Up to 93% of patients undergoing abdominal surgery will develop intra-abdominal adhesions with the subsequent morbidity that they represent. Various substances have been tested for the prevention of adhesions with controversial results; the aim of our study is to compare the capability of pirfenidone in adhesion prevention against sodium hyaluronate/carboxymethylcellulose.
MethodsA randomized, prospective, longitudinal experimental study with Winstar rats. They were divided into 3 groups. The subjects underwent an exploratory laparotomy and they had a 4cm2 cecal abrasion. The first group received saline on the cecal abrasion, and groups 2 and 3 received pirfenidone and sodium hyaluronate/carboxymethylcellulose respectively. All rats were sacrificed on the 21st day after surgery and the presence of adhesions was evaluated with the modified Granat scale. Simple frequency, central tendency and dispersion measures were recorded. For the statistical analysis we used Fisher's test.
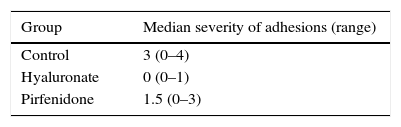
ResultsTo evaluate adhesions we used the Granat's modified scale. The control group had a median adhesion formation of 3 (range 0–4). The pirfenidone group had 1.5 (range 0–3), and the sodium hyaluronate/carboxymethylcellulose group had 0 (range 0–1). There was a statistically significant difference to favour sodium hyaluronate/carboxymethylcellulose against saline and pirfenidone (P<.009 and P<.022 respectively).
ConclusionsThe use of sodium hyaluronate/carboxymethylcellulose is effective for the prevention of intra-abdominal adhesions. More experimental studies are needed in search for the optimal adhesion prevention drug.
Hasta el 93% de los pacientes sometidos a una cirugía abdominal desarrollarán adherencias intraabdominales, con la subsecuente morbilidad que estas representan. Se han estudiado diversas sustancias para la prevención de adherencias con resultados controvertidos. El objetivo de nuestro estudio es comparar la capacidad de prevención de adherencias de la pirfenidona frente al hialuronato de sodio con carboximetil celulosa.
MétodoEstudio aleatorizado, prospectivo, longitudinal en modelo experimental en ratas Winstar. Se dividieron aleatoriamente en 3 grupos de estudio. A todos los animales se les realizó una laparotomía exploradora y se les provocó un deserosamiento de 4cm2 en el colon. El primer grupo recibió solución salina en la zona lesionada, los grupos 2 y 3 recibieron pirfenidona y hialuronato de sodio/carboximetilcelulosa, respectivamente. Al día 21 se sacrificaron las ratas y se evaluó la presencia de adherencias según la escala modificada de Granat. Registramos medidas de tendencia central y dispersión. Para el análisis estadístico se utilizó la prueba de Mann-Whitney.
ResultadosEn grupo control, la mediana de formación de adherencias fue de 3 (rango 0-4), para el grupo pirfenidona fue 1,5 (rango 0-3) y para el grupo hialuronato de sodio/carboximetilcelulosa 0 (rango 0–1). El empleo de hialuronato de sodio/carboximetilcelulosa es estadísticamente superior en la prevención de adherencias comparado con la solución salina y con pirfenidona respectivamente (p<0,009 y p<0,22).
ConclusionesEl empleo de hialuronato de sodio/carboximetilcelulosa es efectivo para la prevención de adherencias intraabdominales. Son necesarios más estudios experimentales en búsqueda del fármaco ideal para la prevención de adherencias.
