Neurofibromatosis type 1 (NF1) is an autosomal dominant hereditary syndrome with an incidence of 1:3000 births; it is caused by alterations in the NF1 gene, which involve the development of different tumors.1,2 Its gastrointestinal manifestations can lead to acute gastrointestinal hemorrhages, which endanger the life of the patient.3,4 Although this situation is exceptional, diagnostic suspicion is essential to establish appropriate treatment, and decision making should be individualized.
We present the case of a 74-year-old man with COPD and home oxygen therapy. He had been diagnosed with NF1 at the age of 35, but refused follow-up. The clinical symptoms began with syncope, so the patient was admitted for further studies. An abdominal computed tomography scan demonstrated images of cutaneous nodules, a solid retroperitoneal mass (neurofibroma), neuroendocrine tumors in the pancreaticoduodenal groove, and gastrointestinal stromal tumors (GIST) in the jejunum and duodenum. The patient presented an episode of rectal bleeding with hemodynamic instability, requiring transfusion of packed red blood cells and perfusion of noradrenaline. Colonoscopy and gastroscopy discovered no pathological findings. After another episode of rectal bleeding, we decided to perform urgent surgery. During the operation, multiple fibrous-looking lesions (more than 30) were identified from the angle of Treitz to the ileocecal valve, all of different sizes (up to 3cm). Suspecting that these lesions were causing the hemorrhage, we removed the 7 largest tumors in the jejunum and intestine. A large, umbilicated and fibrous lesion was observed in the cecum, and ileocecectomy and ileocolic anastomosis were performed. The gallbladder was large and the bile duct dilated, although no mass was detected in the head of the pancreas. The postoperative period was uneventful.
The pathological anatomy of the ileocecectomy piece reported diffuse intestinal ganglioneuromatosis. The pathology study of the resected jejunal tumors reported multicentric GIST with multiple nodules measuring 0.5–5Ycm; the predominant cell type was fusiform, histological grade 1, and resection margins were involved in more than one nodule.
Immunohistochemistry reported abnormal proliferation of fibers and enteric nerve plexuses in the submucosa and transmural invasion, with the presence of isolated nerve cells and small accumulations.
In the intestinal ganglioneuromatosis, positivity was reported for S-100 protein in the neural fusocellular component, negativity for CD117 (c-KIT), DOG-1, desmin, caldesmon and alpha-actin, and intense positivity of ganglion cells for calretinin.
In the multiple GIST, diffuse positivity was reported for the tumor cells for CD117 (c-KIT), DOG1 and Ki-67<1%. No change in c-KIT or PDGFR-alpha was identified, and the mutational result for exon 13 of the c-kit gene was negative.
After evaluation by the Multidisciplinary Oncology Committee for sarcomas, it was considered a multicenter wild-type GIST (negative C-KIT, negative PDGFR-alpha) with a Performance Status 3, which prevents considering treatment with tyrosine kinase inhibitors (imatinib mesylate). In the outpatient clinic visits, the patient has presented good progress, with no further episodes of rectal bleeding.
In the scientific literature from the last 10 years, there have been 3 reviews published about the gastrointestinal manifestations of NF1, and most of the references come from isolated clinical cases or short case series.
