Granular cell tumor is a very rare entity (0.03%) with controversial management, due to its low incidence and its usually benign behavior (98%). Its location in the digestive tract is unusual (3–11%), being the esophagus the most frequently affected organ, with about 400 published cases. However, the incidence in the cervical esophagus is anecdotal (20 published cases).
We present a patient with an esophageal granular cell tumor that invaded trachea, thyroid and soft tissues, performing a block resection of the cervical esophagus, two tracheal rings, thyroid and prethyroid musculature. For digestive reconstruction, a free jejunum graft with microvascular anastomosis was made and tracheal reconstruction was performed using term-terminal anastomosis.
The importance of the case is twofold: to contribute more casuistry, and to describe a highly complex surgical technique never indicated in this type of tumors, due to its rarely aggressive character.
El tumor de células granulares es una entidad muy infrecuente (0,03%) y con un manejo terapéutico controvertido debido a su escasa incidencia y a su comportamiento habitualmente benigno (98%). Su localización en el tracto digestivo es inusual (3–11%), y el esófago es el órgano más frecuentemente afectado, con unos 400 casos publicados. Sin embargo, la incidencia en el esófago cervical es anecdótica (20 casos publicados).
Presentamos un paciente con un tumor de células granulares esofágico que invadía tráquea, tiroides y partes blandas, realizándose una resección en bloque de esófago cervical, dos anillos traqueales, tiroides y musculatura pretiroidea. Para la reconstrucción digestiva se empleó un injerto de yeyuno libre con anastomosis microvascular y reconstrucción traqueal mediante anastomosis termino-terminal.
La importancia del caso es doble: aportar mayor casuística y describir una técnica quirúrgica altamente compleja nunca indicada en este tipo de tumores debido a su carácter raramente agresivo.
Granular cell tumors are a very rare entity. First described in 1926 by Abrikossoff,1 their origin lies in the Schwann cells. They usually present with benign behavior, and their invasive behavior is rare (2%).2
These tumors are located in the digestive tract in 3% to 11% of cases,3–5 and the most frequently affected organ is the esophagus, with about 400 published cases.2 However, their incidence in the cervical esophagus is anecdotal, with only 20 published cases.6
We describe the case of a 38-year-old male with no relevant medical-surgical history who consulted for dysphagia of one year of evolution. The study was started with fiberoptic gastroscopy, which revealed a heterogeneous subepithelial solid nodular lesion some 16 to 21cm from the dental arcade. The study was completed with endoscopic ultrasound, and the lesion was observed to measure 24×22mm in diameter, dependent on the deep layers of the esophageal wall and possible infiltration of the right thyroid lobe. Cervicothoracic CT scan confirmed the cervical esophageal lesion with invasion of the posterior wall of the trachea and right thyroid lobe. Fiberoptic bronchoscopy demonstrated the described exophytic lesion 2cm caudal to the glottis, in the membranous part of the tracheal area, which occluded 30% of the tracheal lumen; biopsies were taken. The pathology study confirmed the diagnosis of granular cell tumor. We decided to conduct radical excision surgery, resecting and reconstructing the airway and digestive tract in the same operation, while preserving the patient’s ability to speak and thus avoiding definitive tracheostomy, which was a surgical challenge.
Surgical techniqueAn enlarged transverse cervical incision was used with dissection done by planes, revealing an esophageal tumor with cranial extension just below the hypopharynx and caudal extension to the level of the upper thoracic esophagus. There was invasion of the posterior tracheal side, but the anterior cricoid lamina was preserved; two tracheal rings were compromised.