Abdominal and pelvic surgical operations represent the majority of elective and emergency surgical procedures. As a result of these, up to 93% of postoperative patients develop some type of intra-abdominal adhesions.1,2
The clinical outcomes of these adhesions include infertility, pelvic pain, difficulty in subsequent abdominal surgery and intestinal obstruction. Colorectal surgery has been said to be the main cause of adhesions which lead to intestinal obstruction.3,4
Depending on the series, up to 75% of patients will develop symptoms of intestinal obstruction, while 3.8% will require surgical treatment. Postoperative adhesions cause 20% of all cases of infertility, and 40% of cases of pelvic pain in women.3–5
There are few studies on the new methods for regulating the inflammatory response in the peritoneal cavity.6–8 Experimental studies have confirmed the importance of tumour necrosis factor alpha (TNF-a), transforming growth factor beta (TGF-b), interleukin 1 beta (IL-1b) and interleukin 6 (IL-6), in the formation and maturation of intra-abdominal adhesions. All of these cytokines modulate the fibrinogenesis route and, as a result of this, by the end of the first week there are mature adhesions in the peritoneal cavity.9–16
The methods described in the literature to prevent intra-abdominal adhesions include types of surgical technique, pharmacological, biological and physical methods, amongst others, with highly variable results. Products derived from carboxymethyl cellulose plus sodium hyaluronate are the ones which have been shown to give the best results, and they have even been approved now for use in human beings.6,17–20
There is a type of salt in the market that is known for its antifibrotic, anti-inflammatory and antioxidant powers: pirfenidone. Although little is known about its mechanism of action, it is known to reduce the production of the cytokines involved in the formation of adhesions. This was proven by Tietze and Oku et al. in 2 different studies in animal models, as it reduces the expression of cytokines TNF-a, TGF-b, IL-1 and IL-6.21,22 In 1999 Iyer et al. documented the reduction in the expression of the procollagen gene in a pulmonary fibrosis model induced by bleomycin, reducing the formation of extracellular matrix.23 As well as experimental models in pulmonary fibrosis, its efficacy has also been studied in vivo in renal, hepatic and cardiac fibrosis models, in which a reduction in the expression of TGF-b was observed.24,25
Pirfenidone has also been shown to be safe in humans by prospective randomized studies. In 2007 Shi et al. studied the pharmacokinetic characteristics of pirfenidone in healthy patients. They found suitable absorption rates, with minimum adverse events that were tolerated well, and these events were reduced even more if it was taken with food.26 In 2011 Carter reported the preliminary findings of 2 double-blind prospective randomized studies in patients with mild to moderate idiopathic pulmonary fibrosis. He found significant improvements in terms of forced vital capacity in favour of pirfenidone, compared with a placebo from weeks 52 to 72 of treatment. The doses used varied from 1800mg/day to 2403mg/day, with a suitable safety profile when taken orally.27
This study has the aim of comparing the topical application of a product known for its decreasing effect on modulating scar-forming cytokines (pirfenidone) against a barrier method of proven efficacy in the prevention of postoperative adhesions (carboxymethyl cellulose with sodium hyaluronate) in an experimental model.
MethodA controlled, randomized, longitudinal and prospective study was undertaken in an experimental model of 30 female albino Wistar rats (Rattus norvegicus), weighing from 300 to 400g and from 6 months to one year of age. This type of rat was selected due to its suitable size for tissue manipulation, its infection-resistant immune system and its excellent scarring. Moreover, anatomically its colon is suitable for the type of surgical procedure to be performed. The study was carried out in the Research and Experimental Surgery Vivarium of the Hospital Central Sur de Alta Especialidad de PEMEX, Mexico City. This study was approved by the Research Ethics Committee of our hospital. Likewise, at all times the official Mexican rule number 062–1999 governing the production, care and use of laboratory animals was followed, together with the United States’ Guide for the care and use of laboratory animals.28
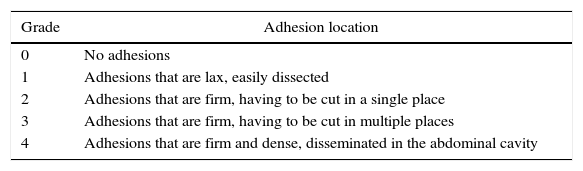
A sample was calculated based on the different averages expected in the formation of adhesions for an experimental study, with a total of 30 study subjects divided into 3 groups, to each one of which 10 individuals were assigned by simple randomization using a table of numbers. This determined that each experimental subject could correspond to one of the 3 possible treatments (pirfenidone, sodium hyaluronate with carboxymethyl cellulose or saline solution). Clinically healthy female rats that had not previously been used in any other experimental model were included. Clinically sick animals were excluded, as were pregnant females, those with previous abdominal surgery and those that had been included in another research project. Through laparotomy, each one of the 3 randomly-composed groups received a different preventive treatment against the formation of adhesions (saline solution, pirfenidone and sodium hyaluronate with carboxymethyl cellulose). All 3 groups of experimental subjects were sacrificed 21 days after the first surgery and the presence and severity of their adhesions were analysed by an observer unconnected to the study group using the modified Granat scale (Table 1).29
Granat's Modified Scale of Adhesions.
