We present our experience of 100 consecutive cases who underwent ambulatory cholecystectomy using a standard protocol of anesthesia and surgery.
Patients and methodProspective study of 100 consecutive patients assessed in the surgery outpatient clinic in Torrevieja Hospital (September 2008–September 2009). Both anesthetic and surgical techniques were protocolized, standardized. The protocol included the use of intraperitoneal and parietal anesthesia.
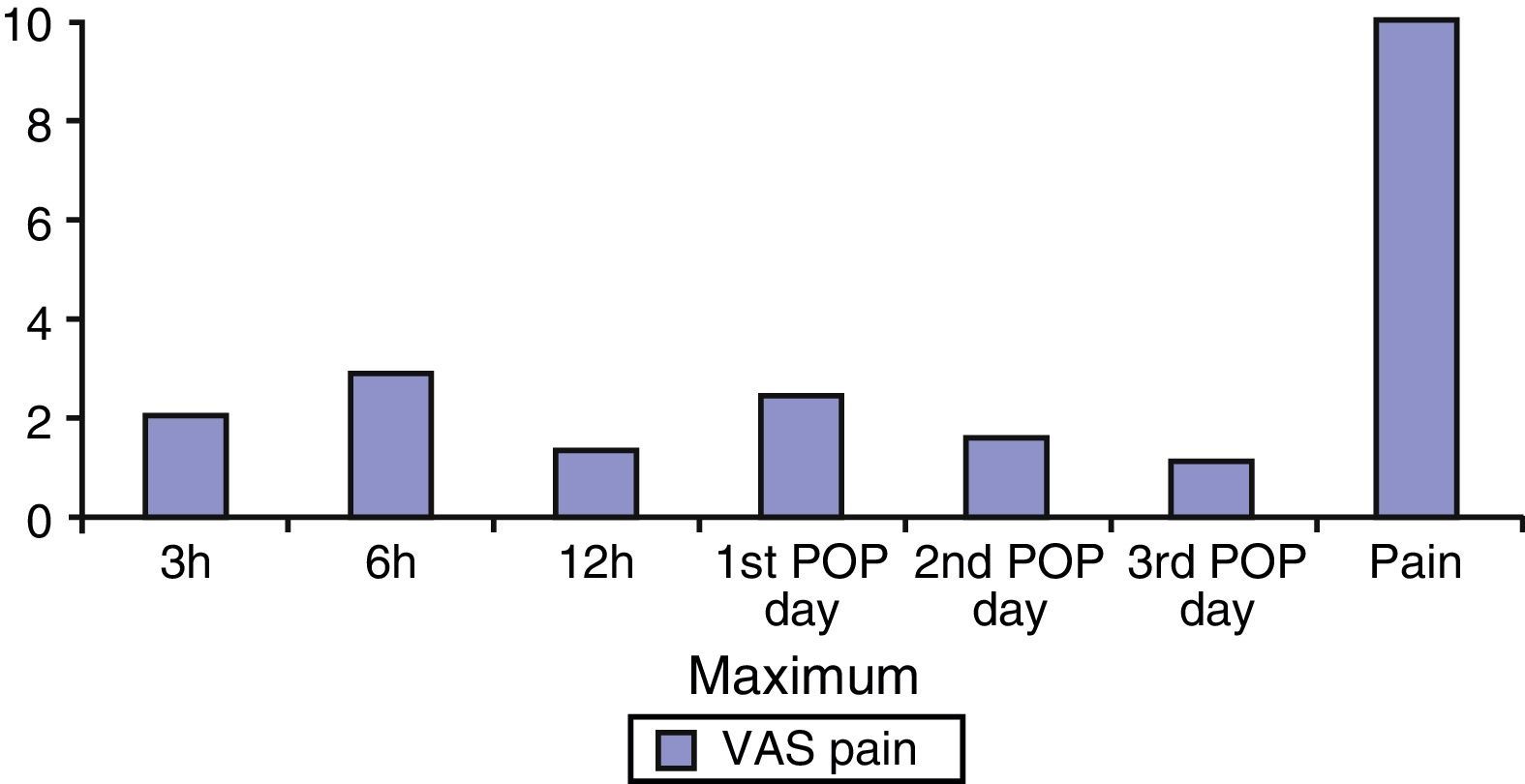
ResultsOne hundred patients were included. Average age was 53 years and average surgical time was 29±12min. Day-case surgery rate was 96%. Postoperative pain (VAS scale) was less than 4 in all cases. Six patients complained of nausea that eased with the administration of ev metoclopramide. Average length of stay in the day-case surgery unit was 7.4h (maximum 9.6, minimum 7). Morbidity and mortality rates were 0%. No re-admission was registered and conversion rate was 0%. Postoperative follow-up was 100%. A total of 97% of the cases were fully satisfied with the procedure.