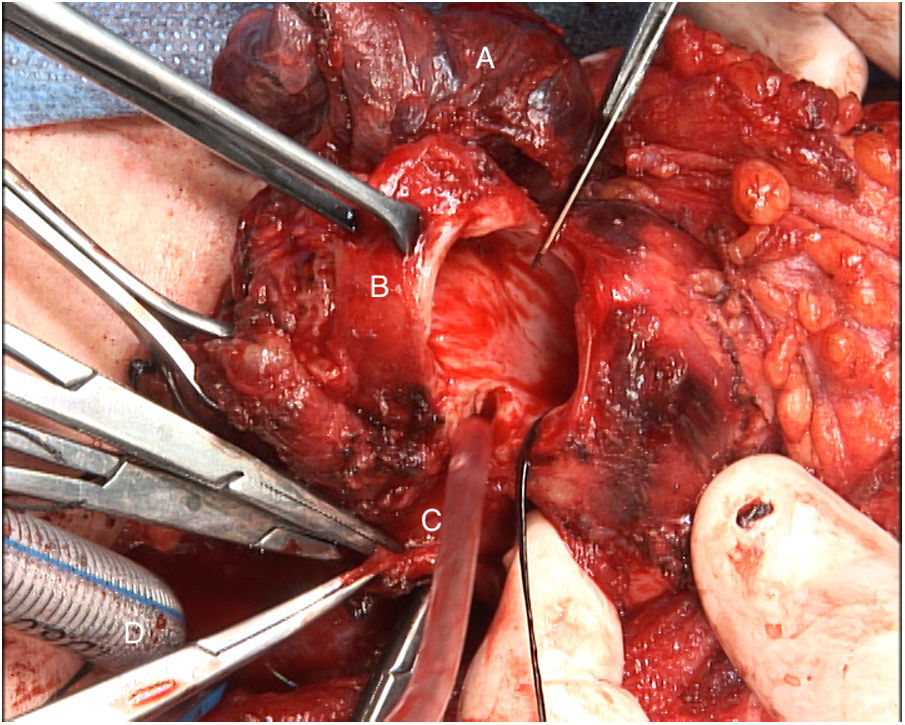
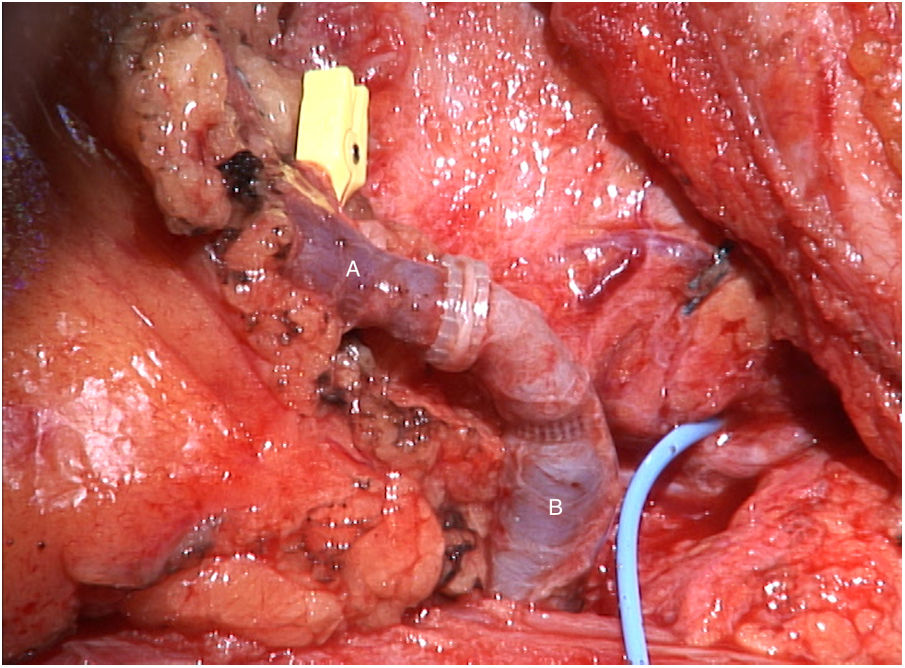
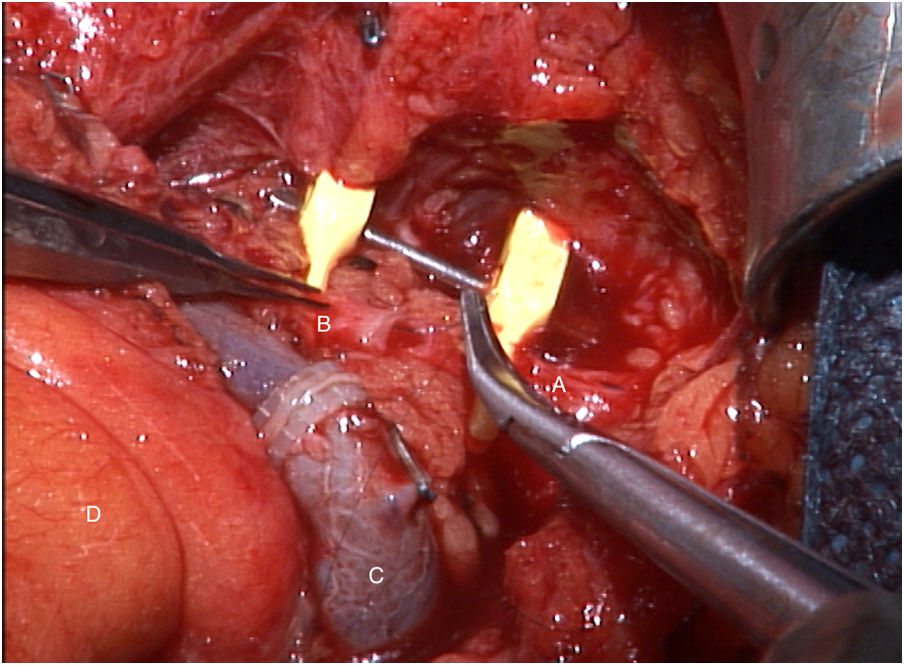
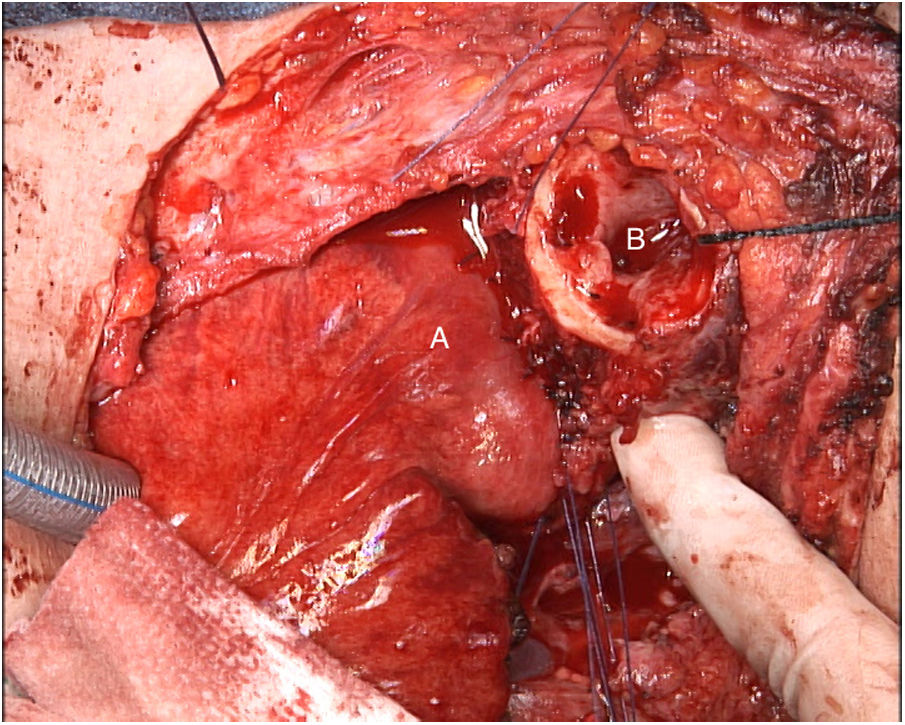
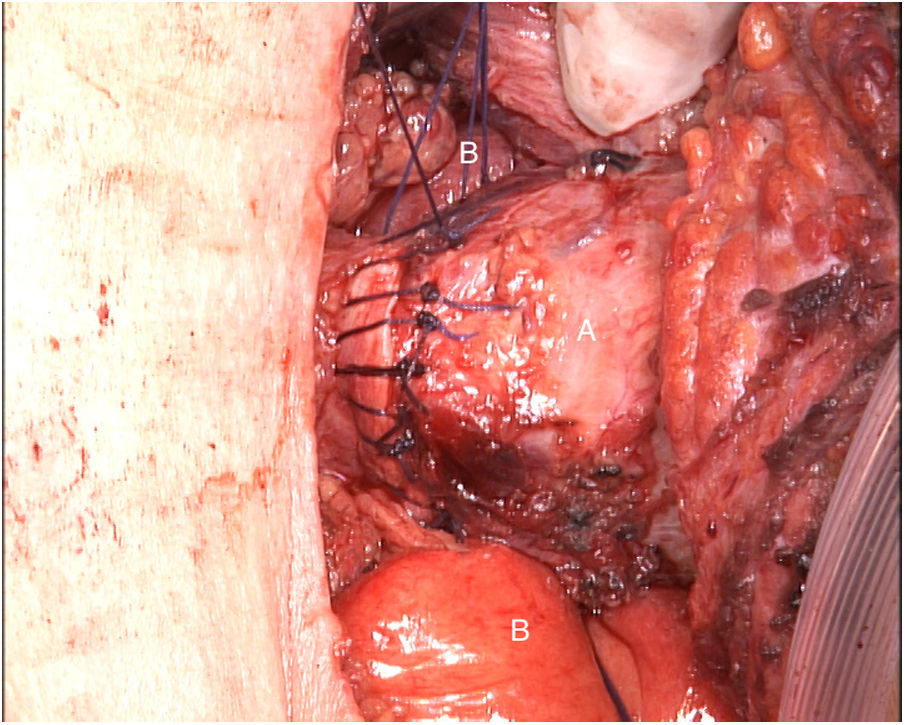
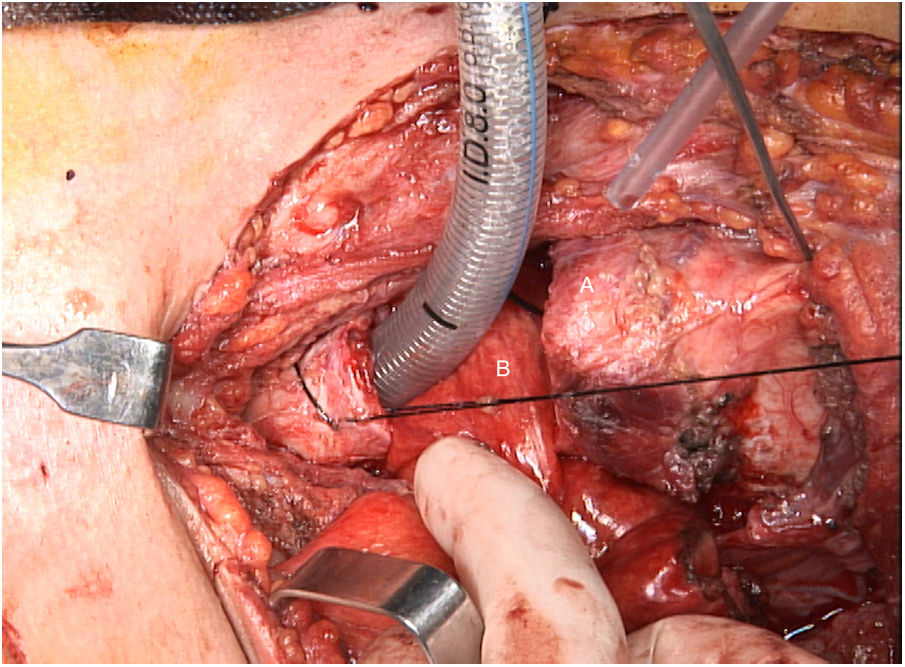
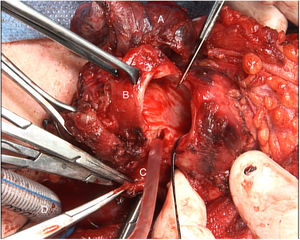
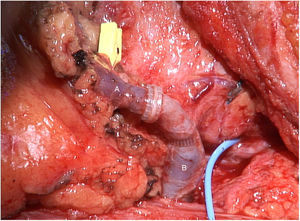
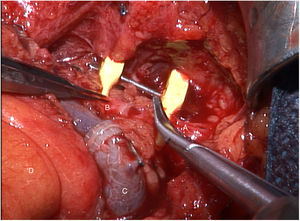
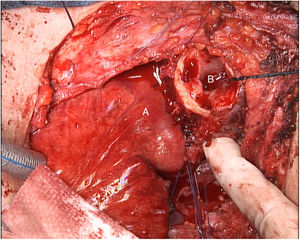
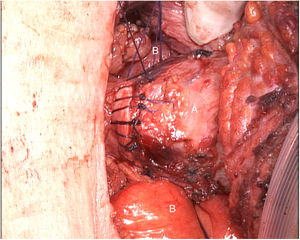
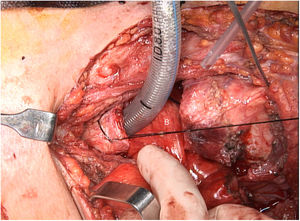
The tumor invaded the right thyroid lobe and the right recurrent nerve. The plane of separation between these structures and the surrounding tissues could not be visualized. An en bloc resection of all these structures (Fig. 1), including prethyroid musculature and soft tissues, was performed to ensure the resection margin and avoid tumor manipulation. For the reconstruction of the digestive tract, a free jejunal graft was indicated as it was a short segment of the esophagus. By means of laparotomy, we resected about 30cm of the jejunal loop, preserving its vessels at the root. Subsequently, in the cervical stage, the thyrolinguofacial venous trunk and the left internal mammary artery were dissected through a transverse incision in the second left intercostal space and subsequently uncrossed until it was positioned at the cervical level. The jejunal-thyrolinguofacial microvascular anastomosis was performed using circular mechanical end-to-tend suture (Fig. 2), and the manual end-to-end arterial anastomosis was created with simple Ethilon® 9/0 sutures between the jejunal and internal mammary arteries (Fig. 3). Correct vascularization of the graft was confirmed by indocyanine green. The digestive anastomosis was monolayer manual hypopharynx-jejunal end-to-side with simple Vicryl 3/0 sutures (Fig. 4) and manual jejunal-esophageal side-to-end with the same characteristics, with the difficulty of exposing a good retrosternal surgical field. The procedure was completed with a feeding jejunostomy.
