Observation is the gold standard for stable patients with stab wounds. The aim of the study was to analyze the value of the primary review and complementary examinations to predict the need for surgery in stab wound patients in order to decrease observation times.
MethodsA retrospective study of stab wound patients recorded in a database. Clinical and diagnostic workup parameters were analyzed. The main variable was the need for surgery.
ResultsA total of 198 patients were included between 2006 and 2009, with a mean injury severity score (ISS) of 7.8±7, and 0.5% mortality. More than half (52%) of the patients suffered multiple wounds. Wound distribution was 23% neck, 46% thorax and 31% abdomen. Surgery was required in 73 (37%) patients (59% immediate, 27% delayed and 14% delayed). The need for surgery was associated with a lower revised trauma score (RTS), evisceration, active bleeding, and fascial penetration. Initial and control hemoglobin levels were significantly lower in patients who required surgery. A positive computerized tomography (CT) scan was associated with surgery. There were complications in 18% of patients, and they were more frequent in those who underwent surgery. There was no difference in complication rates between immediate and delayed (P=.72). Surgery was finally required in 10% of the patients with no abnormalities in the primary review and diagnostic workup, and 6% of those developed complications.
ConclusionNone of the parameters studied could individually assess the need for surgery. Primary and secondary reviews were the most important diagnostic tool, but CT scan should be used more often. An observation period of 24h is recommended in torso penetrating wounds.
La observación es el patrón oro del tratamiento de heridas de arma blanca en pacientes estables. El objetivo del estudio fue analizar el valor de la exploración física inicial y de las exploraciones complementarias ante la necesidad de cirugía, para disminuir tiempos de observación.
Material y métodosEstudio retrospectivo de un registro prospectivo de pacientes politraumáticos, seleccionando heridas de arma blanca troncales. Se analizan parámetros clínicos y diagnósticos. La variable principal es la necesidad de cirugía.
ResultadosEntre 2006 y 2009 se incluyó a 198 pacientes, con injury severity score medio de 7,8±7 y mortalidad del 0,5%. El 52% sufrieron heridas múltiples que se distribuyeron en cervicales 23%, torácicas 46% y abdominales 31%. Precisaron intervención quirúrgica 73 pacientes (37%), siendo el 59% inmediata, 27% precoz y 14% tardía. La necesidad de intervención se asoció a un menor revised trauma score, evisceración, hemorragia activa o constatación de herida penetrante. Las hemoglobinas iniciales, a las 2 y 12 h fueron significativamente inferiores en pacientes quirúrgicos. La tomografía computarizada (TC) positiva se asoció a intervención. Un 18% de pacientes presentaron complicaciones, concentradas en los pacientes quirúrgicos. Las intervenciones tardías no presentaron más complicaciones que las inmediatas (p=0,72). El 10% de los pacientes con exploración física y complementarias normales precisaron cirugía y el 6% desarrollaron complicaciones.
ConclusiónNingún parámetro fisiológico o analítico guía de forma individual la necesidad de intervención. La exploración física seriada es la maniobra diagnóstica más importante para decidir intervención, pero la TC puede usarse de forma liberal. Una observación de 24 h es recomendable en pacientes con heridas penetrantes.
Observation is the gold standard treatment for stab wounds in hemodynamically stable patients. This is supported by the high percentage of unnecessary surgical interventions and morbidity demonstrated in different series from the 1990s.1,2 There is no consensus on the ideal diagnostic-therapeutic approach or the safest minimum time for patient monitoring.
Since 2006, our hospital has applied the Advance Trauma Life Support standards of the American College of Surgeons3 for the resuscitation of patients with potentially penetrating trauma, as well as specific diagnostic–therapeutic algorithms depending on the wound location.
The aim of this study is to determine the value of the initial physical examination (IPE) and the complementary examinations (CE) that were added to the primary review or after the secondary review to predict surgical intervention or complications in patients with stab wounds to the torso.
Materials and MethodsBetween January 2006 and December 2009, 1075 trauma patients were included in a prospective registry. For the study, we selected stab wound patients with cervical, thoracic and abdominal injuries, while excluding wounds to the extremities.