ConclusionAmbulatory laparoscopic cholecystectomy is a feasible and safe technique. Postoperative pain has classically been the reason to not perform day-case surgery, but we achieved an excellent control by the combined use of local anesthetics and warm intraperitoneal saline solution.
Describimos la experiencia de nuestro grupo en la colecistectomía laparoscópica ambulatoria en una serie de 100 casos consecutivos sometidos a un proceso protocolizado de anestesia y cirugía.
Pacientes y métodoEstudio prospectivo de 100 pacientes consecutivos remitidos a consultas externas de Cirugía General del Hospital de Torrevieja (septiembre de 2008 y septiembre de 2009). La técnica anestésica y quirúrgica fue protocolizada incluyendo el uso intraperitoneal y parietal de anestesia local.
ResultadosLa media de edad fue de 53 años. El tiempo quirúrgico medio fue de 29±12min.
La tasa de ambulatorización fue del 96%. La media del dolor postoperatorio en ningún caso superó el valor de 3 en la escala EVA. Seis pacientes sintieron náuseas que cedieron tras la administración de metoclopramida iv.
La estancia media en el hospital de los pacientes ambulatorizados fue de 7,4 h (mínimo de 7 y máximo de 9,6). La morbilidad de la serie fue 0%, y la mortalidad de la misma también fue de 0%. La tasa de conversión a laparotomía de la serie fue del 0%.
Ningún paciente requirió reingreso tras el alta. El seguimiento postoperatorio fue del 100%.
El 97% de los pacientes ambulatorizados se encontraban muy satisfechos con el procedimiento.
ConclusiónLa colecistectomía laparoscópica ambulatoria en una técnica segura y fácilmente realizable. El dolor postoperatorio, principal causa de la no ambulatorización clásicamente, presenta un buen control tras el uso combinado de anaestesia local y suero fisiológico caliente intraperitoneal.
Laparoscopic cholecystectomy is the usual treatment for symptomatic cholelithiasis. This approach provides less duration and intensity of pain than open cholecystectomy, although it does not eliminate it completely; thus, even with this approach route, postoperative pain has been the most important limiting factor for the performance of outpatient laparoscopic cholecystectomy; for this reason, at present, most laparoscopic cholecystectomies are still performed with a hospitalization period ranging from 24 to 48h.1–3
In 1990, Reddick and Olsen introduced the concept of outpatient laparoscopic cholecystectomy when they published a series composed of 83 patients who underwent surgery, achieving a day-case surgery rate of 45% with a minimal complication rate.4 In our country, several groups have performed this kind of approach in a major ambulatory surgery regimen,5–14 and, recently, small series of patients who underwent a single-port laparoscopic cholecystectomy in a day-case program with good results have been published.10–12,14 However, laparoscopic cholecystectomy has not been widely accepted in our country or in the rest of Europe as one of the procedures suitable for day-case management, since some authors believe that this regimen may lead to a late detection of potential complications derived from the surgical process and, most frequently, the early onset of postoperative symptoms such as vomiting or abdominal pain, which hinders the early discharge of patients.3,15
We present our series composed of 100 consecutive cases of patients prospectively collected, who underwent an outpatient laparoscopic cholecystectomy.
