Choledochal cysts are rare bile duct dilatations, which have higher prevalence in Asian population.
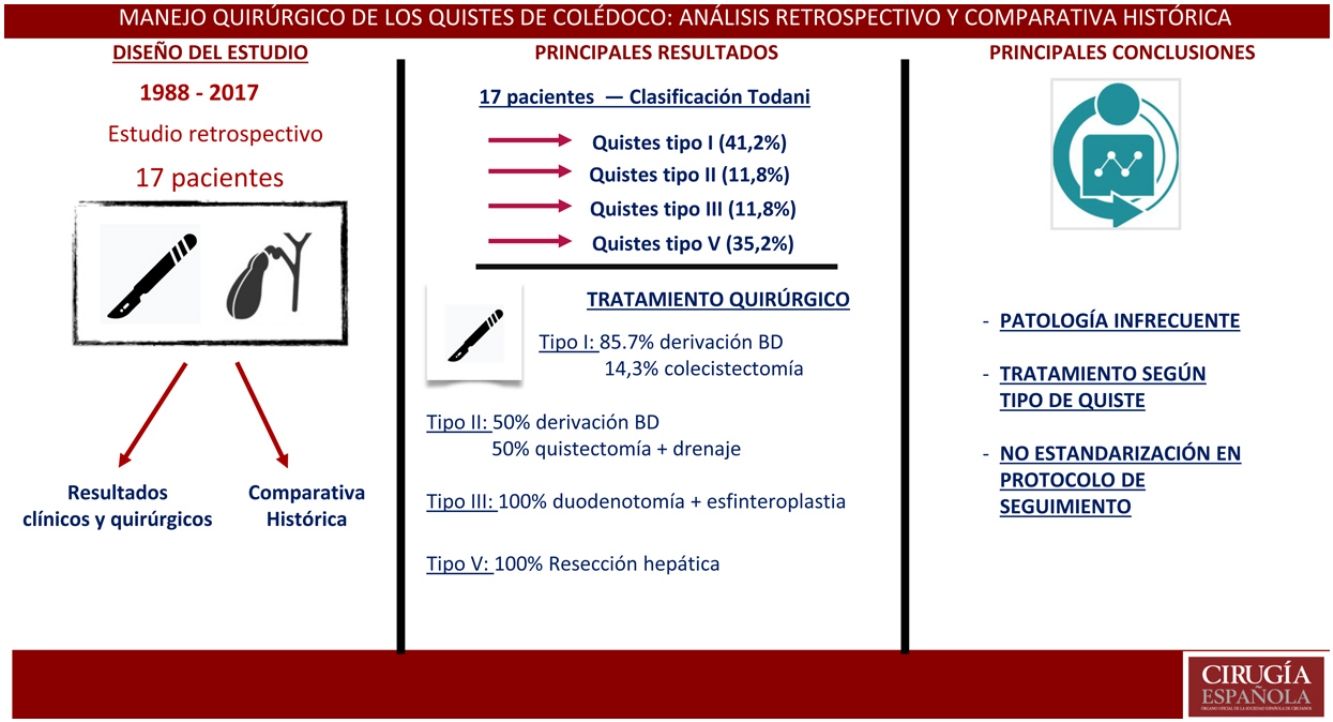
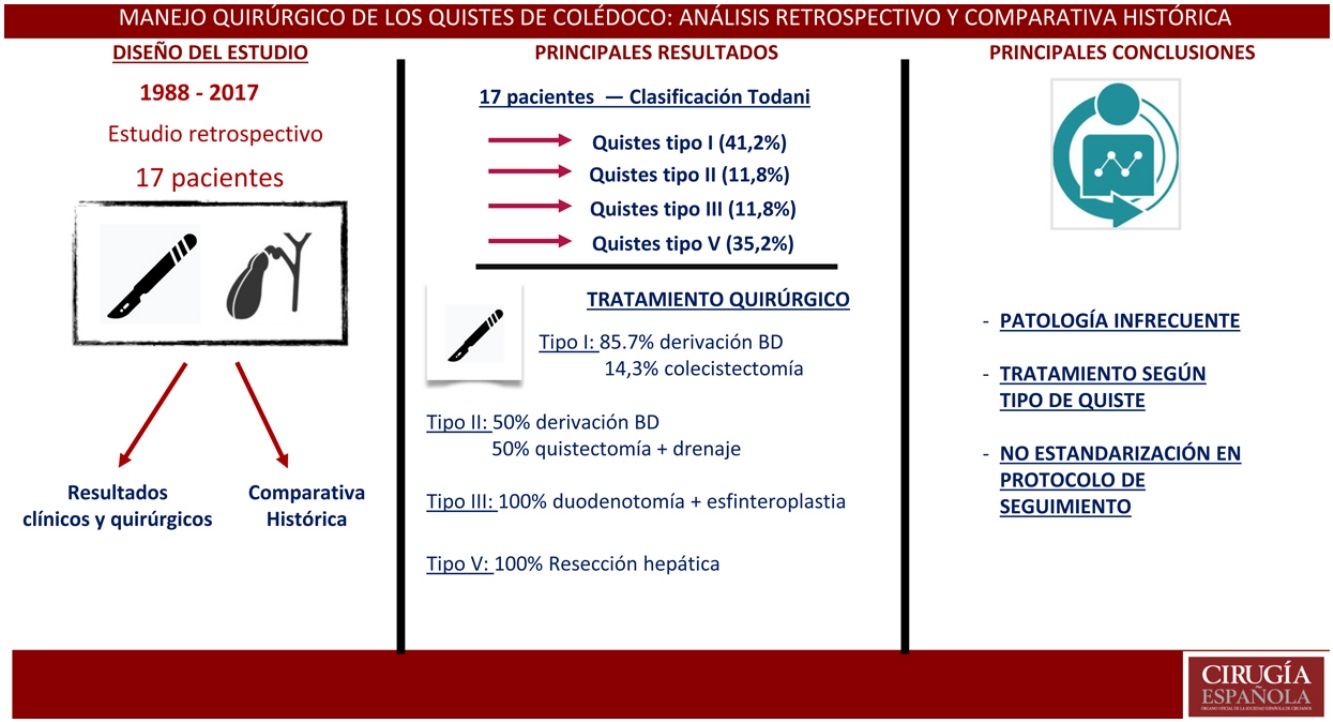
The aim of the study was to analyze clinical and surgical results about biliary cysts management. In addition, a comparative historical analysis was performed.