Continuous and categorical variables were studied, including demographic variables (sex and age), hospitalization data (date and time and trauma team actions), number and location of the wounds (differentiating superficial anatomy from the cervical areas4 and the thoracoabdominal region), associated injuries, history of substance abuse and comorbidities. The primary review variables (blood pressure, heart and respiratory rates, temperature, Glasgow Coma Scale and Revised Trauma Score (RTS), respiratory auscultation, abdominal examination and pulses, local inspection data of the wounds including active bleeding, expanding hematoma, subcutaneous emphysema, penetration or evisceration) and the results of CE performed during admittance (initial and serial blood counts and biochemistry, blood gas analysis, x-ray, ultrasound and computed tomography [CT]) were studied individually and grouped into 22 categorical variables (positive physical examination and positive CE). We also analyzed the Injury Severity Score (ISS), the data of the surgical procedure such as the type or timing of the indication, defined as either immediate, early (within 6h) or delayed (after 6h), and the subsequent complications of the patients.
Continuous variables are expressed as mean±standard deviation. A univariate analysis was carried out. For the statistical study of the different variables, the X2 and Student's t-tests were used. The statistical analysis was done with SPSS version 16 software (SPSS Inc., Chicago, USA).
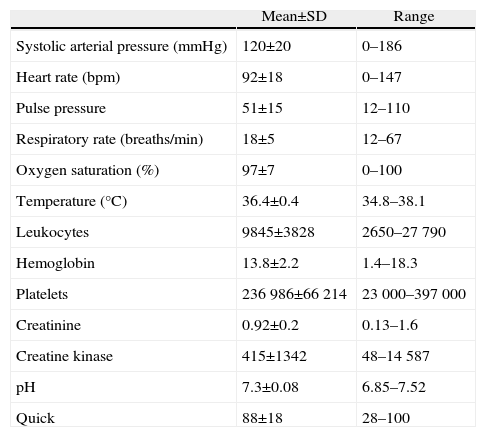
ResultsDuring the 4 years studied, 198 (18.4%) of 1075 trauma patients presented stab wounds to the torso. Most were male (178, 90%) with a mean age of 31±11. A total of 102 (52%) patients had more than one wound (range 1–14) with an average of 2 lesions per patient. In 189 patients (95.5%), the wounds were the result of assaults, in 7 (3.5%) from suicide attempts, and in 2 (1%) from accidents. Ninety-four (47.5%) patients were inebriated. The patients’ vital signs upon admission are expressed in Table 1. The average RTS of the patients was 11.8±0.4.
Vitals and Mean Work-up Values of Patients Upon Admittance.
| Mean±SD | Range | |
| Systolic arterial pressure (mmHg) | 120±20 | 0–186 |
| Heart rate (bpm) | 92±18 | 0–147 |
| Pulse pressure | 51±15 | 12–110 |
| Respiratory rate (breaths/min) | 18±5 | 12–67 |
| Oxygen saturation (%) | 97±7 | 0–100 |
| Temperature (°C) | 36.4±0.4 | 34.8–38.1 |
| Leukocytes | 9845±3828 | 2650–27790 |
| Hemoglobin | 13.8±2.2 | 1.4–18.3 |
| Platelets | 236986±66214 | 23000–397000 |
| Creatinine | 0.92±0.2 | 0.13–1.6 |
| Creatine kinase | 415±1342 | 48–14587 |
| pH | 7.3±0.08 | 6.85–7.52 |
| Quick | 88±18 | 28–100 |
The distribution of the 251 stab wounds was 60 (23%) cervical, 114 (46%) thoracic and 77 (31%) abdominal. Most cervical injuries were located in zone ii (31; 51%), most chest injuries were in the left anterior hemithorax (48; 42%) and most abdominal injuries were in the left upper quadrant (33; 43%). A total of 81 injuries (31%) were located in the thoracoabdominal region (mostly left thoracic).
Mean ISS of the series was 7.8±7, while in 32 (16%) patients it was higher than 15. Ten patients (5%) required blood transfusions. Mortality was 0.5% (one patient who came to the ER was asystolic after precordial stab wound) and 37 (18.6%) patients had complications.
