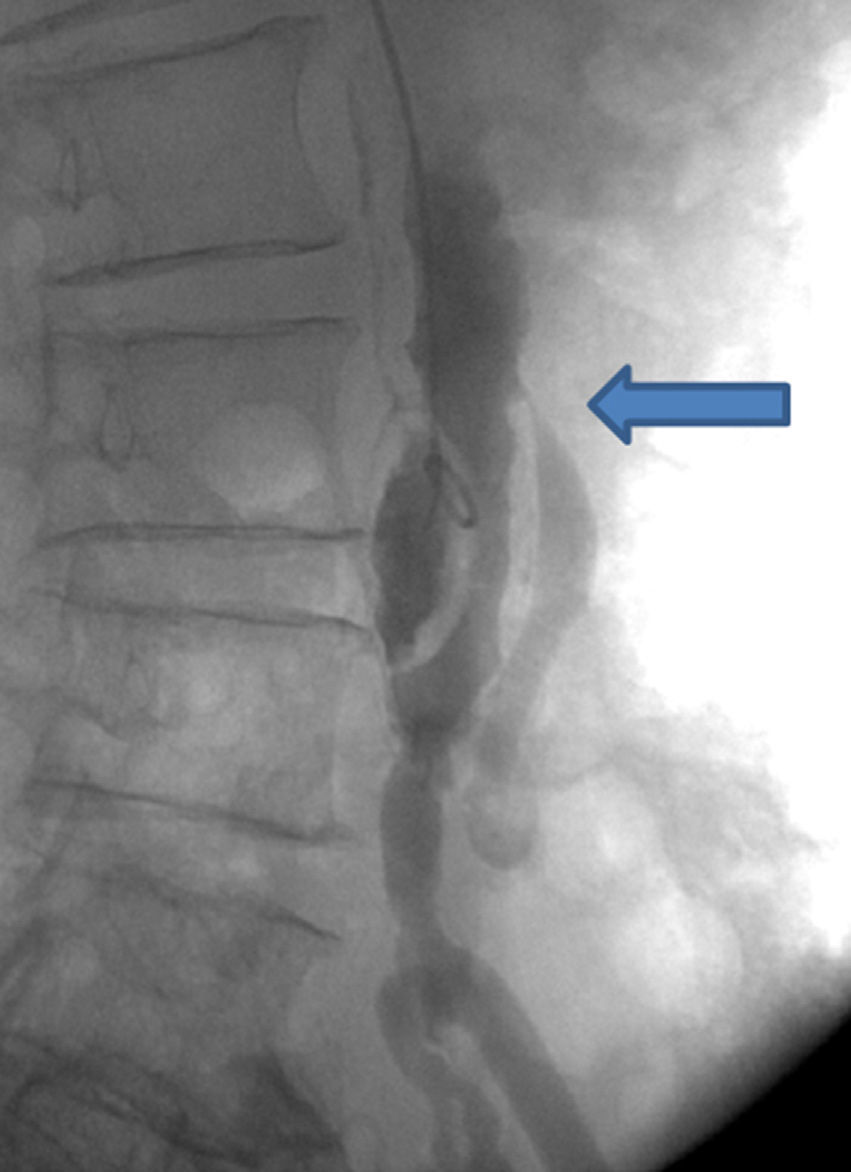
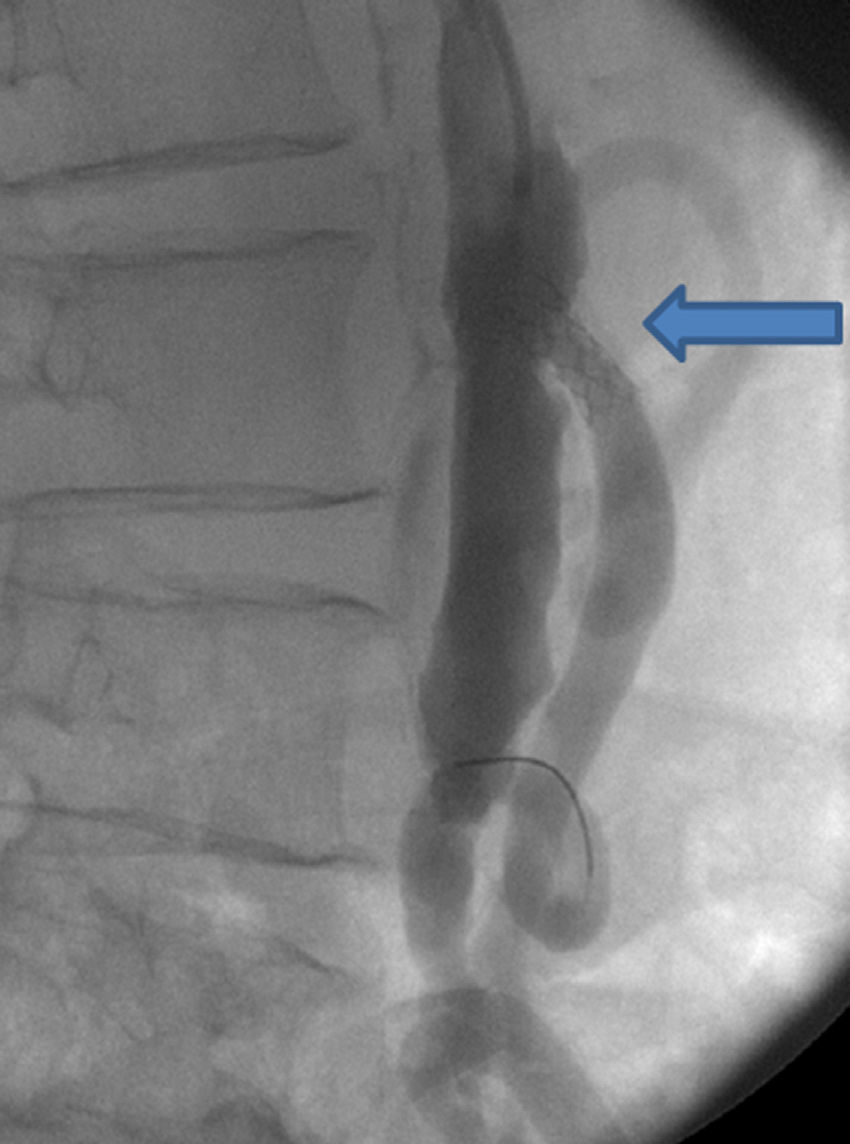
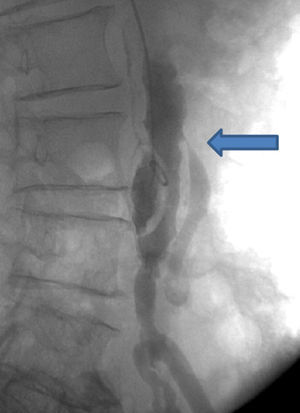
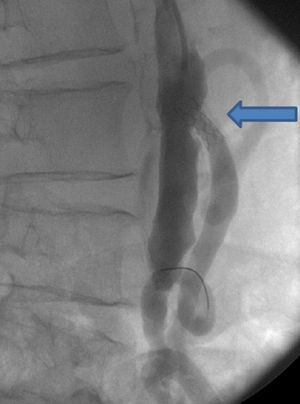
In a multidisciplinary session with vascular surgery, radiology and general surgery specialists, and while considering the patient's high surgical risk, it was decided that we should perform angiography and attempt to place stents in the 3 affected blood vessels. However, only one stent was successfully inserted (7mm×18mm expandable balloon) in the inferior mesenteric artery, after which good permeabilization was achieved with quite an improvement in the patient's usual symptoms (Figs. 1 and 2). In case of failure, we had considered an inferior aortomesenteric bypass as it had a good caliber posterior to the stenosis and a good arc of Riolan, although this would have entailed very high surgical risk.
The patient reinitiated oral intake with no new episodes of abdominal pain. He was discharged with treatment including clopidogrel and pantoprazole. One year later, he has not returned to the emergency department, and periodic outpatient follow-up visits in the outpatient consultation have been satisfactory.
Chronic intestinal ischemia is an uncommon condition, given the large quantity of collateral arteries and variant vessels that supply blood to the intestine. It is associated with high morbidity and mortality as its main complication is massive intestinal infarction. Its main etiology is occlusive atherosclerotic disease (95%), especially in the ostia of the 3 main trunks that supply the intestines: celiac trunk, superior mesenteric artery and inferior mesenteric artery.
The most common symptom is postprandial abdominal pain that appears 10–30minutes after oral intake and lasts 1–3h. As the pain progressively increases, the patient eats less and loses weight as a result.1–4 The diagnosis is based on symptoms and the angiographic examinations of the arterial lesions. The differential diagnosis includes gastroesophageal reflux disease, irritable bowel syndrome, peptic ulcer or gastritis, chronic pancreatitis, visceral cancer and vasculitis, such as polyarteritis nodosa.