| Grade | Adhesion location |
|---|---|
| 0 | No adhesions |
| 1 | Adhesions that are lax, easily dissected |
| 2 | Adhesions that are firm, having to be cut in a single place |
| 3 | Adhesions that are firm, having to be cut in multiple places |
| 4 | Adhesions that are firm and dense, disseminated in the abdominal cavity |
Once the previously healthy rat had been selected it was anaesthetised by the intramuscular administration of ketamine (0.1mg/kg/dose). It was then placed on an operating table and the abdominal wall was prepared by shaving, asepsis and antisepsis of the wall using iodopovidone; a fenestrated sterile field was put into place. Through an average incision of approx. 5cm dissection in planes was performed until celiotomy, after which exploratory laparotomy was performed in quadrants to search for preformed peritoneal adhesions. After this the ascending colon was identified and a lesion was created in the serous membrane of this organ measuring approx. 4cm2 (1cm wide, 4cm long) using the cutting edge of the scalpel until bleeding could be seen. 3ml of 0.9% saline solution was applied to the roughened area in the control group; 3ml pirfenidone in 8% gel was applied to the same area in the pirfenidone group, and in the hyaluronate group 3ml of sodium hyaluronate (0.25%)/carboxymethyl cellulose (0.5%) was applied. The injured colon was replaced in the abdominal cavity and the peritoneum, muscle and aponeurosis was closed using a continuous 3–0 silk suture, while the skin was closed using 4–0 polypropylene in single stitches. The experimental animals went on to recover from the anaesthesia and were monitored daily after the operation. The rats were placed in grouped individual cages, with radiant heating. They were kept fasting for 12h and were given a prophylactic dose of antibiotic (Ceftriaxone 20mg/kg) and an analgesic (Metamizole 5mg/kg).30
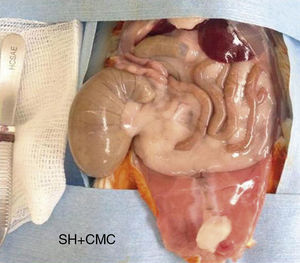