Physical Examination and Complementary TestsThe most common findings in the IPE varied according to the location of the wounds. Thus, cervical wound findings were penetration through the platysma (37; 61%), active bleeding (20; 30%), hematoma (12; 20%) and subcutaneous emphysema (11; 18%). Chest wound findings included hypophonesis (42; 37%), and in the abdomen penetration of the peritoneum was seen (40; 52%). In the latter, we observed evisceration in 8 (10%) cases; abdominal palpation was initially normal in 52 (67%) cases, showed peritonitis in 21 (27%) and distension in 4 (5%).
In addition to the primary review, blood tests were always ordered (Table 1) and 173 (87%) patients had chest radiography, of which only 43 (25%) were considered pathological. During observation, CT was performed in 137 (69%) patients, with pathological findings observed in 96 (70%) cases. Eighteen (9%) patients underwent Focused Abdominal Sonography for Trauma (EcoFAST), which was positive in only 3 (17%) patients. No peritoneal lavage was performed.
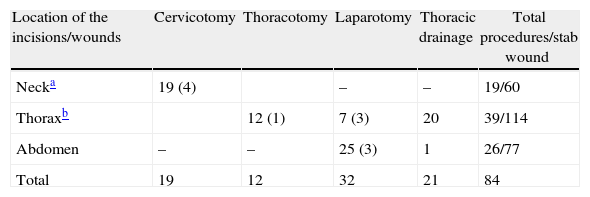
Surgical InterventionsSeventy-three (37%) patients underwent surgery and 84 procedures were performed, 21 of which were chest drains and considered minor interventions (not included in the analysis). The remaining 63 interventions were exploratory cervicotomies, thoracotomies and laparotomies (one lumbotomy and one laparoscopy), including: vascular sutures or ligatures; pharyngeal, pulmonary, cardiac sutures; gastrorrhaphy; primary repair of the small bowel; colorrhaphy; hepatic, renal, gallbladder, diaphragm primary repair or intestinal resections. Eleven (17%) were simple wall repairs, considered non-therapeutic or negative interventions (Table 2).
Surgical Procedures Performed According to Wound Location.
| Location of the incisions/wounds | Cervicotomy | Thoracotomy | Laparotomy | Thoracic drainage | Total procedures/stab wound |
| Necka | 19 (4) | – | – | 19/60 | |
| Thoraxb | 12 (1) | 7 (3) | 20 | 39/114 | |
| Abdomen | – | – | 25 (3) | 1 | 26/77 |
| Total | 19 | 12 | 32 | 21 | 84 |
In parentheses, simple wall repairs.
In 37 (59%) cases, surgery was immediate, in 17 (27%) early and in 9 (14%) deferred. Only 2 (1.2%) patients were operated on after 24h. One was a 52-year-old male with 2 previous abdominal stab wounds, normal physical examination and work-up, whose CT showed a hematoma on the greater curvature of the stomach. He was admitted for observation, and on the 4th day gastrorrhaphy was performed due to gastric perforation. The second patient was a 19-year-old female with multiple thoracoabdominal stab wounds and injuries to the extremities. She was diagnosed by CT with grade iii right renal laceration and, due to progressive anemia, a hemostatic renal suture was performed. Both patients were discharged without complications.
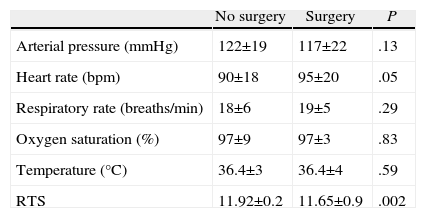
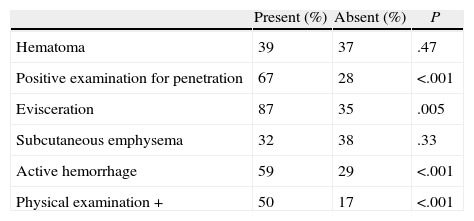
The patients who underwent surgery were slightly more tachycardic and had lower RTS values upon admission (Table 3). The presence of multiple injuries did not entail a significantly greater likelihood of surgical treatment (38% vs 35%, P=.77). The findings of penetration (P<.001), evisceration (P=.005) or active bleeding (P<.001) were significantly associated with surgery. The presence of a finding in the IPE was associated with a 50% need for intervention, but a negative IPE did not exclude it (Table 4). When analyzing the IPE of patients with abdominal wounds, up to 17 (32%) patients with normal-appearing abdomens required surgery.