MethodsPatients who underwent surgery between January 1988 and December 2019 in a single tertiary level center were retrospectively included. Demographic and clinical patient data; cyst types; diagnostic methods and surgical technique were analyzed, as well as short and long-term follow-up complications. A comparative descriptive study focus on the main historical series was also carried out.
ResultsA total of seventeen patients were identified; 58.8% were men. The mean age at diagnosis was 39.9 years (SD: 20.54). The median follow-up was 5 years (IQR 1-15). The most frequent cysts were type I (41.2%). Abdominal pain was the most common presenting symptom (58.8%).
Cystic excision with bilio-enteric anastomosis was the main procedure, it was underwent in 85, 7% type I cysts. 29.4% postoperative complications were recorded. Malignancy was not documented in any pathology specimen.
ConclusionsCholedochal cysts are an uncommon disorder whose diagnosis requires a high level of suspicion. Surgical treatment depends on type of cyst. In most patients with choledochal cysts disease, complete cyst excision with bilio-enteric anastomotic reconstruction is the treatment of choice.
Los quistes de colédoco son una rara entidad en la que se forman dilataciones quísticas del árbol biliar, con mayor prevalencia en poblaciones asiáticas.
El objetivo principal del estudio fue el análisis de los resultados clínicos y quirúrgicos en el manejo de los quistes biliares. De forma secundaria, se realizó un análisis comparativo de las principales series históricas publicadas.
MétodosEstudio observacional retrospectivo en un único centro de tercer nivel. Se incluyeron pacientes intervenidos quirúrgicamente entre enero de 1988 y diciembre de 2019. Los datos demográficos, clínicos y analíticos de los pacientes, tipos de quiste, métodos diagnósticos, técnica quirúrgica empleada, así como los resultados del seguimiento y complicaciones a corto y largo plazo fueron analizados. Se realizó un estudio descriptivo comparativo con las principales series históricas.
ResultadosSe identificaron 17 pacientes con edad media de 39,9 años (DE: 20,54); el 58,8% eran varones. La mediana de seguimiento fue de 5 años ( 1-15). Los quistes tipo I fueron los más frecuentes (41,2%); la manifestación clínica más frecuente fue el dolor abdominal (58,8%).
La escisión quística con derivación biliodigestiva fue el principal procedimiento realizado en quistes tipo I (85,7%). Un 29,4% presentó complicaciones posquirúrgicas. No hubo hallazgos de malignidad en el estudio anatomopatológico.
ConclusionesLos quistes de colédocos constituyen una patología de baja incidencia que requiere un alto nivel de sospecha para su diagnóstico. El tratamiento quirúrgico se ajusta al tipo de quiste, siendo la escisión del quiste y la derivación biliodigestiva el tratamiento quirúrgico más comúnmente empleado.
Choledochal cysts are a rare entity that involve cystic dilatations of the intra- or extrahepatic biliary tree. Most reported cases have been published in Asian countries, with an incidence of 1:1000, compared to 1:100 000 - 150 000 in Western populations. These cysts are more common in women, with a female:male ratio of 3:1 to 4:11–5. Classically, choledochal cysts were diagnosed in childhood, although more recent studies establish a similar incidence in adulthood6.
Cysts can be congenital or acquired (secondary to bile duct surgery)7 and have been associated with a wide variety of congenital anatomical abnormalities. Several theories have been proposed on the formation of bile cysts. The theory proposed by Babbitt8,9 in 1969 is that the main factor is an anomalous pancreaticobiliary junction (APBJ), resulting in pancreatic reflux towards the biliary tree. Cha et al3 and Singham et al4 have questioned this theory because APBJ is a rare congenital anomaly, with a registered prevalence of 0.03% in the Japanese population and present in 50%-80% of patients with bile cysts. Kusunoki et al10 proposed the reduction of ganglion cells in the cyst wall, which would correspond with biliary oligoganglionosis, similar to what is found in Hirschsprung’s disease of the colon as the origin of cyst formation.
