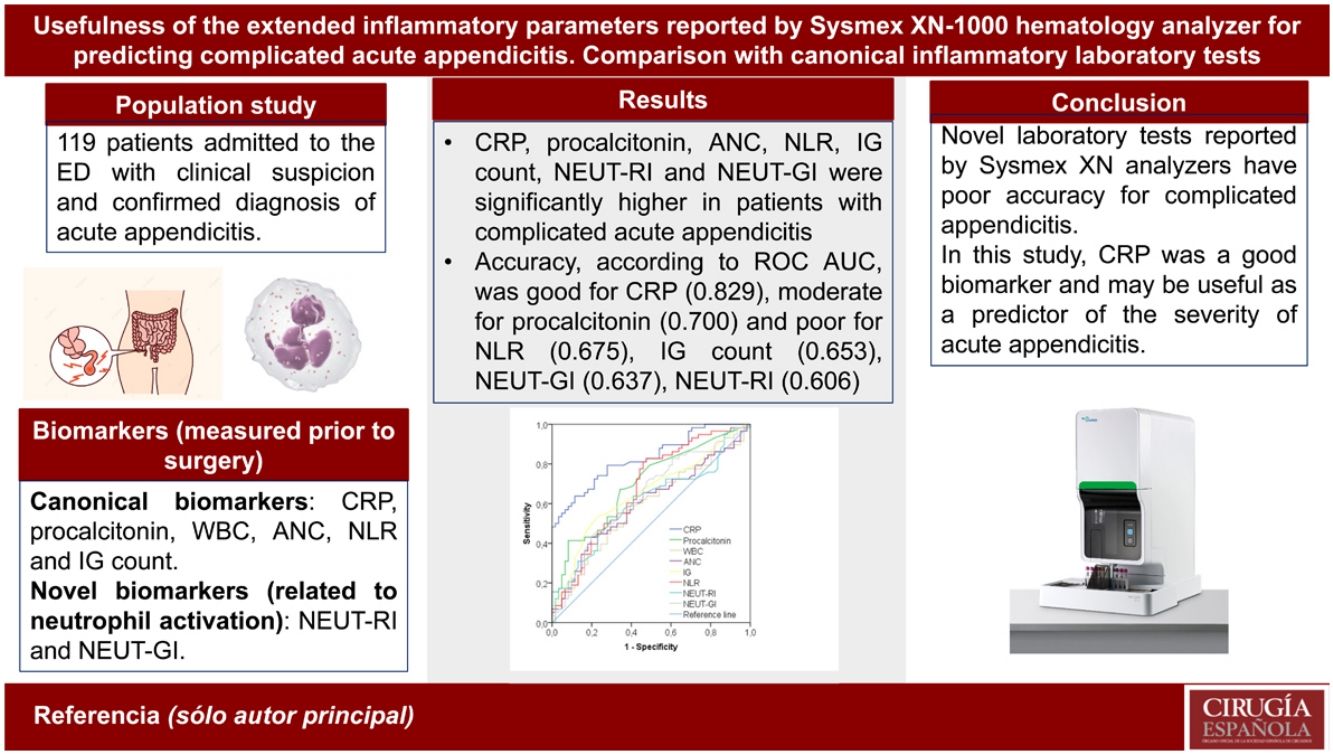
Accurate diagnosis of complicated appendicitis is of importance to ensure that patients receive early and effective treatment, minimizing the risk of postoperative complications to promote successful recovery. Biochemical markers are a promising tool to identify complicated appendicitis. We aimed to evaluate the potential role of novel parameters related with neutrophil activation, known as “Extended Inflammation Parameters” (EIP), included in blood cell count reported by Sysmex XN-Series analyzers, compared to other canonical biomarkers in identifying complicated appendicitis.
MethodProspective observational study including patients with confirmed diagnosis of acute appendicitis. C-reactive protein (CRP), procalcitonin, cell blood count, including white blood cell (WBC), absolute neutrophil (ANC) and immature granulocyte (IG) count and EIP (neutrophil reactivity [NEUT-RI] and granularity intensity [NEUT-GI]) were analyzed before surgery. Their accuracy to diagnose complicated appendicitis was tested in an ROC curve analysis.