Mean Vitals in Patients Who Underwent Surgery vs Those Who Did Not.
| No surgery | Surgery | P | |
| Arterial pressure (mmHg) | 122±19 | 117±22 | .13 |
| Heart rate (bpm) | 90±18 | 95±20 | .05 |
| Respiratory rate (breaths/min) | 18±6 | 19±5 | .29 |
| Oxygen saturation (%) | 97±9 | 97±3 | .83 |
| Temperature (°C) | 36.4±3 | 36.4±4 | .59 |
| RTS | 11.92±0.2 | 11.65±0.9 | .002 |
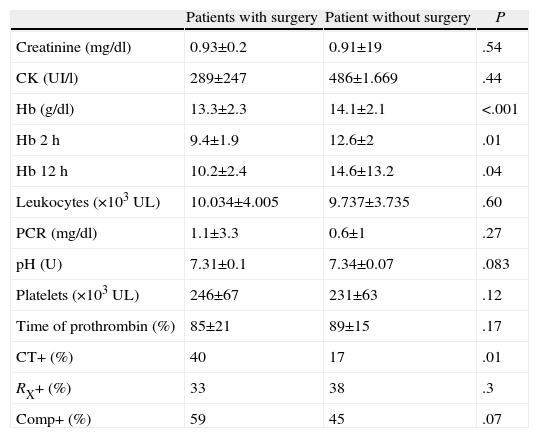
By comparing observed versus surgical patients with regards to CE, there were significant differences observed in mean hemoglobin values, both initially as well as in subsequent tests. The differences between the two groups allowed for weighing clinical significance, which was 0.8g/dl at admission, 3.2g/dl after 2h and 4.4g/dl after 12h. There were no significant differences in the analytical values of other parameters (Table 5). CT was the imaging test with the greatest prognostic value for intervention, although it was only positive in 84% of the patients who underwent surgery in whom CT has been ordered. Positive CE implied greater need for intervention, but not significantly. Up to 45% of patients with conservative treatment showed some pathologic data in CE. About 10% of patients with normal IPE and CE required surgery.
Mean Work-up Values and Percentages of Positive Examinations in Patients With or Without Surgery.
| Patients with surgery | Patient without surgery | P | |
| Creatinine (mg/dl) | 0.93±0.2 | 0.91±19 | .54 |
| CK (UI/l) | 289±247 | 486±1.669 | .44 |
| Hb (g/dl) | 13.3±2.3 | 14.1±2.1 | <.001 |
| Hb 2h | 9.4±1.9 | 12.6±2 | .01 |
| Hb 12h | 10.2±2.4 | 14.6±13.2 | .04 |
| Leukocytes (×103UL) | 10.034±4.005 | 9.737±3.735 | .60 |
| PCR (mg/dl) | 1.1±3.3 | 0.6±1 | .27 |
| pH (U) | 7.31±0.1 | 7.34±0.07 | .083 |
| Platelets (×103UL) | 246±67 | 231±63 | .12 |
| Time of prothrombin (%) | 85±21 | 89±15 | .17 |
| CT+ (%) | 40 | 17 | .01 |
| RX+ (%) | 33 | 38 | .3 |
| Comp+ (%) | 59 | 45 | .07 |
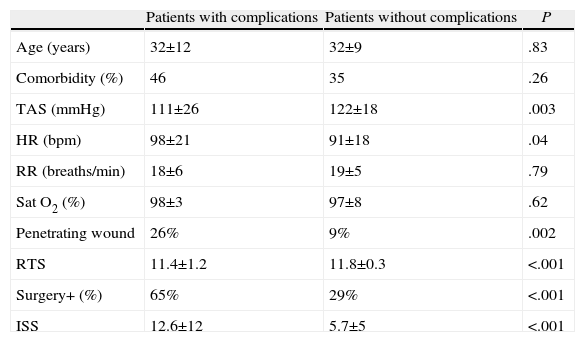
Thirty-seven (18%) patients had complications. The most frequent complications were local (wound infection, hyperalgesia or rebleeding). The most common systemic complications were withdrawal symptoms and pneumonia. The presence of complications was associated with penetrating wounds (26% vs 9%, P=.002). Patients with complications had poorer systolic arterial pressure (P=.003) and more tachycardia (P=.04). There were no differences in the analytical results between patients with complications or those with correct clinical course (Table 6). About 6% of patients with normal CE and IPE presented complications. Complications were concentrated in the surgical patients (65% vs 29%, P<.001). The time of surgery was not significantly associated with a higher incidence of complications; thus, immediate surgery presented a 34% rate of complications compared to 30% of early surgeries and 43% of late surgeries (P=.72).