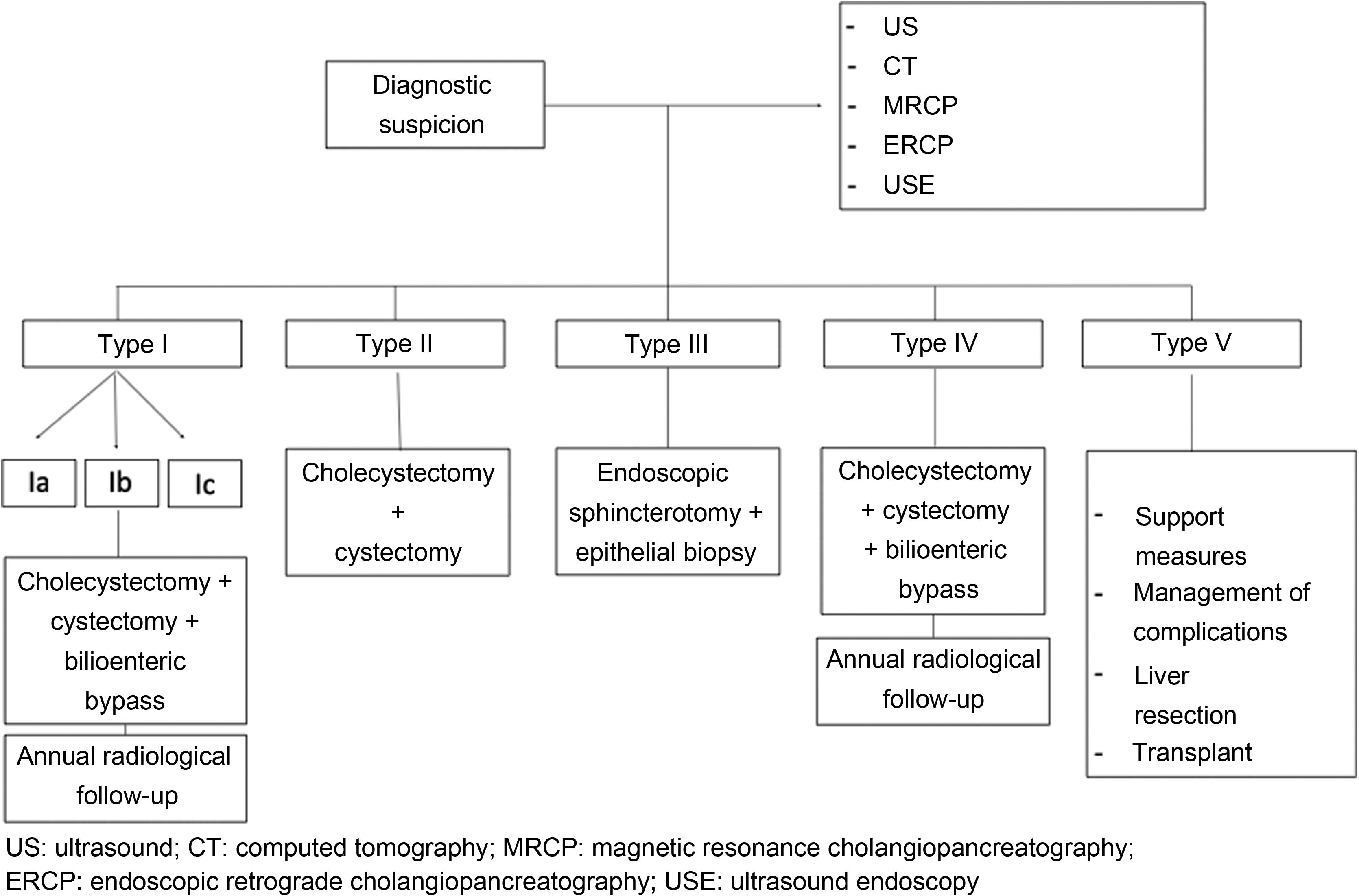
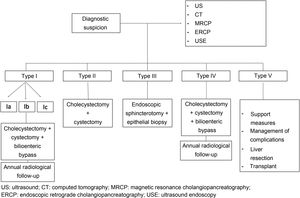
The most widely used classification scheme today is Todani’s, which was refined in 2003 to incorporate the presence of APBJ2. This classification identifies 5 main types: type I, the most common (50%-80%), is described as a dilatation of the extrahepatic bile duct type that can be cystic (Ia), focal or segmental (Ib) or fusiform (Ic); type II is supraduodenal extrahepatic diverticulum; type III involves an intraduodenal cyst, also called choledochocele; type IV (15%-35%) includes both extrahepatic and intrahepatic cysts; and type V is comprised of multiple intrahepatic cysts (Caroli’s disease).
The main objective of this study is to review and compare clinical and surgical results in the management of biliary cysts. For a complete analysis, we present the clinical, diagnostic and surgical data from a national tertiary center and establish a comparison with the most extensive historical series published.
MethodsDesignThis is a retrospective observational study of data from a prospective database, carried out at a single tertiary hospital. A descriptive comparative study was conducted with other series published in the literature.
PatientsThe study included 17 patients diagnosed with choledochal cyst who underwent surgery between January 1, 1988 and December 1, 2019. The inclusion criteria were: patients with anatomic pathological confirmation of the choledochal cyst diagnosis after surgery.
The selection criteria of the comparative descriptive analysis were: 1) the 5 published series with the largest volume of patients who had been diagnosed with choledochal cyst and had been treated surgically; 2) series published in the last 20 years; 3) data recorded according to the Todani classification; 4) studies that included clinical data and diagnostic methods. The exclusion criteria were: 1) series with patients who had not undergone surgery; 2) exclusively pediatric series; 3) cases not classified according to the Todani classification.