To reconstruct the airway, a manual end-to-end anastomosis was created with simple Vicryl 3/0 sutures, with a protective tracheostomy distal to the anastomosis (Fig. 5).
The postoperative evolution was satisfactory. Eight days later, a cervical/thoracoabdominal CT scan was performed with intravenous and oral contrast, which confirmed the correct vascularization of the graft and no leaks of the anastomoses. Oral intake was initiated and well tolerated. The control bronchoscopy ruled out anastomotic dehiscence and revealed paralysis of the vocal cords in the paramedial position, but some phonation was possible.
Twelve months after the procedure, the patient tolerates an oral diet without the need for nutritional support, while avoiding liquid textures due to pulmonary aspiration episodes but perfectly tolerating other textures. The tracheostomy remains closed and only requires reopening under conditions of great physical exertion.
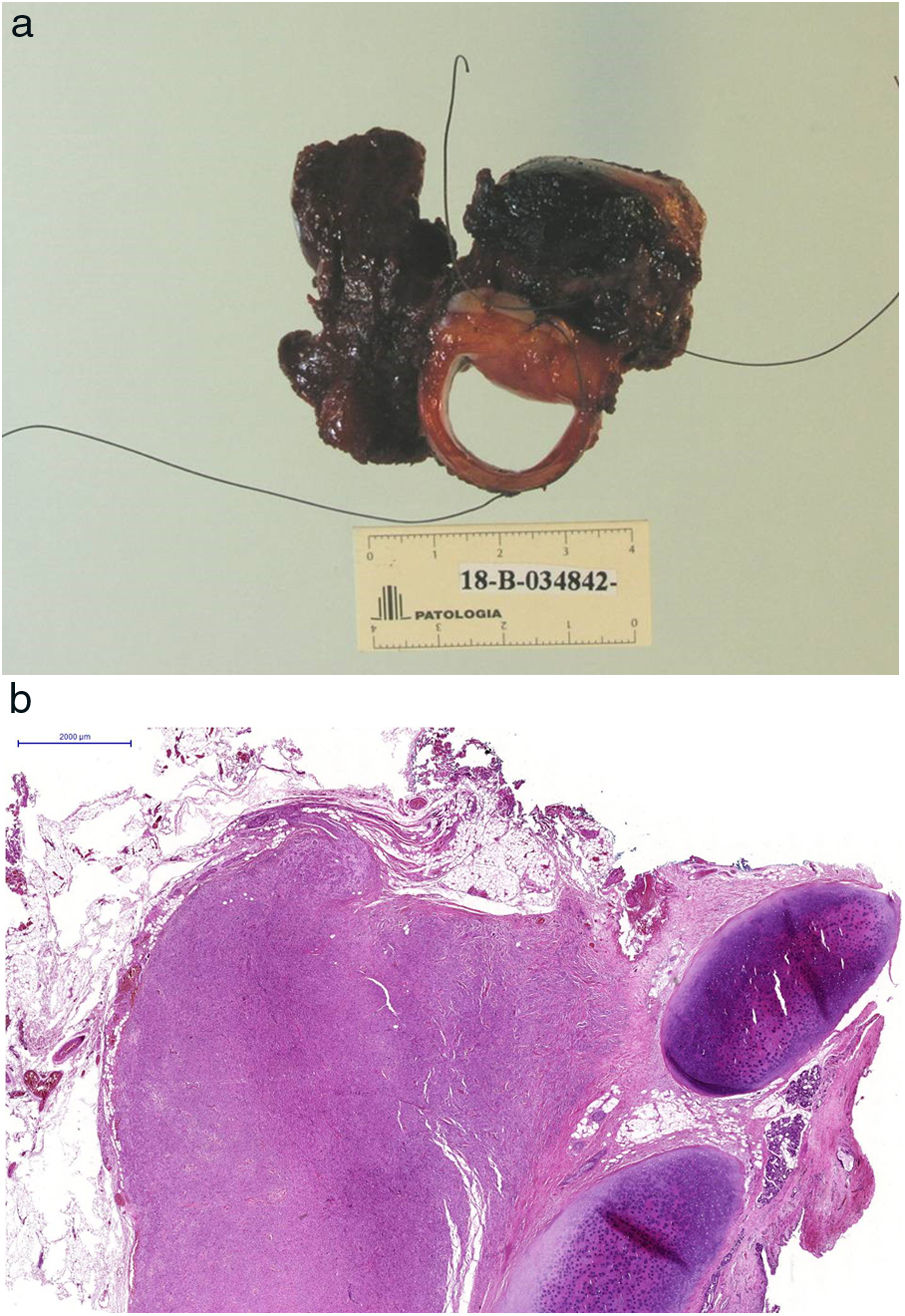
The pathological examination described a lesion made up of polygonal cells with broad and granular cytoplasm, a small round nucleus, arranged in groups with an infiltrative pattern and perineural invasion. The immunohistochemical study was positive for S-100 and enolase, compatible with a granular cell tumor showing a transmural invasive pattern of the esophagus, trachea, soft tissue and thyroid parenchyma (Fig. 6A–C).
(A) Surgical specimen consisting of the trachea, esophagus and right thyroid lobe; (B) Panoramic microscopic image in which the tumor is identified in relation to the tracheal cartilage; (C) Optical microscope image showing that the tumor infiltrates the tracheal wall with extensive involvement of the submucosa.
Granular cell tumor is a very rare entity (0.03%).6 Its therapeutic management is controversial due to its low incidence and its usually benign behavior.
In tumors that are <1cm and asymptomatic, most authors advocate clinical follow-up. However, Huang et al.6 defend surgical treatment when the location is cervical, regardless of size and symptoms. This posture is based on the more aggressive behavior of tumors in this area, where they rapidly invade important neighboring structures. The case we present is an example of the invasive behavior described by Huang in the cervical location and requires an en bloc surgical resection of all invaded structures.
In 1–3cm tumors with no invasion of the muscularis propria, endoscopic therapy (diathermy, polypectomy loop resection, endoscopic mucosal resection, or endoscopic submucosal dissection) is advocated and has been gaining acceptance thanks to its low morbidity.6