Patient Characteristics According to the Appearance of Complications.
| Patients with complications | Patients without complications | P | |
| Age (years) | 32±12 | 32±9 | .83 |
| Comorbidity (%) | 46 | 35 | .26 |
| TAS (mmHg) | 111±26 | 122±18 | .003 |
| HR (bpm) | 98±21 | 91±18 | .04 |
| RR (breaths/min) | 18±6 | 19±5 | .79 |
| Sat O2 (%) | 98±3 | 97±8 | .62 |
| Penetrating wound | 26% | 9% | .002 |
| RTS | 11.4±1.2 | 11.8±0.3 | <.001 |
| Surgery+ (%) | 65% | 29% | <.001 |
| ISS | 12.6±12 | 5.7±5 | <.001 |
Stab wounds are usually low-energy, potentially penetrating, injuries. Mortality reports in the literature, however, range from 0% to 40% depending on the series and the location of the wounds.5,6 In the past 25 years, the approach of hemodynamically stable patients with penetrating injuries has changed from mandatory surgical exploration to conservative treatment with serial physical examination and no local wound exploration or minimally invasive techniques. The diagnostic and therapeutic management of stab wounds to the torso varies greatly in different centers.7–9 There is also no consensus on safe, necessary observation times, although most authors place them between 12 and 24h.10–12
In our hospital, the protocol for these injuries includes primary and secondary patient review. Subsequent decisions are conditioned by hemodynamic stability and wound location. In cervical injuries, the presence of “severe signs” during examination (active bleeding that does not yield with compression, expanding hematoma, absence of radial pulse, haematemesis or obvious esophageal trauma, air leak or increasing subcutaneous emphysema, dyspnea or stroke)13 are indications for urgent surgery. In chest wounds, chest tubes are used liberally in suspected hemopneumothorax. Surgery is indicated according to the drainage volume (initially 1500ml>200ml/h in the following 4h) and by the presence of significant persistent air leak or certain cardiac, esophageal or diaphragm lesions.5 In abdominal wounds, peritonitis and the inability to assess the abdomen are indications for immediate surgery.7 As a general rule, in stab wound patients we consider 24h a safe period of observation.14,15
Some physiological parameters have been described as predictors of outcome in specific types of penetrating trauma to the torso.16 Not surprisingly, patients requiring intervention or presenting complications were more tachycardic or had lower RTS values, but our data do not allow us to establish a cutoff to discern the need for surgery or probability of complications.
The local examination of the wound as a secondary review maneuver is no longer performed because penetrating wounds are no longer considered an indication for surgery per se. In 1987, Demetriades et al. demonstrated in a prospective study of 476 patients with stab wounds in the anterior abdomen and confirmed penetration of the peritoneum that up to 27% did not present significant injuries.7 For some authors, it is useful in negative cases in order to decide upon immediate patient discharge.10,17 In our series, the high incidence of interventions in patients with confirmed penetration was due to the fact that, in cervical wounds, the violation of the platysma is an indication for exploratory cervicotomy in many cases, in accordance with the application of a policy used in hospitals with a low incidence of these injuries.18 In 5 cases of abdominal wounds, the confirmation of penetration per se motivated the surgery (2 negative laparotomies). Currently, we adhere to the idea of not locally exploring the wounds, especially given the little information this provides versus the possible disadvantages (pain, hemorrhage, and wound infection).