VariablesThe demographic, clinical and analytical data of the patients have been analyzed, as well as cyst type, diagnostic methods, surgical technique used, follow-up results, and short- and long-term complications.
Statistical analysisCategorical variables were described as percentages, and continuous variables were expressed as mean and standard deviation (SD) if they followed normal distribution, and as median and interquartile range if they did not follow normal distribution. The analysis of normality was carried out with the Shapiro-Wilk test. SPSS Statistics® v.22. was used to develop the study.
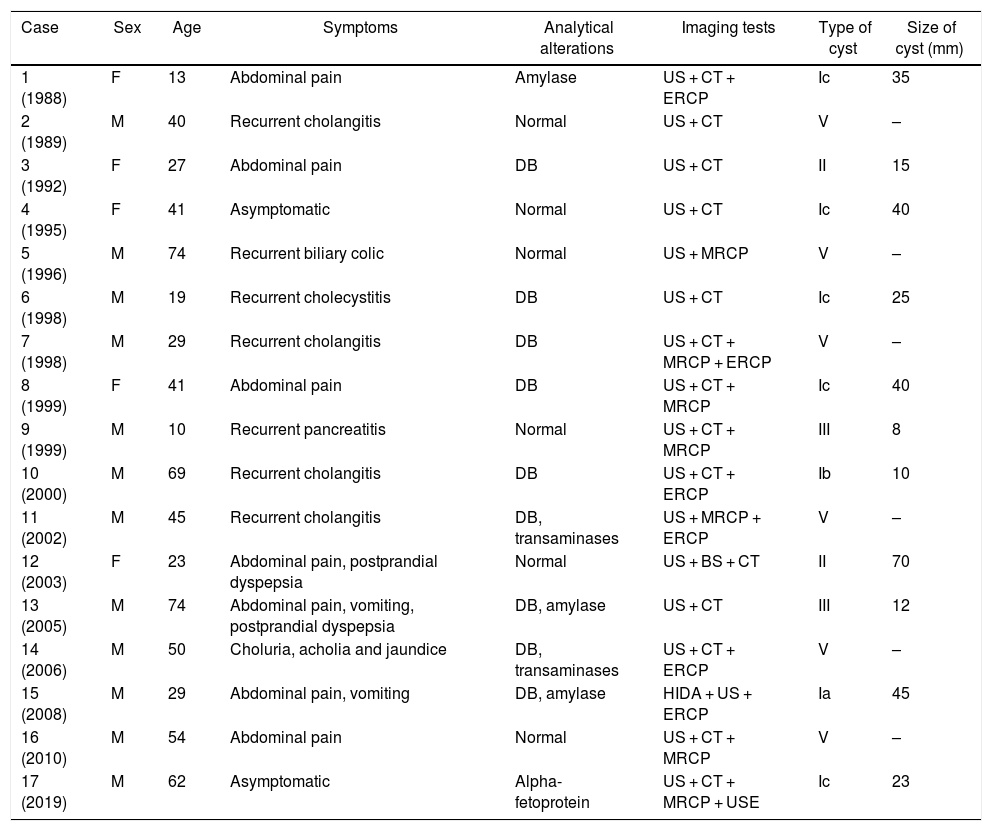
ResultsSeventeen patients were included in the study, and the mean follow-up was 5 years ( 1-15). The sociodemographic variables and preoperative characteristics of the patients are shown in Table 1. The distribution by sex was 11 men (64.7%) and 6 women (35.3%), with a mean age of 41.2 years (SD: 20.47). As for the Todani classification, most of the cysts were type I (7 patients; 41.2%), followed by type V (6 patients; 35.3%) and 11.8% type II and III cysts; there were no type IV cases. The most frequent clinical manifestations at diagnosis were abdominal pain in 58.8% of the patients, followed by jaundice (41.2%) and vomiting (35.3%). Four patients (23.5%) presented recurrent cholangitis as the main condition. In 2 cases (11.6%), the diagnosis was incidental in asymptomatic patients. In all cases, the initial diagnostic imaging technique was abdominal ultrasound, followed by CT in 82.4%. The diagnosis was confirmed by magnetic resonance cholangiopancreatography (MRCP) in 63.6% of the patients, endoscopic retrograde cholangiopancreatography (ERCP) in 35.3%, and endoscopic ultrasound in only one patient (5.9%). In 55.6% of the cases, cysts between 2-4 cm were observed, while 22.2% had cysts greater than 4 cm. Table 2 shows the surgical technique used in each case and the complications recorded according to the type of cyst and their management.