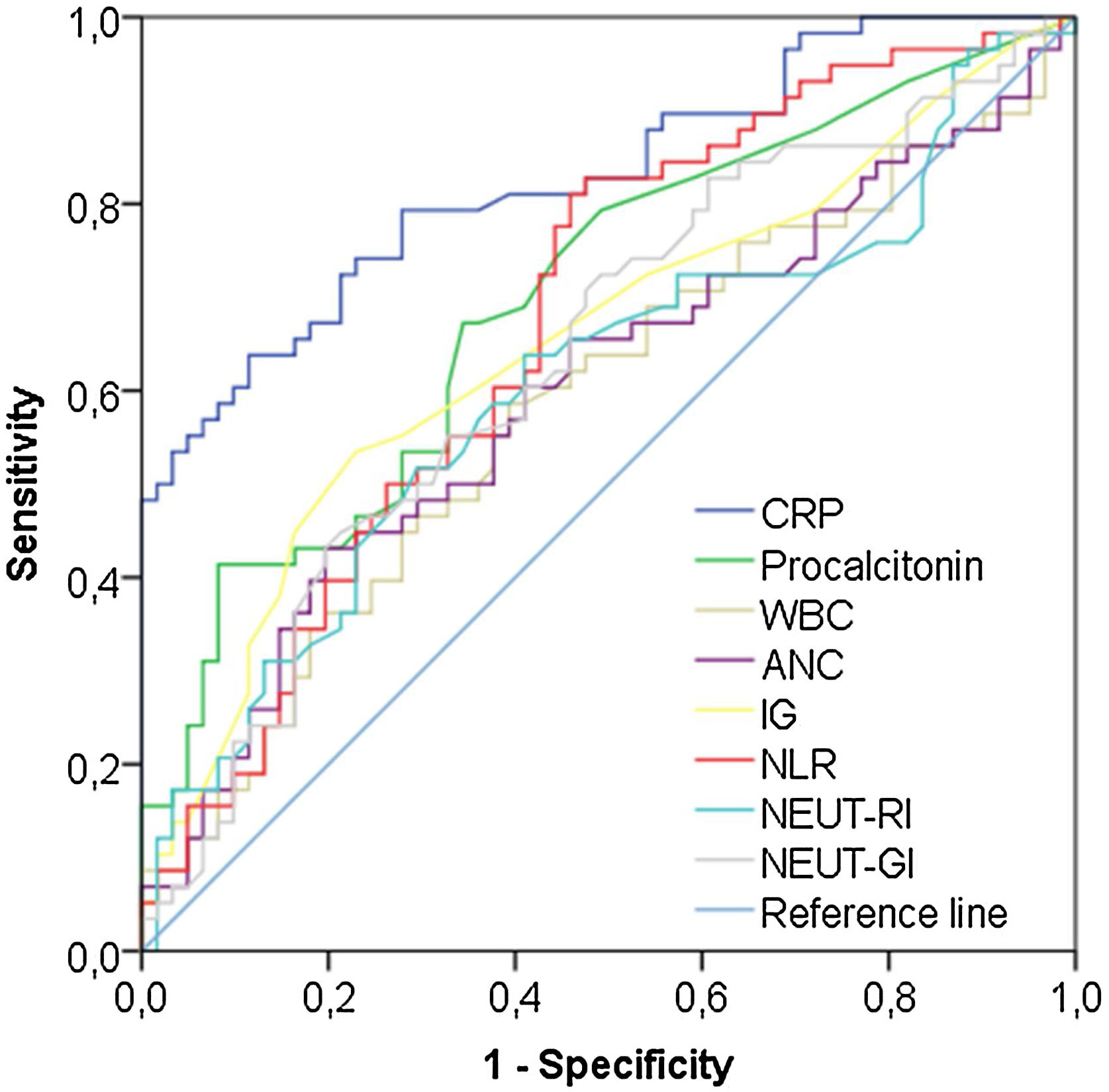
ResultsOur population study included 119 patients, and appendicitis was complicated in 58 (48.7%). NLR, CRP and procalcitonin levels, ANC and IG count and NEUT-RI and NEUT-GI were higher in patients with complicated appendicitis. Regarding accuracy for complicated appendicitis, CRP was the biomarker with the highest performance (ROC AUC: 0.829), with an optimal cutoff of 73.1 mg/L (sensitivity: 63.8%, specificity: 88.5%). NEUT-RI and NEUT-GI achieved both significant but poor accuracy, with ROC AUC of 0.606 and 0.637, respectively.