Likewise, evisceration is also not an absolute criterion for surgery, although some protocols do include it as an indication for laparotomy and associate it with a rate of visceral injury of 80%.6,19 Benissa et al. reported a retrospective series of 75 patients with abdominal stab wounds, and the group that based the indication for surgery on evisceration presented 78% unnecessary laparotomies.20 In our series, 7 out of the 8 cases with evisceration underwent surgery. In 3 patients with evisceration of bowel loops through the wall defect, surgery was immediate to repair the abdominal wall, but laparotomy was negative. The 4 patients who presented evisceration of the mesentery were surgically treated early on after CT scans showed positive findings (3 injuries to hollow viscus and one mesenteric vascular repair).
Careful physical examination and serial monitoring by the surgeon are safe even in inebriated patients, but adding CT to diagnostic algorithms increases confidence in the selection of conservative treatment.21 In our series, the IPE seems to have more value than CE for deciding on surgery. However, a normal physical examination does not exclude the existence of injuries requiring surgery, which implies that the physical examination may have been incorrectly done or that it its sensitivity is not 100%.10,11
Early identification of patients with internal bleeding or visceral injury is essential for conservative treatment, and serial laboratory tests seem to be useful in intensive monitoring protocols. Low hemoglobin values or decreasing levels in serial tests have been widely used as indicators of the need for surgery.21,22 Leukocytosis is a nonspecific finding for diagnosing the presence of visceral injury even in serial determinations.23
The value of chest radiography as an addition to the primary review in penetrating injuries is, in our experience, limited. In unstable patients with clinical suspicion of hemopneumothorax, radiography is able to verify the correct placement of a drain. In stable patients with cervical injuries in zone i or the thoracoabdominal region, radiography can help detect pneumothorax that was not noticed during auscultation. In addition, its sensitivity and negative predictive value for diaphragm injuries are very low.24
Peritoneal lavage is an invasive procedure indicated in unstable patients that has been associated with a high percentage of non-therapeutic laparotomies.25 There is no threshold for positivity of erythrocytes or leukocytes with 100% sensitivity for injury, nor do amylase or alkaline phosphatase determinations provide any benefit as their results take too long.26 EcoFAST is a fast test for detecting fluid and, although its negativity does not imply the absence of injury,15 if it is positive it provides the same information as lavage, with no added morbidity.27
Our results confirm the value of CT in the management of stable patients with stab wounds to the torso. In 2001, Chiu et al. presented a series of 75 consecutive patients with penetrating thoracoabdominal injuries and hemodynamic stability who underwent triple-contrast CT with a sensitivity of 94%, specificity of 95% and positive predictive value for surgery of 95%.28 CT scans can assess wound penetration or facilitate the conservative treatment of penetrating liver trauma by ruling out active hemorrhaging. Its value to exclude diaphragmatic injury or hollow viscus injury is somewhat lower.29,30
In our series, 86% of the surgeries were performed within the first 6h of observation. In the non-immediate interventions, the indication was based on changes in the clinical evolution of the patients, with diagnostic intention in the case of laparoscopy to rule out diaphragmatic injury. Since the deferred surgeries did not present a higher rate of complications and only 2 cases required surgery beyond the first 24h, we support the idea of maintaining a safe 24h observation period.
Our study presents several limitations related with its retrospective nature, the heterogeneity of the lesions and the possibility of incompliance or changes in the protocols used during the study period. The establishment of shorter observation times while maintaining safety will depend on the degree of compliance with these protocols.
ConclusionsConservative treatment with observation and serial testing of initially stable patients with stab wounds is safe. No single physiological or analytical parameter on its own can determine the need for surgery.
Serial physical examination is the most important diagnostic maneuver for determining surgical intervention in these patients, and CT is the CE with the best performance.
Since normal IPE and CE do not exclude the need for surgery, we recommend the use of surgical decision protocols and the observation of these patients during a period of no less than 24h.
Conflict of InterestsThe authors have no conflict of interests to declare.
Please cite this article as: Martínez Casas I, Sancho Insenser J, Climent Agustín M, Membrilla Fernández E, Pons Fragero MJ, Guzmán Ahumada J, et al. Estudio del valor predictivo de la revisión primaria y de las exploraciones complementarias para anticipar la necesidad de intervención quirúrgica en pacientes con heridas de arma blanca en el torso. Cir Esp. 2013;91:450–456.