During the second phase of the study the rats were subjected to a new surgical examination 3 weeks after the first procedure. The rodents were sacrificed with a lethal dose of Pentobarbitone. An exploratory laparotomy was performed using a U-shaped incision along both flanks up to the epigastrium, deepening until the peritoneal cavity was reached. The adhesions formed were measured macroscopically according to Granat's modified grading. This scale was used because it measures the grade of adhesions and their severity based on their quality and distribution, and it has also been used in experimental rat models.29,31,32
Statistical AnalysisThe Mann–Whitney test for non-parametric variables was used for statistical analysis of the data, using the Epi Info™ version 7.1.4 program, as well as measuring core tendency and dispersion for the ordinal variables.
ResultsNone of the 30 individuals died after the operation to which they were subjected in the first phase of the study. In the second laparotomy, all of the individuals in each group were evaluated for the presence and grade of intra-abdominal adhesions according to Granat's modified scale.
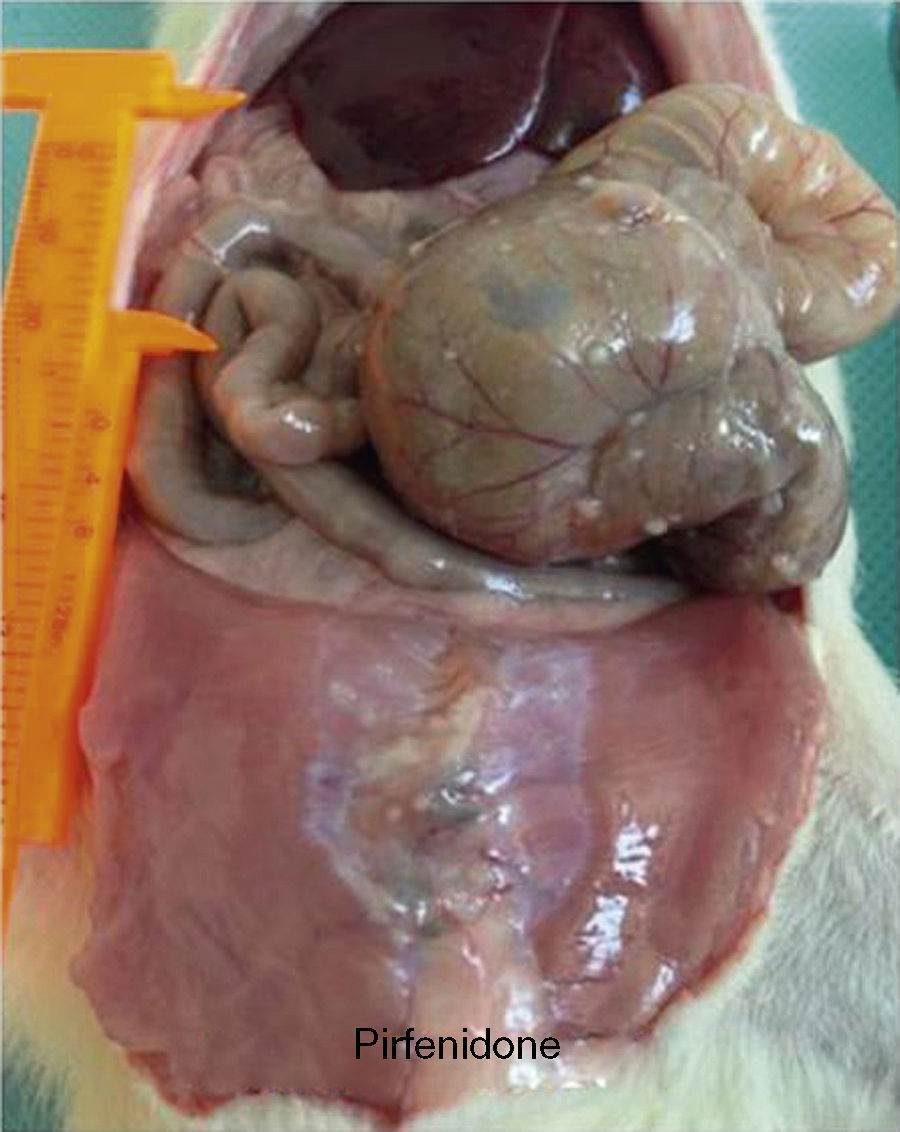
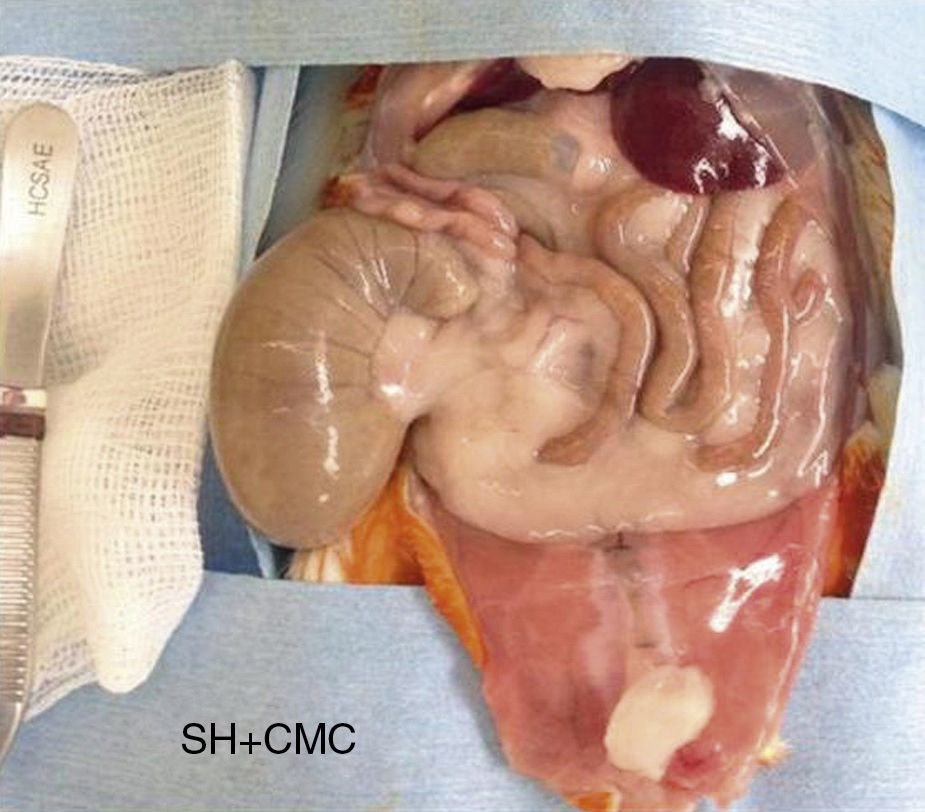
In the control group the median grade of adhesions was 3, with a range from 0 to 4 (Fig. 1). When this was compared with the median in the pirfenidone group (median 1.5, range 0–3), no statistically significant differences were found (P<.7) (Fig. 2). In the hyaluronate group the adhesion formation median was 0, with a range from 0 to 1 (Fig. 3). When this was compared with the control group median we found a difference in favour of the hyaluronate group (P<.009) and, in the same way, when the hyaluronate group was compared with the pirfenidone group, we found a reduction in the severity of the adhesions with P<.022 (Table 2).
This study showed experimentally that sodium hyaluronate with carboxymethyl cellulose is effective in the prevention of intra-abdominal adhesions following colon surgery. However, when pirfenidone was compared to sodium hyaluronate with carboxymethyl cellulose it was found to be less effective.
Our resultswith the use of sodium hyaluronate with carboxymethyl cellulose are similar to other previous publications in the literature.
