Angiosarcomas are very rare, aggressive tumours originating from endothelial cells. They are found in different organs, but have a greater affinity for skin tissue.
Depending on their aetiology, they can be classified as primary, secondary to chronic lymphoedema (Stewart-Treves) and radio-induced angiosarcomas (RIAS).
The breast is the most common site of RIAS. However, it accounts for less than .05% of malignant breast pathology and 2%–10% of sarcomatous pathology.1
It affects women with a mean age at diagnosis of 70 years and a previous history of breast neoplasia treated by radiotherapy.
Clinically, it presents as purplish lesions that appear with an average latency of 6 years in the irradiated area.2
We present the cases of three patients diagnosed with radioinduced angiosarcoma in our centre.
Case 1. An 87 year-old woman operated on in 2003 for infiltrating ductal carcinoma (IDC) (T2N0M0) with hormone receptors (HR) + Her-2. Quadrantectomy with lymphadenectomy was performed (with negative anatomopathological result for infiltration) followed by radiotherapy (50 Gys left breast + 60 Gys in the tumour bed), chemotherapy (cyclophosphamide, methotrexate, 5-FU) and hormone therapy with tamoxifen.
Seven years later she was diagnosed with angiosarcoma of the left breast after biopsy of new lesions in the irradiated area. A left mastectomy and adjuvant treatment with doxorubicin was indicated. The following year she presented three episodes of local recurrence, treated by surgical extensions. Since then, the disease has been stable.
Case 2. A 75-year-old patient, operated on in 2000 and 2010 for bilateral metachronous IDC (T1N0M0) RH+ Her-2, with conservative surgical treatment in both cases after neoadjuvant chemotherapy with docetaxel and cyclophosphamide. She subsequently received radiotherapy (50 Gys in the breast + 65 Gys in the tumour bed) and hormone therapy with letrozole.
Ten years later she was diagnosed with angiosarcoma of the right breast after biopsy of a new violaceous nodule in the superointernal quadrant. Radical excision of the lesion with reconstruction using two advancement flaps was indicated. The patient continues to be followed up without requiring adjuvant treatment.
Case 3. 67-year-old woman, operated on in 2014 for IDC of the right breast (T2N0M0) RH+ Her-2. Quadrantectomy and deferred axillary lymphadenectomy were performed due to macrometastasis in the sentinel lymph node. She subsequently received radiotherapy (40 Gys in the right breast + 12 Gys in the tumour bed), chemotherapy (epirubicin, cyclophosphamide, 5-FU) and hormone therapy with tamoxifen.
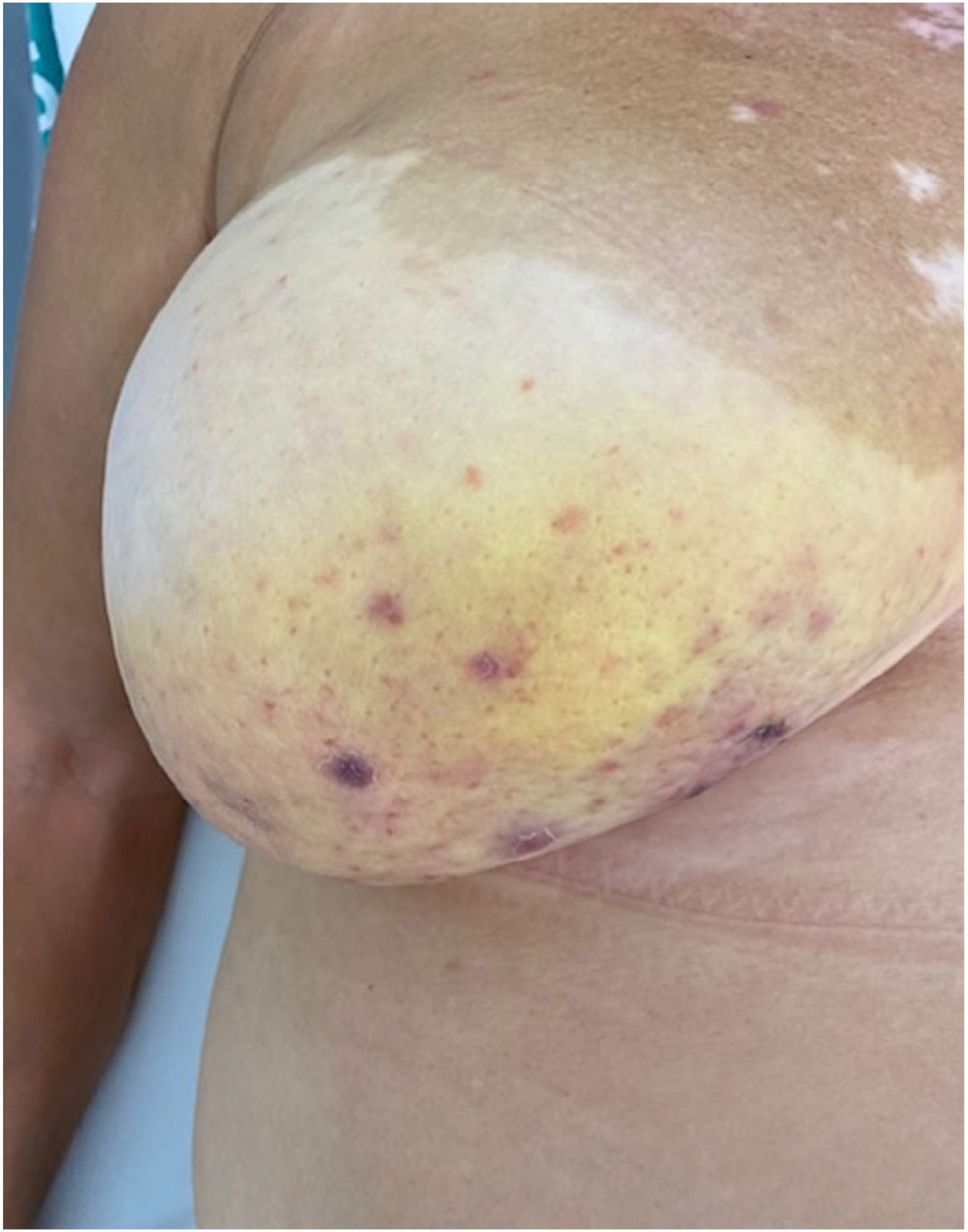
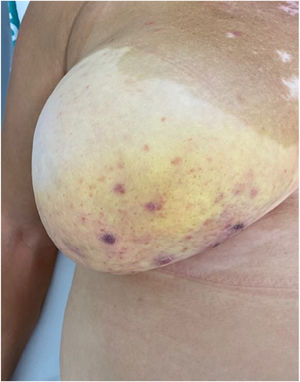
Six years later she was diagnosed with angiosarcoma of the right breast after biopsy of two separate lesions in the area of irradiation. Surgery was rejected due to the impossibility of achieving free margins. The patient was initially treated with sunitinib, and is currently being treated with nivolumab, with rapid progression of the disease after 3 months of treatment (Figs. 1 and 2).