ConclusionsNovel laboratory tests reported by Sysmex XN-Series analyzers have poor accuracy for identifying complicated appendicitis. In this study, CRP was the biomarker with the highest performance and may be useful as predictor of the severity of acute appendicitis.
El diagnóstico de la apendicitis complicada es esencial para garantizar el tratamiento precoz y eficaz del paciente, minimizando el riesgo de complicaciones postquirúrgicas. Los biomarcadores son una herramienta prometedora para la identificación de esta condición. En este estudio evaluamos los nuevos parámetros (“Perfil Inflamatorio Extendido” [PIE]) incluidos en el hemograma de los analizadores Sysmex de la Serie XN, en comparación con marcadores tradicionales, para identificar la apendicitis complicada.
MétodoEstudio prospectivo observacional incluyendo pacientes con diagnóstico confirmado de apendicitis aguda. Previo a la cirugía se midieron proteína C reactiva (PCR), procalcitonina, recuento celular en sangre (recuento de leucocitos, recuento absoluto de neutrófilos [RAN] y granulocitos inmaduros [GI]) y PIE (intensidad de la reactividad (NEUT-RI) y de la granularidad (NEUT-GI) de neutrófilos). Su rendimiento se analizó mediante análisis de curvas ROC.
ResultadosLa población incluyó 119 pacientes y la apendicitis fue clasificada como complicada en 58 (48,7%). El cociente neutrófilos/linfocitos, las concentraciones de PCR y procalcitonina, el RAN y de GI y NEUT-RI y NEUT-GI fueron más altos en pacientes con apendicitis complicada. La PCR fue el biomarcador con mayor rendimiento (AUC ROC: 0.829), con un punto de corte óptimo de 73,1 mg/L (sensibilidad: 63,8%, especificidad: 88,5%). El rendimiento de NEUT-RI y NEUT-GI fue pobre, con AUC ROC de 0,606 y 0,637, respectivamente.
ConclusionesLos nuevas medidas de laboratorio de los analizadores Sysmex de la Serie XN tienen un pobre rendimiento para identificar la apendicitis complicada. En este estudio, la PCR fue el biomarcador con el mayor rendimiento y puede ser útil como predictor de la gravedad de la apendicitis aguda.
Acute appendicitis is one of the most common general surgical emergencies worldwide.1 Patients with suspected acute appendicitis are evaluated with several diagnostic tools, such as clinical examination, scoring systems, biochemical testing and imaging modalities. Although appendectomy has long been considered the standard of care for acute appendicitis, conservative management with antibiotics has been reported as a safe strategy for non-complicated appendicitis.2,3 Therefore, the differential diagnosis between both conditions is a challenge for clinicians, and there is a need for novel early predictors of the severity of acute appendicitis that would enable us to provide optimal treatment for each patient. Biochemical markers are a promising, reliable diagnostic tool to identify negative cases as well as complicated acute appendicitis.4
Because acute appendicitis is a local inflammatory process in the early stage, inflammatory-related biomarkers, such as white blood cell (WBC) and absolute neutrophil counts (ANC), C-reactive protein (CRP), procalcitonin, interleukin-6, fibrinogen, immature granulocyte (IG) count or neutrophil-lymphocyte ratio (NLR) have been evaluated as predictors of complicated acute appendicitis, with controversial results.5–11
Advances in blood count technology bring novel parameters and provide deeper insights into the blood cells than cell count alone. Sysmex XN-Series analyzers offer additional parameters, known as “Extended Inflammation Parameters” (EIP), which make it possible to quantitatively assess IG and the activation status of neutrophils during inflammation. These analyzers use flow cytometry fluorescence technology to obtain data about cell membrane composition and cytoplasmic activity. Hence, parameters related to neutrophils, such as neutrophil reactivity (NEUT-RI) and granularity intensity (NEUT-GI), are indicative of the activation status of the neutrophilic granulocytes, and their measurement takes into account the metabolic activity of neutrophils, the internal structure, and cell size.12
In a previous study, we reported that, among EIP obtained through CBC analysis by the Sysmex-XN 1000 hematology analyzer, parameters associated with neutrophil activation are not useful for the early diagnosis of acute appendicitis.13 However, their value for predicting complicated acute appendicitis has not yet been evaluated. The inclusion of these novel laboratory tests as criteria for decision making in patients with acute appendicitis would be of interest because they are readily available from a routine complete blood count with differentials, at no additional cost.