Sociodemographic and preoperative characteristics.
| Case | Sex | Age | Symptoms | Analytical alterations | Imaging tests | Type of cyst | Size of cyst (mm) |
|---|---|---|---|---|---|---|---|
| 1 (1988) | F | 13 | Abdominal pain | Amylase | US + CT + ERCP | Ic | 35 |
| 2 (1989) | M | 40 | Recurrent cholangitis | Normal | US + CT | V | – |
| 3 (1992) | F | 27 | Abdominal pain | DB | US + CT | II | 15 |
| 4 (1995) | F | 41 | Asymptomatic | Normal | US + CT | Ic | 40 |
| 5 (1996) | M | 74 | Recurrent biliary colic | Normal | US + MRCP | V | – |
| 6 (1998) | M | 19 | Recurrent cholecystitis | DB | US + CT | Ic | 25 |
| 7 (1998) | M | 29 | Recurrent cholangitis | DB | US + CT + MRCP + ERCP | V | – |
| 8 (1999) | F | 41 | Abdominal pain | DB | US + CT + MRCP | Ic | 40 |
| 9 (1999) | M | 10 | Recurrent pancreatitis | Normal | US + CT + MRCP | III | 8 |
| 10 (2000) | M | 69 | Recurrent cholangitis | DB | US + CT + ERCP | Ib | 10 |
| 11 (2002) | M | 45 | Recurrent cholangitis | DB, transaminases | US + MRCP + ERCP | V | – |
| 12 (2003) | F | 23 | Abdominal pain, postprandial dyspepsia | Normal | US + BS + CT | II | 70 |
| 13 (2005) | M | 74 | Abdominal pain, vomiting, postprandial dyspepsia | DB, amylase | US + CT | III | 12 |
| 14 (2006) | M | 50 | Choluria, acholia and jaundice | DB, transaminases | US + CT + ERCP | V | – |
| 15 (2008) | M | 29 | Abdominal pain, vomiting | DB, amylase | HIDA + US + ERCP | Ia | 45 |
| 16 (2010) | M | 54 | Abdominal pain | Normal | US + CT + MRCP | V | – |
| 17 (2019) | M | 62 | Asymptomatic | Alpha-fetoprotein | US + CT + MRCP + USE | Ic | 23 |
BS: barium swallow; CT: computed tomography; DB: direct bilirubin; ERCP: endoscopic retrograde cholangiopancreatography; F: female; HIDA: hepatobiliary iminodiacetic acid scan; M: male; MRCP: magnetic resonance cholangiopancreatography; US: ultrasound; USE: ultrasound endoscopy.
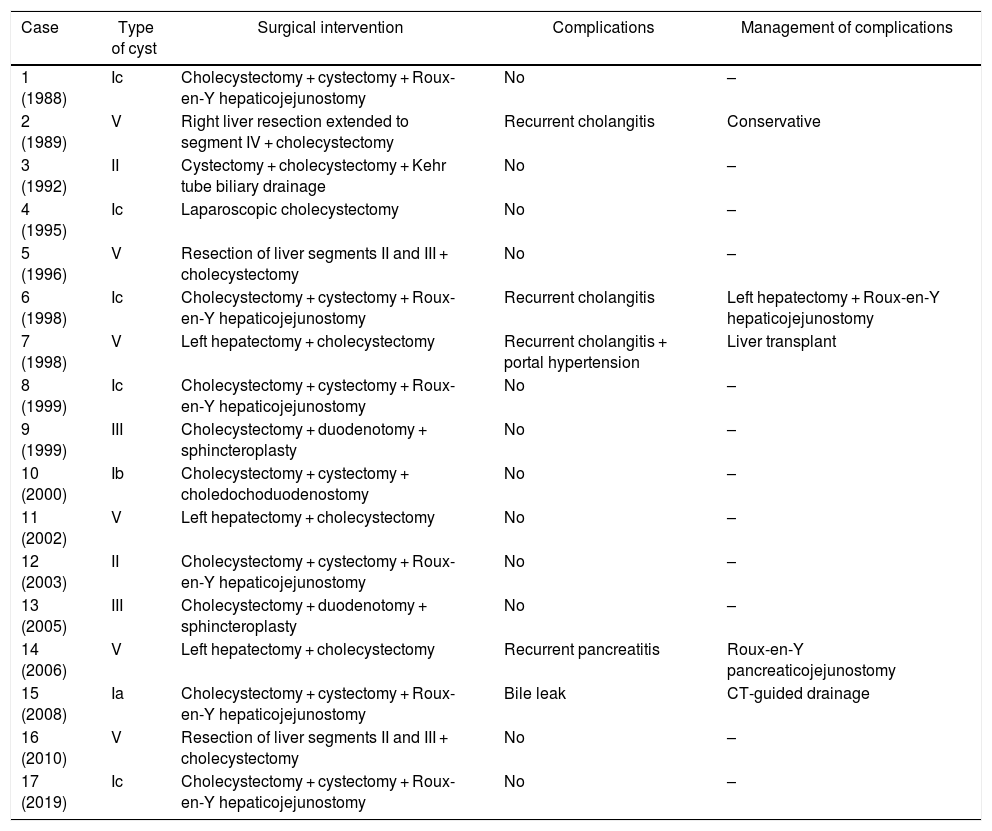
Surgical intervention, complications and management.