In chronic intestinal ischemia, angiography, which can be therapeutic, is still the exploration of choice. It should be mentioned, however, that in many instances the diagnostic suspicion arises from abdominal CT, CT angiography or MRA.
Traditionally, the treatment of this disease has been surgical revascularization of the visceral arteries. Endarterectomy and artery implants have also been used. Each of these treatments has important morbidity and mortality associated with advanced age, cardiovascular state and, to a lesser degree, failed revascularization.2,5,6 It is still the treatment of choice for patients who are fit or whose physical condition can be improved before surgery.
In the 1980s, this disease started to be treated with balloon angioplasty and stents, a minimally invasive percutaneous technique with lower morbidity and mortality rates than traditional surgery. When the literature is reviewed, the results obtained give mean success rates above 90% and good immediate clinical results in 85%. There has been greater success obtained in non-ostial than in ostial lesions. Stent implantation should always be considered the first option after successful angioplasty.2,3,6–9 The technique is performed with local anesthesia and the patient can be discharged 24h later, which reduces hospitalization times and increases patient comfort.2,10 Nevertheless, even though the results are initially good, there is a greater percentage of restenosis and higher symptoms recurrence than in revascularization surgery.
When treating such cases, it is very important to understand the natural history of the disease while taking into account patient age, comorbidities and surgical risk. The decision-making process should be multidisciplinary and aimed at finding the best possible therapeutic option.3,10
Please cite this article as: Palau Figueroa T, Roura Agell M, González Martínez V, Medarde Ferrer M, De Caralt Mestres E. Isquemia intestinal crónica por estenosis severa múltiple resuelta mediante cirugía endovascular en paciente de alto riesgo. Cir Esp. 2015;93:48–50.