In this study, we aimed to evaluate the potential role of these novel inflammatory parameters to identify complicated acute appendicitis, in comparison with CRP, WBC, ANC, IG count, NLR and procalcitonin, which could provide an assessment basis to decide between surgical or conservative treatment options.
MethodsStudy design and population studyThis was a single-center, prospective, observational study conducted from May 2021 to November 2022 that included adult and pediatric patients admitted to the Emergency Department with clinical suspicion of acute appendicitis requiring surgical treatment according to the attending surgeon’s judgment, followed by pathology results confirming the diagnosis of acute appendicitis. Patients who were pregnant, received previous antibiotics and/or immunosuppressive or steroid treatment or under conservative management, presented hematologic malignancy, or had missing data were excluded from the study. Patients were recruited through convenience sampling when the investigators participating in the study were present.
To evaluate the value of biomarkers for complicated acute appendicitis, we divided the patients into 2 groups according to histopathological findings described in the specimen after surgery: (a) non-complicated group (phlegmonous or catarrhal); and (b) complicated group (perforated and/or gangrenous).
Blood sampling and laboratory methodsOn admission to the Emergency Department, initial management included venous blood sampling for routine laboratory workup, including CRP, procalcitonin and blood cell count with WBC, ANC and IG count.
Regarding laboratory assays, serum CRP levels were measured by an immunoturbidimetric assay in Cobas c702 analyzer (Roche Diagnostics, Switzerland), serum procalcitonin levels by a chemiluminescent enzyme immunoassay on G600II analyzer (Fujirebio Diagnostics Inc, Japan) and WBC, ANC and IG count by fluorescence flow cytometry, on Sysmex XN-1000 analyzer (Sysmex, Kobe, Japan), according to manufacturer recommendations. NLR was also calculated. Furthermore, for analysis, IG count and EIP associated with neutrophil activation, (NEUT-RI and NEUT-GI), were collected. These latter laboratory tests were not reported to attending physicians.
This study was approved by the local Ethics Committee and performed under a waiver of informed consent. The work was carried out in accordance with the guidelines of the Declaration of Helsinki of the World Medical Association. All data used in the study was retrieved from results obtained during routine laboratory diagnostics, without the need for additional blood collection or storage for later measurements.
Statistical analysisThe normality of continuous variables was analyzed by the Kolmogorov–Smirnov or Shapiro–Wilk tests, and they are reported as median (interquartile range [IQR]) or mean (standard deviation), as appropriate. Categorical variables are presented as frequency and percentage in each category. Mann–Whitney U and chi-squared or Fisher exact tests were used, as appropriate, to compare continuous and categorical data between groups, respectively.
To assess the discrimination ability for complicated acute appendicitis of circulating biomarkers, we estimated receiver operating characteristic (ROC) curves and area under the curves (AUC).14 Interpretation of AUC is as follows: 1.0 is a perfect discriminative biomarker, 0.9−0.99 is an excellent biomarker, 0.8−0.89 is a good biomarker, 0.7−0.79 is a fair biomarker, 0.51−0.69 is a poor biomarker, and ≤0.5 is of no value.15 We additionally determined the optimal cutoff value using Youden’s index,16 and sensitivity, specificity, positive likelihood ratio (LR) and negative LR were calculated. The Delong method was used for comparison of significant AUC.17
We performed analyses using the software packages SPSS 21.0 (SPSS Inc., IL, USA) and MedCalc 15.0 (MedCalc Software, Ostend, Belgium). In all tests, a 2-sided P-value of <.05 was considered statistically significant.