In 2009 Kumar et al. undertook a meta-analysis of 7 randomized studies, 6 of which compared results with those in a control group. A significant reduction in the formation of adhesions was observed (OR 0.15; IC 95%: 0.05–0.43); P=.0005).7 In a more recent systematic revisiew Robb et al. found a significant reduction in the incidence of postoperative adhesions with the use of sodium hyaluronate with carboxymethyl cellulose, leading to a lower incidence of intestinal obstruction and the need for surgical treatment.33
The above-mentioned study contrasts with the one published by ten Broek et al., who in another systematic revisiew found no reduction in the need for surgery due to intestinal obstruction. Nevertheless, the use of sodium hyaluronate with carboxymethyl cellulose significantly reduced the surgical time in the second operation, such as stoma closure or hepatic metastasectomy, when necessary.34
With respect to the benefits for gynaecological surgery, Hindocha et al. undertook a revision of the studies published by the Cochrane library that included the use of agents to prevent the formation of intra-abdominal adhesions. The main objective was to determine their efficacy in reducing pelvic pain and infertility. None of the studies revised by this author demonstrated a direct benefit in terms of their primary objectives.35
In our study, the use of sodium hyaluronate with carboxymethyl cellulose in comparison with the control group showed a difference in the formation of adhesions, with P<.009.
Different studies have focused on the modulation of the local inflammatory response which causes intra-abdominal adhesions. They studied cyclo-oxigenase inhibitors, antibiotics, hypertonic solution, heparin and other substances, with controversial results.31,32,36,37 In the particular case of using pirfenidone, no previous studies have been published. In our study we observed a direct reduction in the median severity of the adhesions, without reaching a statistically significant difference in comparison with the control group (P<.7).
Macías-Barragán et al. reported beforehand on the use of pirfenidone in an 8% gel as a treatment for hypertrophic scars secondary to burns. After 6 months of topical application they observed resolution of the hypertrophic scars that was significant compared to the untreated scars.25 In our study we used a different type of presentation as a gel, and we also used a different dose, exposure time and route of administration. However, we have to point out that our primary aim was to prevent and not reverse the effects of fibrinogenesis.
The relevance of our study centres on the fact that it is one of the first to use intraperitoneal pirfenidone. However, this same fact leads to one of its limitations, because due to the lack of previous experiences, the dose of pirfenidone used may have been suboptimal.
Another important aspect is that although the surgical technique used strictly followed the criteria of asepsis and antisepsis, the sterility of the gel presentation that we used during application could not be guaranteed, according to the manufacturer's specifications. Although the animal model used has an excellent immune system, and we complied with the principles of antimicrobial prophylaxis, a possible distortion in the presentation of adhesions may have arisen due to the commercial presentation of the pirfenidone, thereby increasing the incidence and severity of adhesions in comparison with sodium hyaluronate with carboxymethyl cellulose. Another possible limitation may be the size of the sample.
Aside from the results, we wish to underline that pirfenidone is used to prevent intra-abdominal adhesions. There are in fact protocols in the recent literature that focus on the prevention of postoperative fibrosis in breast surgery by using oral pirfenidone. In the previous example, the physiopathology of breast capsule contraction follows a very similar pattern to that of the formation of intra-abdominal adhesions.38,39 A second means of preventing intra-abdominal adhesions may be to administer this same active ingredient orally in the experimental model, with the aim of modifying the fibrinogenesis cascade through intestinal absorption. This would also give us better control of the dose given, as the pharmacokinetics of this salt are perfectly well known while, at the same time, we could eliminate the distorting factor of the intraperitoneal application of the gel.
The formation of adhesions is a problem that does not only affect colorectal surgery, as it also arises in gynaecological, oncological, gastrointestinal and orthopaedic surgery, as well as in neurosurgery.9–11 We believe it to be pertinent to continue implementing protocols to study the effects of pirfenidone to prevent the formation of adhesions due to its antifibrotic qualities.
To conclude, the use of sodium hyaluronate in an experimental model proved superior in preventing the formation of intra-abdominal adhesions in comparison with the control group using saline solution and 8% pirfenidone gel, with a statistically significant difference. More experimental studies are required to seek the ideal drug to prevent adhesions.
Conflict of InterestsThe authors declare that they have no conflict of interests.
Please cite this article as: Bello-Guerrero JA, Cruz-Santiago CA, Luna-Martínez J. Pirfenidona frente a hialuronato de sodio/carboximetilcelulosa como preventivos de la formación de adherencias intraabdominales tras cirugía colónica. Estudio aleatorizado en modelo experimental. Cir Esp. 2016;94:31–37.