| Case | Type of cyst | Surgical intervention | Complications | Management of complications |
|---|---|---|---|---|
| 1 (1988) | Ic | Cholecystectomy + cystectomy + Roux-en-Y hepaticojejunostomy | No | – |
| 2 (1989) | V | Right liver resection extended to segment IV + cholecystectomy | Recurrent cholangitis | Conservative |
| 3 (1992) | II | Cystectomy + cholecystectomy + Kehr tube biliary drainage | No | – |
| 4 (1995) | Ic | Laparoscopic cholecystectomy | No | – |
| 5 (1996) | V | Resection of liver segments II and III + cholecystectomy | No | – |
| 6 (1998) | Ic | Cholecystectomy + cystectomy + Roux-en-Y hepaticojejunostomy | Recurrent cholangitis | Left hepatectomy + Roux-en-Y hepaticojejunostomy |
| 7 (1998) | V | Left hepatectomy + cholecystectomy | Recurrent cholangitis + portal hypertension | Liver transplant |
| 8 (1999) | Ic | Cholecystectomy + cystectomy + Roux-en-Y hepaticojejunostomy | No | – |
| 9 (1999) | III | Cholecystectomy + duodenotomy + sphincteroplasty | No | – |
| 10 (2000) | Ib | Cholecystectomy + cystectomy + choledochoduodenostomy | No | – |
| 11 (2002) | V | Left hepatectomy + cholecystectomy | No | – |
| 12 (2003) | II | Cholecystectomy + cystectomy + Roux-en-Y hepaticojejunostomy | No | – |
| 13 (2005) | III | Cholecystectomy + duodenotomy + sphincteroplasty | No | – |
| 14 (2006) | V | Left hepatectomy + cholecystectomy | Recurrent pancreatitis | Roux-en-Y pancreaticojejunostomy |
| 15 (2008) | Ia | Cholecystectomy + cystectomy + Roux-en-Y hepaticojejunostomy | Bile leak | CT-guided drainage |
| 16 (2010) | V | Resection of liver segments II and III + cholecystectomy | No | – |
| 17 (2019) | Ic | Cholecystectomy + cystectomy + Roux-en-Y hepaticojejunostomy | No | – |
The median duration of surgery was 210 min (range 120-360). In type I cysts, cholecystectomy was performed with cystectomy and biliary bypass in 6 of the 7 cases (85.7%). The bypass technique used was Roux-en-Y hepaticojejunostomy in 5 patients and choledochoduodenostomy in one patient. In one case of type I cyst, a laparoscopic cholecystectomy was performed exclusively, without excision of the cyst, since the patient was asymptomatic and presented a duodenal duplication cyst as an anatomical anomaly, which made the bypass difficult. Two patients had type II cyst: one underwent cholecystectomy, cystectomy, and bypass (Roux-en-Y hepaticojejunostomy), while the other was managed with cholecystectomy and simple excision of the cyst with drainage of the bile duct using a Kehr tube, since the neck of the cyst was small in size. In the 2 patients with type III cyst, a cholecystectomy with duodenotomy and open sphincteroplasty was performed without requiring cystectomy due to the low risk of malignancy (lower than in type I or IV cysts). In 3 of the 6 patients with type V cyst, left hepatectomy was performed, in 2 patients segmentectomy II and III were performed, and a single patient was treated with extended right hepatectomy after preoperative portal embolization.
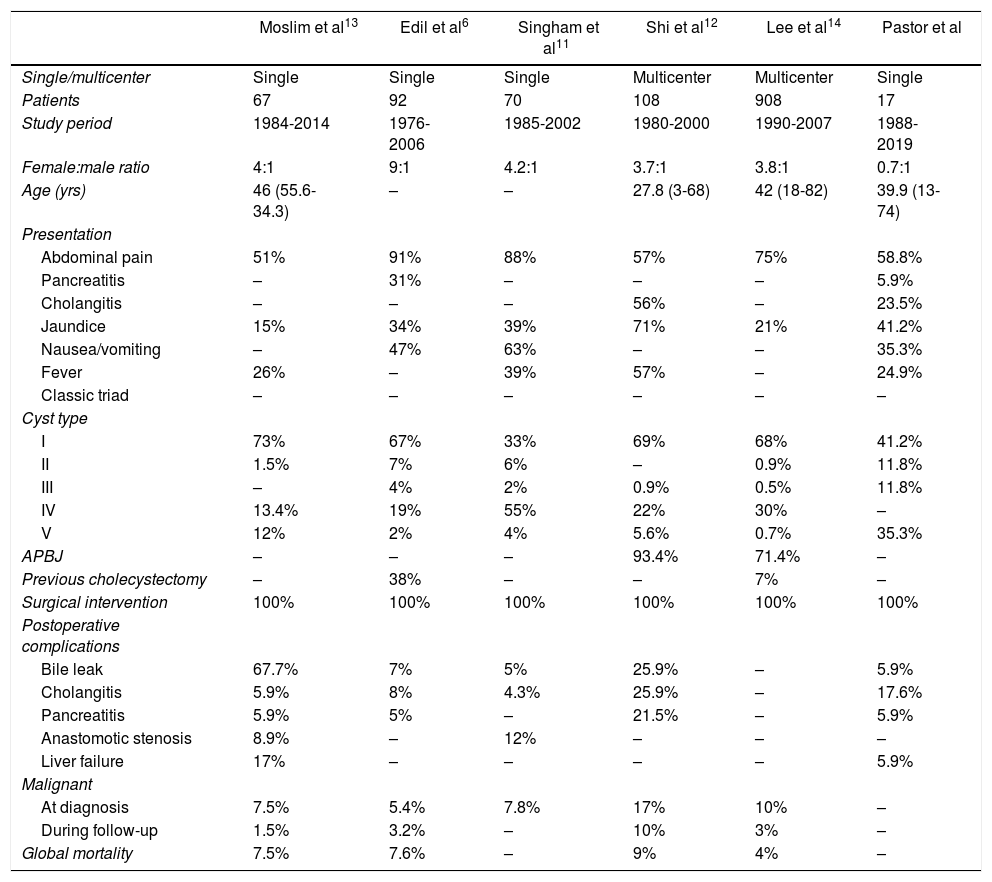
Out of the 5 patients (29.4%) who presented postoperative complications, only one patient presented a complication in the immediate postoperative period (Clavien-Dindo III-A) (Table 2). The median hospital stay was 9 days (range 4-26). The pathological diagnosis was biliary cyst in 100% of the cases, with no findings of malignancy. Postoperative mortality was 0%. During follow-up, no recurrence of the cyst or malignancy was found. Table 3 shows the comparative data of our series with the 5 most extensive series published in the last 20 years6,11–14.