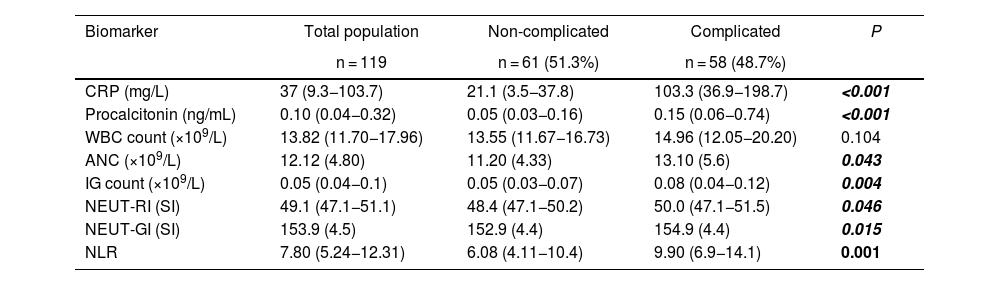
ResultsThis study included a total of 119 patients (median age: 28 years, interquartile range [IQR]: 15–47 years, range: 6–101 years; 75 [63%] male) with a confirmed diagnosis of acute appendicitis who underwent appendectomy. According to the histopathological findings, 58 (48.7%) patients were classified in the complicated group and 61 (51.3%) in the non-complicated group. Patients with complicated acute appendicitis were significantly older (median age: 40 years, IQR: 20–57) vs the non-complicated group (median age: 18 years, IQR: 13–35; P = .004). No differences were detected according to gender (P = .353).
Laboratory findings are listed in Table 1. Higher NLR, CRP and procalcitonin levels, ANC and IG count and NEUT-RI and NEUT-GI were found in patients with complicated acute appendicitis, with no significant difference between groups for WBC count.
Laboratory findings in both groups (non-complicated vs complicated acute appendicitis).
| Biomarker | Total population | Non-complicated | Complicated | P |
|---|---|---|---|---|
| n = 119 | n = 61 (51.3%) | n = 58 (48.7%) | ||
| CRP (mg/L) | 37 (9.3−103.7) | 21.1 (3.5−37.8) | 103.3 (36.9−198.7) | <0.001 |
| Procalcitonin (ng/mL) | 0.10 (0.04−0.32) | 0.05 (0.03−0.16) | 0.15 (0.06−0.74) | <0.001 |
| WBC count (×109/L) | 13.82 (11.70−17.96) | 13.55 (11.67−16.73) | 14.96 (12.05−20.20) | 0.104 |
| ANC (×109/L) | 12.12 (4.80) | 11.20 (4.33) | 13.10 (5.6) | 0.043 |
| IG count (×109/L) | 0.05 (0.04−0.1) | 0.05 (0.03−0.07) | 0.08 (0.04−0.12) | 0.004 |
| NEUT-RI (SI) | 49.1 (47.1−51.1) | 48.4 (47.1−50.2) | 50.0 (47.1−51.5) | 0.046 |
| NEUT-GI (SI) | 153.9 (4.5) | 152.9 (4.4) | 154.9 (4.4) | 0.015 |
| NLR | 7.80 (5.24−12.31) | 6.08 (4.11−10.4) | 9.90 (6.9−14.1) | 0.001 |
Values expressed as median (IQR) or mean (SD), as appropriate.
Itilicized values is to highlight that the p-value is significant (< 0,05).
Abbreviations: CRP: C-reactive protein; WBC: white blood cell; ANC: absolute neutrophil count; IG: immature granulocytes; NEUT-RI: neutrophil reactivity; NEUT-GI: granularity intensity; NLR: neutrophil-to-lymphocyte ratio.
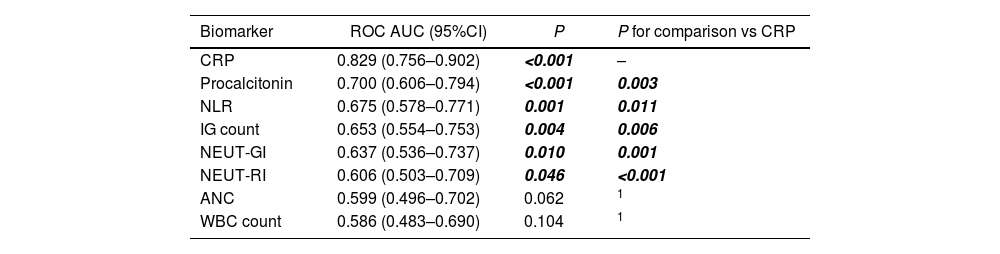
In the ROC analysis, a significant AUC was estimated for CRP and procalcitonin levels, NLR, ANC and IG count and NEUT-RI and NEUT-GI (Table 2 and Fig. 1). CRP was the biomarker with the highest accuracy for complicated acute appendicitis, with a significant difference compared to procalcitonin, NLR, ANC, IG count and both parameters related to neutrophil activation included in EIP. According to the Youden index, the optimal cutoff was 73.1 mg/L, achieving a sensitivity of 63.8% (95% CI: 50.1–76.0), specificity of 88.5% (95% CI: 77.8–95.3), positive LR of 5.6 (4.5–6.9) and negative LR of 0.4 (0.2−0.9). As criteria to rule out complicated acute appendicitis, a CRP cutoff of 7.7 mg/L (reference value in our laboratory: <5 mg/L) achieved a negative LR of 0.2.