Most authors recommend surgical treatment for tumors >3cm, with invasion of the muscularis propria or presence of three or more signs of aggressiveness described by Fanburg-Smith et al.:7 tumor necrosis, cells arranged in a spindle, pleomorphism, large nucleolus, high nucleus/cytoplasm ratio or ≥2 mitoses per 10 magnification fields ×200.
It is important to emphasize that tumors with benign histological characteristics can also metastasize8 or have a malignant invasive behavior.9
In our case, surgical treatment was indicated due to the size of the tumor and the invasion of neighboring organs. For the reconstruction of the digestive tract, as it was a short segment of the esophagus, we opted for a free jejunal graft with microvascular anastomosis. In our group, in cases where a short segment cervical esophageal resection was required, this was our first reconstructive option compared to other repair techniques, such as gastroplasty10 or ‘supercharged’ ileocoloplasty.11 The advantages of this technique are: the avoidance of total esophagectomy and the postoperative morbidity that this entails; preservation of the esophagus and stomach function; creation of a proximal anastomosis without tension by achieving a plasty of adequate length and being able to place it wherever we want; and creation of a microvascular anastomosis between vessels that are similar in caliber (not so in supercharged ileocoloplasty), which makes it easier and avoids ischemic events.
The challenges of the surgical technique include: the preservation of the cricoid rostrum and with it the ability to speak; the reconstruction of the digestive tract with a microvascular graft; and the creation of a tension-free tracheal anastomosis due to the space occupied by the free jejunal graft, making it difficult to bring together the tracheal ends (Fig. 7).
The importance of this case report is twofold: it contributes another case to the literature (only 20 cases of granular cell tumors of the cervical esophagus reported to date)6 and describes a highly complex surgical technique never before indicated in this type of tumors, due to the aggressive nature of this tumor that compromised the digestive tract and the airway.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Miró M, Rivas F, López A, Farran L. Esofaguectomía cervical más resección traqueal e injerto de yeyuno libre como tratamiento de un tumor de células granulares esofágico. Cir Esp. 2021;99:147–151.