Comparison of the longest series of choledochal cyst in the last 20 years and our series.
| Moslim et al13 | Edil et al6 | Singham et al11 | Shi et al12 | Lee et al14 | Pastor et al | |
|---|---|---|---|---|---|---|
| Single/multicenter | Single | Single | Single | Multicenter | Multicenter | Single |
| Patients | 67 | 92 | 70 | 108 | 908 | 17 |
| Study period | 1984-2014 | 1976-2006 | 1985-2002 | 1980-2000 | 1990-2007 | 1988-2019 |
| Female:male ratio | 4:1 | 9:1 | 4.2:1 | 3.7:1 | 3.8:1 | 0.7:1 |
| Age (yrs) | 46 (55.6-34.3) | – | – | 27.8 (3-68) | 42 (18-82) | 39.9 (13-74) |
| Presentation | ||||||
| Abdominal pain | 51% | 91% | 88% | 57% | 75% | 58.8% |
| Pancreatitis | – | 31% | – | – | – | 5.9% |
| Cholangitis | – | – | – | 56% | – | 23.5% |
| Jaundice | 15% | 34% | 39% | 71% | 21% | 41.2% |
| Nausea/vomiting | – | 47% | 63% | – | – | 35.3% |
| Fever | 26% | – | 39% | 57% | – | 24.9% |
| Classic triad | – | – | – | – | – | – |
| Cyst type | ||||||
| I | 73% | 67% | 33% | 69% | 68% | 41.2% |
| II | 1.5% | 7% | 6% | – | 0.9% | 11.8% |
| III | – | 4% | 2% | 0.9% | 0.5% | 11.8% |
| IV | 13.4% | 19% | 55% | 22% | 30% | – |
| V | 12% | 2% | 4% | 5.6% | 0.7% | 35.3% |
| APBJ | – | – | – | 93.4% | 71.4% | – |
| Previous cholecystectomy | – | 38% | – | – | 7% | – |
| Surgical intervention | 100% | 100% | 100% | 100% | 100% | 100% |
| Postoperative complications | ||||||
| Bile leak | 67.7% | 7% | 5% | 25.9% | – | 5.9% |
| Cholangitis | 5.9% | 8% | 4.3% | 25.9% | – | 17.6% |
| Pancreatitis | 5.9% | 5% | – | 21.5% | – | 5.9% |
| Anastomotic stenosis | 8.9% | – | 12% | – | – | – |
| Liver failure | 17% | – | – | – | – | 5.9% |
| Malignant | ||||||
| At diagnosis | 7.5% | 5.4% | 7.8% | 17% | 10% | – |
| During follow-up | 1.5% | 3.2% | – | 10% | 3% | – |
| Global mortality | 7.5% | 7.6% | – | 9% | 4% | – |
APBJ: anomaly of the pancreaticobiliary junction.
The management of common bile duct cysts is represented in Fig. 1.
DiscussionCurrently, there is controversy about the etiology, pathophysiology, and natural course of cystic biliary disease. Several theories have been proposed about the etiology of cysts(with no consensus), such as the presence of a APBJ causing pancreatic reflux towards the biliary tree8,9 or biliary oligoganglionosis10. In turn, the causes of malignancy associated with the cyst type are unknown.
Although bile cysts are usually diagnosed in childhood, only 2 patients (11.8%) in our study were minors. Thanks to advances in imaging studies, adult patients are being diagnosed with increasing frequency. Recent series in children and adults confirm this trend6.
The presence of the triad of abdominal pain, jaundice, and palpable mass was not found in any case in our cohort. The literature reports the presence of the complete triad in less than 20% of patients11. Out of the 17 cases, abdominal pain was the most common symptom at diagnosis (58.8%), followed by jaundice (41.2%). This coincides with other published studies5,6,11,15. Edil et al reported an incidence of pancreatitis of 30%, which is relatively high compared to our findings (5.9%)6. Two patients (11.8%) in our series did not present symptoms at diagnosis.
Ultrasound is the most commonly used imaging test for the initial diagnosis16,17. In the series by Moslim et al, MRCP was the most used method (66%) in the preoperative study, while ERCP was performed in 43% of cases13. In the group by Singham et al11, ERCP was the test of choice in 80% of patients, since at that time ERCP was more used than MRCP. Currently, MRCP has replaced ERCP as the first-line diagnostic test of choice.
Shi et al12 observed 93.4% APBJ in the patients examined with ERCP. O’Neill also reported an association of 92.2% between choledochal cysts and APBJ in 645 cases18. In none of the cases in our study was such an anomaly observed on the imaging tests performed, although ERCP was only performed in 35.3% of the cases. Although ERCP is considered the gold standard for the visualization of this anomalous junction, MRCP is an efficient, non-aggressive, uncomplicated test to detect more frequent abnormalities.