ROC curves for complicated acute appendicitis.
| Biomarker | ROC AUC (95%CI) | P | P for comparison vs CRP |
|---|---|---|---|
| CRP | 0.829 (0.756–0.902) | <0.001 | – |
| Procalcitonin | 0.700 (0.606–0.794) | <0.001 | 0.003 |
| NLR | 0.675 (0.578–0.771) | 0.001 | 0.011 |
| IG count | 0.653 (0.554–0.753) | 0.004 | 0.006 |
| NEUT-GI | 0.637 (0.536–0.737) | 0.010 | 0.001 |
| NEUT-RI | 0.606 (0.503–0.709) | 0.046 | <0.001 |
| ANC | 0.599 (0.496–0.702) | 0.062 | 1 |
| WBC count | 0.586 (0.483–0.690) | 0.104 | 1 |
Itilicized values is to highlight that the p-value is significant (< 0,05).
Abbreviations: CI: confidence interval; CRP: C-reactive protein; WBC: white blood cell; ANC: absolute neutrophil count; IG: immature granulocytes; NEUT-RI: neutrophil reactivity; NEUT-GI: granularity intensity; NLR: neutrophil-to-lymphocyte ratio.
Acute appendicitis is the most frequent urgent abdominal surgery, and a delayed diagnosis may lead to disease complications, such as perforation and peritonitis, and more postoperative complications. Acute appendicitis occurs when the lumen of the vermiform appendix becomes inflamed, usually due to an obstruction. This obstruction can be caused by a fecalith (“fecal stone” or mass of feces), lymphoid hyperplasia (most commonly in children), a rare parasitic infection, or a tumor.18 Complicated appendicitis, which accounts for nearly 25% of cases requiring appendectomy, is the result of appendiceal rupture with subsequent abscess or phlegmon formation.18 Although complicated and non-complicated acute appendicitis share similar physical signs and symptoms, differences between both forms of acute appendicitis include mean time with symptoms (less than 24 h for uncomplicated appendicitis vs 48 h or more for complicated appendicitis) and other variables, such as age and gender.18 Because complicated and non-complicated acute appendicitis are associated with higher morbidity and mortality, it is a challenge for Emergency Department physicians and surgeons to reliably distinguish between them. Thus, there is a need to develop tools to potentially differentiate between these conditions in clinical practice to allow for stratified management in decisions.19
In recent decades, research has been carried out to identify circulating biomarkers in body fluids that could differentiate between non-complicated and complicated appendicitis. Biochemical markers have the potential to provide non-invasive objective criteria with no adverse effects for the patient. Conventional biomarkers like CRP, procalcitonin, WBC, ANC or NLR have been widely evaluated for diagnosis of acute appendicitis and to identify complicated disease. The role of emerging biomarkers related to ischemia or inflammation have also been evaluated for this purpose. For instance, ischemia-modified albumin has been reported as a novel and useful marker to distinguish gangrenous/perforated appendicitis from non-complicated appendicitis,20 although further prospectively designed and adequately powered studies are needed for this biomarker.21 Similarly, increased plasma calprotectin levels have been reported in patients with complicated acute appendicitis, improving the diagnostic accuracy of conventional biomarkers, such as CRP or WBC.22 Less known is the role of novel biomarkers like EIP that reflect neutrophil activation, functioning as a signature of the activation of immune system cells in the course of inflammation, which is a characteristic condition of acute appendicitis.1
The role of biomarkers for this purpose is controversial. Lietzén et al. concluded that laboratory markers like WBC and CRP are not reliable enough to accurately estimate the severity of acute appendicitis.23 Recently, a review including 65 laboratory tests concluded that no single biomarker can be used by clinicians to reliably differentiate between patients with complicated and non-complicated appendicitis.24 In our study, which evaluated canonical and novel parameters related with neutrophil activation reported by Sysmex analyzers, the main findings were: (1) although these novel tests showed statistically significant accuracy for complicated acute appendicitis, their discriminatory ability was poor15; and (2) CRP was the biomarker with the highest accuracy for complicated acute appendicitis (ROC AUC: 0.829), above other tested conventional inflammatory-related biomarkers, such as procalcitonin, IG count, NLR or ANC.
