Solid pseudopapillary tumors (SPT) represent 1%–2% of pancreatic tumors.1 Described by Frantz in 1959,2 they have received several names: Frantz tumor, Hamoudi tumor, solid cystic pancreatic tumor or papillary epithelial neoplasm. In 1996, the WHO established their denomination as solid pseudopapillary tumor of the pancreas.3
The epidemiology of this neoplasm is very characteristic, appearing almost exclusively in young women in their second to third decades of life.1,4,5 It is usually an incidental finding on imaging studies that are ordered for other reasons. In spite of the fact that 15% of cases can present metastatic dissemination, it is considered a tumor with a low potential for malignancy, with overall survival rates of more than 95% and a recurrence rate lower than 10%.4,5
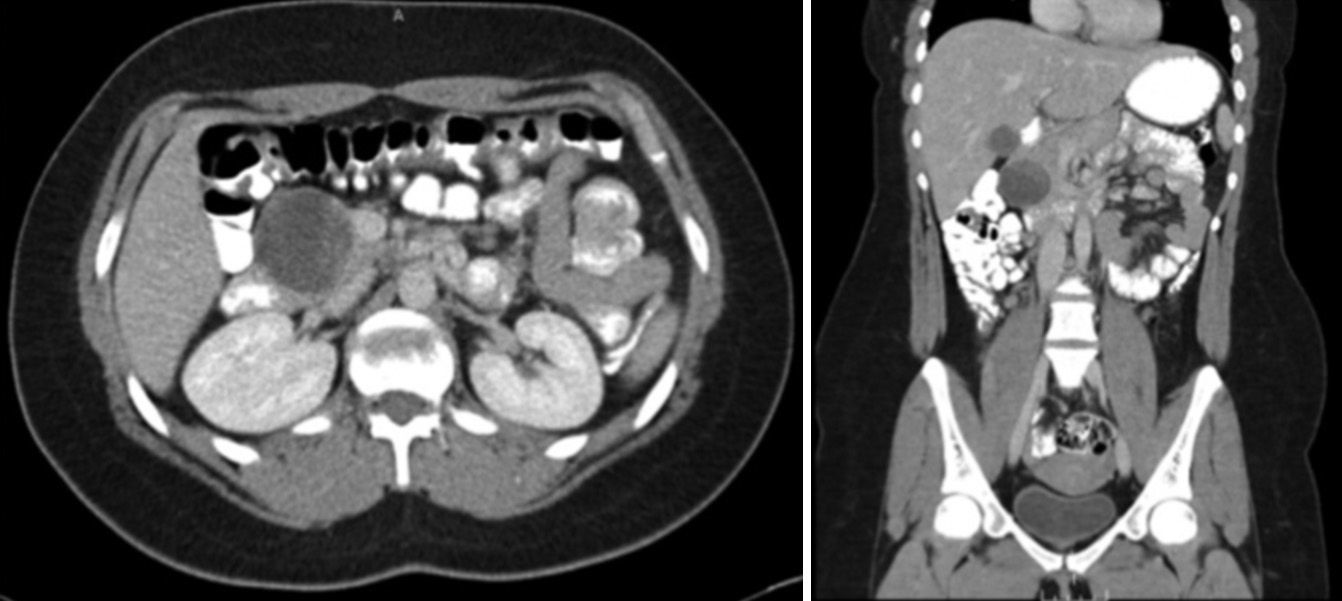
We present the clinical case of a 23-year-old woman with no history of interest who consulted for abdominal pain in the right iliac fossa. Physical examination as well as the basic work-up presented no alterations. Abdominal CT showed thickening that was inflammatory in appearance in the terminal ileum and a 4-cm mass with well-defined margins and a cystic appearance in the head of the pancreas (Fig. 1). The study was completed with a colonoscopy, that was normal, and an endoscopic ultrasound with needle aspiration of the pancreatic lesion. The result of the cytology was not conclusive and the suctioned liquid contained a concentration of carcinoembryonic antigen of less than 2ng/ml.
With the clinical and radiological suspicion of a pancreatic SPT, the neoplasm was resected by means of pancreaticoduodenectomy with resection of the pylorus (Fig. 2), followed by a Child's reconstruction. The postoperative period transpired without complications.
The pathology report corroborated the diagnosis of pancreatic SPT, with the characteristic solid and cystic components and areas of intratumoral hemorrhage. All the resection margins were free, although foci were found of perineural invasion, but not vascular. In the surgical specimen, 11 lymph nodes were isolated, none of which showed evidence of malignancy. The immunohistochemistry study was positive for alpha-1 antitrypsin, beta-catenin, vimentin and CD56, as well as weakly and focally positive for synaptophysin. These findings also favored the diagnosis of pancreatic SPT.
The most important retrospective SPT series was published by Papavramidis,5 who reviewed 718 cases reported in the English literature in 210 articles published by American, European and Japanese groups between 1933 and 2003. All the series reported the predominance of females, with a male:female ratio of 1:9.78. Mean age at presentation was 21.97 (range 2–85) and the mean tumor size was 6.08cm (0.5–34.5cm). Around half of the cases presented abdominal pain, one-third of them due to the sensation of the abdominal mass, and 15% were asymptomatic. The most frequently reported location was the tail of the pancreas, followed by the head and body of the pancreas.
The existence or absence of metastasis or invasion was described in 497 patients, 19.92% of whom presented metastasis or local invasion. The usual location of distant disease was the liver. Data about the surgical procedure was available for 553 patients and showed that only 2.53% required a palliative procedure, while in 3.07% no therapeutic procedure was performed. The remaining patients underwent surgical resection. The overall survival rates were 95.5% at 5 years and 93.4% at 10 years.5
SPT of the pancreas is a rare neoplastic disease that is well characterized by its epidemiologic, imaging and histologic peculiarities and by its biological behavior. The typical radiological appearance consists of a cystic tumor with a solid component or wall nodules.4,6 Macroscopically, it is a solid neoplasm with degenerative, hemorrhagic or necrotic cystic areas. Histologically, what is typical is the configuration in cell cords along a fibrovascular axis, composing pseudopapillae. Although the cellular origin is unknown, immunohistochemistry studies and those with cell markers probably mean that they are derived from a pluripotent precursor as they share similarities with duct and acinar as well as endocrine cells.4
In spite of its well-defined radiological characteristics and a relatively indolent biological behavior in most cases, the finding on imaging tests of a lesion that is cystic in nature with a solid component should direct the therapeutic algorithm toward intensive management and, therefore, toward radical surgical excision.6 Even in those cases with evidence of vascular invasion of the portal vein or the superior mesenteric artery or with metastatic dissemination, SPT should not be considered unresectable, as the survival rates continue to be very high.7 It has not been demonstrated that extensive lymphadenectomy is required.8 The use of chemo and radiotherapy in certain patients who are not considered candidates for surgery has also been described.9 Intra-arterial embolization can also be of use in selected cases.10
Please cite this article as: de Gregorio Muñiz L, Moss AK, Farhangmehr Setayeshi N, Colás Vicente A, Fernández-del Castillo C. Mujer joven con tumoración quística en la cabeza pancreática. Cir Esp. 2014;92:565–567.