Both type I and IV cysts are the most common. Types II and V in general are rare, representing 2% and 20% of cysts reported in the literature, respectively. However, no type IV cyst has been documented in our hospital, with a predominance of type I and V cysts (41% and 35%, respectively).
The management of patients with biliary cysts depends on the cyst type and symptoms8. For patients with type I or IV cysts, complete surgical removal of the cyst is recommended with hepaticojejunostomy instead of conservative treatment16 due to the high risk of malignancy. In our study, this type of surgery was performed in 71.4% of cases.
Narayanan et al19 published a meta-analysis of 6 studies comprising 679 patients who underwent resection of a choledochal cyst, comparing hepaticojejunostomy versus hepaticoduodenostomy. The results suggest that hepaticoduodenostomy is comparable to hepaticojejunostomy in terms of benefits and results. However, a higher level of postoperative reflux/gastritis is recorded in hepaticoduodenostomy than in hepaticojejunostomy, but the hospital stay is shorter. In another series of 59 patients17, the hepaticoduodenostomy required less surgical time and allowed for faster recovery of intestinal function. However, its execution is not always feasible since it largely depends on the ease of approximation of the duodenum to the hepatic confluence after performing an extensive Kocher maneuver, allowing for a tension-free anastomosis. Out of the 7 patients with type I cyst, a choledochoduodenostomy was performed in one patient with type Ib cyst (14.3%), with no complications recorded and postoperative results similar to hepaticojejunostomy.
In type II cysts, simple removal of the cyst is suggested16,20, except in those with a complicated clinical presentation (including persistent jaundice or malignancy in the cyst) that may require more extensive resection.
Regarding type III cysts, surgical management is less clear. The treatment of symptomatic cysts is suggested, as well as asymptomatic cysts in young patients8. Sphincterotomy is often sufficient to relieve symptoms, accompanied by a biopsy of the cyst epithelium to exclude dysplasia. In the Edil et al6 series, cystic excision and surgical sphincteroplasty were performed in 50% of type III patients. In the remaining 50%, pancreaticoduodenectomy was performed for suspected malignancy. In none of the patients in our study was the cyst removed, and the procedure was limited to duodenotomy and sphincteroplasty with biopsy of the cyst epithelium to rule out dysplasia.
The treatment of type V cysts is mainly based on supportive measures and should be individualized, focusing on the management of frequent complications such as recurrent cholangitis and sepsis21,22. Partial hepatectomy can be curative in patients in whom the disease is limited to a single liver lobe, with reduced postoperative morbidity and good long-term results (10-year survival 82%)23. In our series, we found 6 patients with type V cysts, one of which required liver transplantation due to postoperative complications. Edil et al6 defined cholangitis (8%) as the most frequent complication, followed by bile leak (7%). The Moslim group most frequently recorded intra-abdominal collections (11.9%) and bile leaks (10.5%) managed mainly with percutaneous drainage13. In contrast, the recorded incidence of cholangitis was 6%. In our study, the main complication during follow-up was cholangitis in 17.4%. Only one of the cases (5.8%) presented postoperative biliary fistula, managed with CT-guided percutaneous drainage.
The risk of malignancy increases with age, being lower in the first decade of life (0.7%) and increasing to 10% after the second decade. Lee et al14 found malignant neoplasms of the biliary tract in 9.9% of the cases, 50% of which were cholangiocarcinoma, while Shi et al12 collected a greater number —some 17% of cases. However, published data probably overestimate the risk of cancer in biliary cysts since most series include only symptomatic patients with complications, including malignancy. To calculate the true risk of malignancy, the incidence of asymptomatic bile cysts in the population should be used as the denominator, a value that is unknown. Regarding the appropriate follow-up for patients who have undergone surgery for a biliary cyst, there is no consensus or standardization. The value of regular imaging tests to detect malignancy is not proven, but an annual imaging test seems advisable in cases with partial cyst resection. Partial resection should not be performed unless complete resection is impossible. In these patients, annual imaging tests are required due to the risk of malignancy. The pathological study will determine the closeness of follow-up according to the presence of dysplasia and grade. In cases of type I and IV cysts, radiological follow-up also seems advisable due to their greater risk of malignancy.
Given the retrospective nature of the study, inherent biases are associated with its design. The small number of included cases makes it impossible to draw conclusions with a high level of scientific evidence. Given the low incidence of the disease, the study period went back 30 years, so the lower availability of diagnostic tests present at that time and changes in perioperative patient care may introduce bias.
ConclusionCholedochal cysts are a rare pathology that requires a high level of suspicion for diagnosis. Correct classification is essential since the treatment of the cyst is determined by the type of cyst, ranging from cystectomy with or without associated bypass to hepatectomy or transplantation. Given the low incidence of choledochal cysts, treatment should be centralized in specialized centers. Multicenter studies are necessary to establish adequate treatment and follow-up guidelines based on greater scientific evidence.
FundingNo funding or grants were received for this manuscript.
Conflict of interestsThere are no conflicts of interests to declare.
Please cite this article as: Pastor P, Ocaña J, González A, Nuñez J, García A, García JC, et al. Manejo quirúrgico de los quistes de colédoco: análisis retrospectivo y comparativa histórica. Cir Esp. 2022:100:39–45.