In a recent study by García-Amador et al.,5 CRP and neutrophil count, expressed as percentages, achieved ROC curves of 0.73 and 0.69, respectively; meanwhile, a predictive model combining both with other clinical and demographic variables showed an ROC AUC of 0.80, lower than CRP alone in our study, achieving an ROC AUC of 0.829. The optimal cutoff (73.1 mg/L) in our study was similar to the García-Amador et al. report (73.6 mg/L).5 In comparison with other studies, the ability of CRP to identify complicated appendicitis was very similar to the Güngör et al. article (ROC AUC: 0.82)25 but slightly lower than the Li et al. (ROC AUC: 0.902) study.7
In comparison with CRP, the value of procalcitonin for predicting complicated acute appendicitis has been less evaluated, and results are controversial. In the Li et al. study,7 this biomarker demonstrated very high accuracy, with an ROC AUC of 0.987, and its usefulness has been recently supported by meta-analyses reporting ROC AUC above 0.9.26,27 However, these results have not been confirmed in other recent studies; for example, Cakal et al. have reported the poor performance of procalcitonin (ROC AUC: 0.59) in differentiating complicated from non-complicated appendicitis.28 NLR has been also reported as a biomarker with a high performance for predicting complicated acute appendicitis.29 Finally, in acute complicated appendicitis, Turkes et al. reported an ROC AUC of 0.796 for IG count.10 In our study, the accuracies of procalcitonin (ROC AUC: 0.700), NLR (ROC AUC: 0.675) and IG count (ROC AUC: 0.653) were moderate and significantly lower than CRP.
Concerning novel inflammatory biomarkers reported by the Sysmex XN-Series analyzers, to our knowledge this is the first study testing their value for differentiating complicated and non-complicated appendicitis. Although significant differences were detected for NEUT-GI and NEUT-RI between both groups, the ability for diagnosis of complicated appendicitis was poor for both biomarkers (ROC AUC below 0.7, significantly lower than CRP), which would limit their use in clinical practice.
Our study presents certain limitations. First, it was a single-center observational study with a small sample size, and the results must be validated in a larger cohort. Second, no clinical scoring system (some including laboratory tests) was included for the comparison of tested biomarkers. However, recent studies do not support the routine use of established clinical scoring systems, such as the Alvarado score or Appendicitis Inflammatory Response (AIR) score, to distinguish between complicated vs non-complicated acute appendicitis.30 Furthermore, the use of these scores in real-life is scarce.31 A third limitation was that all patients included in this study had undergone appendectomy, and we did not analyze patients receiving conservative treatment.
In conclusion, our study suggests that novel laboratory parameters (EIP) reported by Sysmex XN-Series analyzers have poor accuracy for identifying complicated acute appendicitis. However, according to its discriminatory ability through ROC AUC, CRP is a good biomarker and may be useful as a predictor of the severity of acute appendicitis, and its inclusion in multivariate scoring systems would be beneficial to improve diagnostic performance and to provide a tool which is applicable in routine clinical practice.
Author contributionsMIDL and LGGR conceived and designed the study. MIDL, MGM and EMG collected laboratory test results. ECA and AMM contributed to the enrollment and classification of patients and clinical data collection. MTOM provided statistical advice to analyze the data. LGGR drafted the article, and EU contributed substantially to its revision. All authors have accepted responsibility for the entire content of this manuscript and approved its submission.
FundingThe author(s) received no financial support for the research, authorship, and/or publication of this article.
Disclosure statementThe authors report there are no competing interests to declare.