Breast-conserving surgery associated with radiotherapy has demonstrated an overall survival similar to mastectomy in different clinical trials carried out in Europe (Veronesi)3 and the United States (Fisher),4 and is therefore considered the first choice in the surgical treatment of breast cancer, increasing the use of high-dose radiotherapy (>40 Gys)5 and secondarily breast RIAS.
The late appearance of skin lesions in the irradiated area should guide us in the diagnosis of this pathology. The imaging techniques of choice are magnetic resonance imaging and computed tomography; however, the images they provide are difficult to interpret and are not pathognomonic. Therefore, to confirm the diagnosis, a biopsy of the lesion must always be performed and the Cahan criteria described in 19486 must be met. These are:
- □
Previous radiotherapy with a latency period until the appearance of the tumour. In our series, the average latency period was 7.66 years.
- □
Implantation zone within the irradiated area.
- □
Pathological anatomy compatible with angiosarcoma.
The only curative treatment is surgery, and mastectomy is the most commonly used technique. Lesions are usually multifocal, so achieving a resection with free margins is complex, which is reflected in a high recurrence rate (52–94%), usually occurring in the first year after resection.7
Anthracyclines (doxorubicin) have traditionally been used as treatment for disseminated disease, with poor results. There are promising studies in development of immunotherapeutic drugs directed mainly against endothelial growth factor, most commonly used at present, without scientific evidence to recommend their use.8
Paradoxically, the use of radiotherapy as an adjuvant treatment for radioinduced sarcoma seems to reduce the rate of tumour recurrence, according to published studies. Publicados.9
Despite the use of aggressive treatments, these patients have an unfavourable prognosis, with overall survival of between 10.8 and 33 months, with a 5-year survival rate of around 20%.10 In our series, we cannot draw conclusions regarding overall survival due to the short follow-up period and the small number of cases.
Despite the rarity of this entity, it is crucial to train healthcare personnel to be able to make an early diagnosis and differentiate it from other post-radiation breast lesions, such as radiodermatitis or local haematoma, which appear earlier. The treatment of advanced disease requires the development of new effective systemic therapies to reduce the recurrence rate and increase survival.
FinancingThe authors declare no source of funding was used.
Conflict of interestsThe authors have no conflict of interests to declare.
Thanks to the General and Digestive Surgery Service and the Radiation Oncology Service of the Miguel Servet University Hospital.
Please cite this article as: Chóliz Ezquerro J, Casamayor Franco MC, Aparicio López D, Hernando Almudí E, Ibañez Carreras R. Angiosarcoma radioinducido de mama. Una rara complicación de la cirugía conservadora. Cir Esp. 2022;100:520–522.