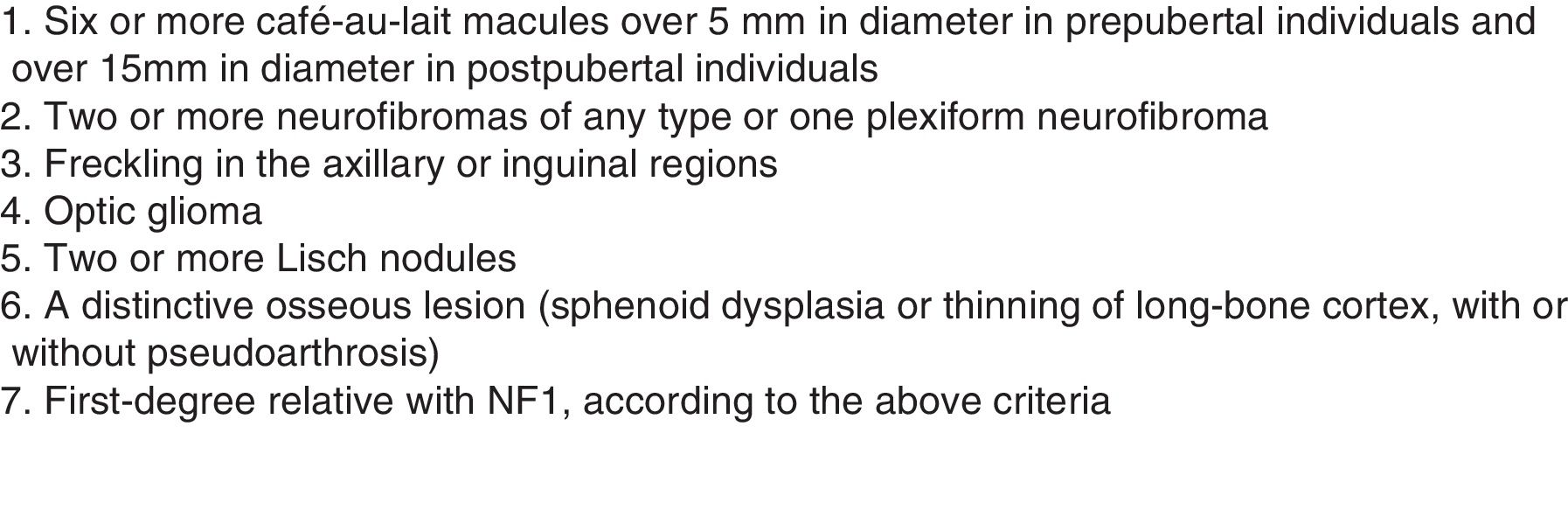
NF1 can present intra-abdominal manifestations (gastrointestinal or retroperitoneal) in 10%–25% of cases, 5% of which are symptomatic and only 2.5% require surgery.3,4 They usually appear in middle age, after cutaneous manifestations, as in the case presented (Fig. 1).
Intestinal involvement appears as tumors of neurogenic origin, neuroendocrine tumors, GIST and adenocarcinomas.3
GIST appear in less than 5% of cases of NF1. The majority of GIST associated with NF1 present as small, asymptomatic lesions with low mitotic activity and benign; only 15%–20% are malignant. NF1 typically presents with multicentric GIST in the small intestine, absence of mutations in KIT and PDGFR-alpha and, therefore, lack of response to imatinib mesylate, although overall and disease-free survival is similar to sporadic GIST. Treatment consists of surgical resection.5–8
In patients with NF1, GIST can present concomitantly with periampullary neuroendocrine tumors in a pathognomonic manner1,8 (as in the case described).
In NF1, GIST and peripheral nerve sheath tumors can also coexist in the gastrointestinal tract, which can be a sign of undiagnosed NF1. Neurofibromas are the most frequent abdominal manifestation; these are benign peripheral nerve sheath tumors that mainly affect the small intestine and retroperitoneum, although they can occur anywhere from the esophagus to the anus, including mesenteric and peritoneal connective tissue. 10% are encompassed in NF1 and can become malignant in 3%–5% of cases.1,9,10
Neurofibromatosis can also be associated with diffuse intestinal ganglioneuromatosis, which entails hyperplasia of the myenteric plexuses and enteric nerve fibers (located in the outer muscular layer) and leads to an intestinal motility disorder.9,10
In this case, the intestinal involvement with hemorrhage could have been due to intestinal GIST and diffuse intestinal ganglioneuromatosis.
Therefore, early diagnosis of abdominal manifestations is important for proper treatment and to avoid complications. In NF1, the concomitant presence of multiple GIST and peripheral nerve sheath tumors or periampullary neuroendocrine neoplasms is pathognomonic, so these entities should be considered diagnostic markers.
Please cite this article as: de la Fuente N, Rodríguez Blanco M, Cerdán G, Artigas V. Hemorragia digestiva aguda en paciente con neurofibromatosis tipo 1 afecto de múltiples GIST y ganglioneuromatosis intestinal. Cir Esp. 2019;97:237–239.