Incarcerated inguinal hernia is a pathology that we frequently encounter in emergency surgery. These hernias have traditionally been treated with open surgery, although laparoscopic techniques are being conducted with increasing frequency. In addition, usually one of the biggest concerns in these cases is determining intestinal viability and whether or not intestinal resection is necessary. In recent years, more hospitals now have laparoscopy towers that provide the possibility of indocyanine green (ICG) fluorescence imaging. The application of ICG can help us decide whether to perform intestinal resection.
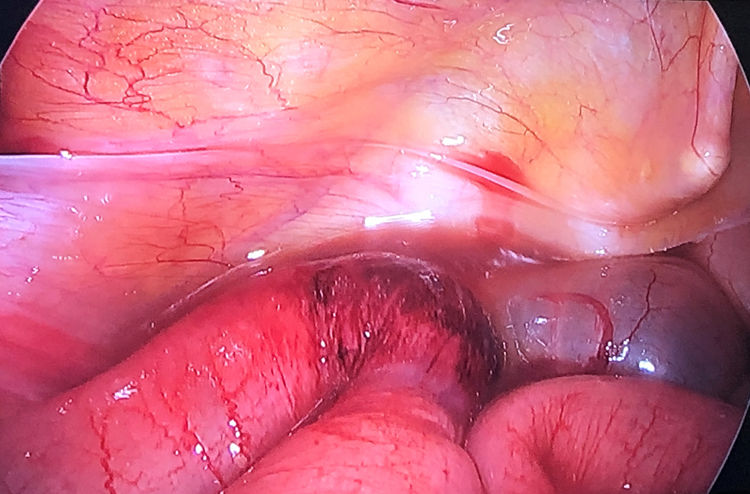
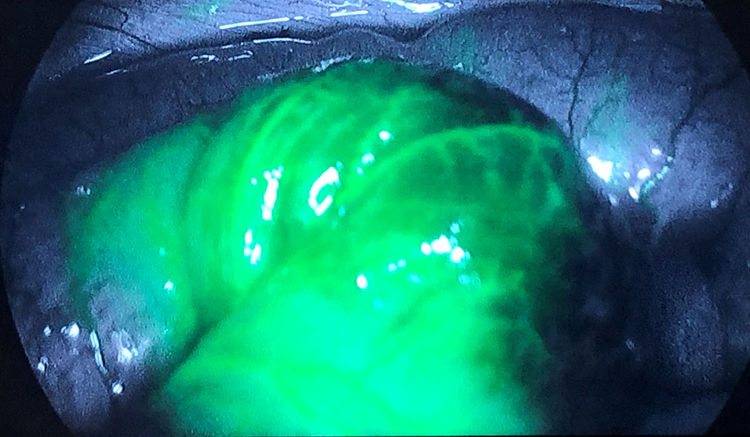
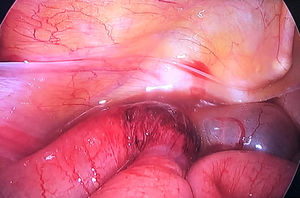
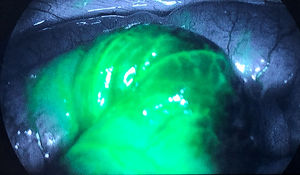
We present our experience with minimally invasive management of incarcerated inguinal hernia. In 2019, we operated on 6 patients using a transabdominal laparoscopic approach. Informed consent was obtained from all patients prior to the procedure. The incarcerated content was: the sigmoid colon (1), omentum (1) and small intestine (4). The hernia was reduced using gentle traction with atraumatic forceps. Subsequently, viability of the intestine was verified. In 3 of these patients (2 small intestine and one sigmoid), we decided to administer an intravenous injection of 2 mL indocyanine green (Verdye® 5 mg/mL), and perfusion of the intestinal loop was evaluated using 10 mm 30° optics, connected to a conventional white light and near infrared (NIR) light-emitting diode as well as a camera, which was connected to a specially equipped 4 K high-definition system (Platform 1588 AIM®, Stryker Endoscopy, San Jose, California, USA). Less than one minute after the injection, the vascularization of the intestinal wall was observed, which was normal in all cases and indicated no ischemia that would require resection. Figs. 1 and 2 demonstrate images of a case before and after the administration of indocyanine green. Subsequently, the hernia defect was repaired using a preformed BARD® 3DMax™ prolene mesh that was affixed with Hystoacryl®, and the peritoneum was closed using 3/0 barbed suture. All patients evolved favorably and were discharged between the first and third days. During the mean 6-month follow-up, one of the patients presented a seroma in the inguinal region, which was treated with conservative measures.
In the literature, there is a growing number of series about laparoscopic treatment of incarcerated inguinal hernia. In 2016,1 a series was published based on data from the National Surgery Quality Improvement Program of the American College of Surgeons (NSQIP-ACS), which compared 2688 laparoscopic approaches versus 15 562 open procedures, obtaining a lower rate of wound infection within 30 days and fewer complications; no differences were found in terms of mortality or reoperations in the first 30 days. Other more recent articles2–4 report series with varying numbers of patients (20-73 cases), generally with low morbidity, shorter hospital stay than in the case of open surgery, low wound/mesh infection rate, and zero mortality. The authors also mention the importance of having surgeons trained in this technique due to the learning curve.
The role of ICG has been reported in the assessment of intestinal viability in the case of acute mesenteric ischemia,5,6 as it is able to determine with greater precision the area to be resected, thereby avoiding major intestinal resections. In the case of macroscopically doubtful sections of the intestine, the use of ICG can guide us for their resection.
However, there are very few articles that mention the use of ICG to evaluate the intestine incarcerated in a hernia. In our bibliographic review, we found 4 case reports7–10 (3 of them by the same authors) that mentioned the use of ICG during urgent surgery for incarcerated hernia, 2 of which were laparoscopic procedures9,10 (one obturator hernia and one inguinal hernia). In all cases, the use of ICG was useful for assessing intestinal viability and deciding on resection.
In our opinion, ICG can be decisive in the assessment of intestinal viability during the laparoscopic management of incarcerated inguinal hernia, guiding the decision of whether to perform intestinal resection.
Please cite this article as: Gianchandani Moorjani R, Díaz García A, Rosat Rodrigo A, Barrera Gómez M. Uso de verde indocianina para la evaluación de la viabilidad intestinal en la cirugía laparoscópica urgente de hernia inguinal incarcerada. Cir Esp. 2021;99:313–314.