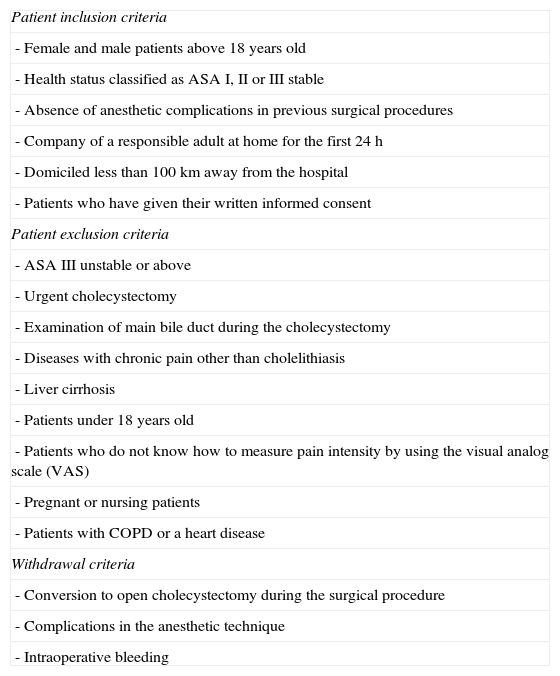
Material and MethodAn outpatient laparoscopic cholecystectomy was performed in all consecutive cases of patients meeting the inclusion criteria and none of the exclusion criteria (Table 1); they were submitted to a mobilization program and early oral intake following the use of physiological saline solution and intraperitoneal and parietal local anesthesia with ropivacaine. Postoperative pain and nausea, percentage of day-case surgery achieved, complications, admission and readmission rates and satisfaction of patients who underwent surgery were assessed.
Patient Inclusion and Exclusion Criteria.
| Patient inclusion criteria |
| - Female and male patients above 18 years old |
| - Health status classified as ASA I, II or III stable |
| - Absence of anesthetic complications in previous surgical procedures |
| - Company of a responsible adult at home for the first 24h |
| - Domiciled less than 100km away from the hospital |
| - Patients who have given their written informed consent |
| Patient exclusion criteria |
| - ASA III unstable or above |
| - Urgent cholecystectomy |
| - Examination of main bile duct during the cholecystectomy |
| - Diseases with chronic pain other than cholelithiasis |
| - Liver cirrhosis |
| - Patients under 18 years old |
| - Patients who do not know how to measure pain intensity by using the visual analog scale (VAS) |
| - Pregnant or nursing patients |
| - Patients with COPD or a heart disease |
| Withdrawal criteria |
| - Conversion to open cholecystectomy during the surgical procedure |
| - Complications in the anesthetic technique |
| - Intraoperative bleeding |
All patients that made a consultation at the General Surgery Unit of Torrevieja Hospital between September 2008 and September 2009 for assessment of laparoscopic cholecystectomy, who met all the inclusion criteria and none of the exclusion criteria and who, once informed, accepted this kind of surgery in a day-case regimen and signed the informed consent sheet, apart from the usual consent obtained from all the patients undergoing a laparoscopic cholecystectomy and with general anesthesia, were included in the study.
Technique DesignBefore the scheduled surgery, antibiotic prophylaxis was systematically performed with 2g of IV amoxicillin-clavulanic acid. In case of allergy to penicillin, IV ciprofloxacin 400mg was administered.
Anesthesia Protocol of the Scheduled SurgeryAll procedures were performed in the morning and the patients were admitted to the hospital on that same day. Surgical procedures were systematically performed with general anesthesia, and the anesthetic procedure was protocolised. During the premedication period (30min before the start of the procedure), dexamethasone (4mg) plus dexketoprofen (50mg) and IV ranitidine were administered to all patients. During the induction phase, propofol (3–5mcg/mL) with remifentanil (0.05–0.10mcg/kg/min) and cisatracurium (0.1mg/kg) were administered. Anesthesia was maintained with propofol and remifentanil, adjusting the induction dose to the patient's BP and stability. Before the end of the procedure, 1g of IV paracetamol was administered.
In the Day-Case Surgery Unit AreaTo maintain analgesia, dexketoprofen 50mg IV/100 SS/8h+paracetamol 1g/8h were administered.
If the patient had nausea and vomiting, one vial of IV metoclopramide was administered.
Treatment of postoperative pain at home was also protocolised as follows:
- -
Dexketoprofen 25mg every 8h PO+paracetamol 1g every 8h PO
- -
Tramadol tablets, one tablet every 8h as rescue analgesia
- -
Metoclopramide tablets, one tablet every 8h, if nausea
The surgical technique was performed with three trocars and by the same two surgeons in all cases. As a local anesthetic, ropivacaine (Naropin® Polybag) 200mg in a 100-mL bag (ropivacaine 2m[sic: mg]/mL) was used. A pneumoperitoneum was created with the Hasson technique, using a 10-mm umbilical trocar (infiltration with local anesthesia before placing the trocar). The rest of the trocars (5 and 11mm) were inserted under direct vision, prior infiltration of local anesthesia in the ports: 10mL of solution containing ropivacaine hydrochloride (Naropin®) (2mg/mL) were infiltrated around the entry ports: 4mL in the umbilical port and 2mL in the other ports.
The gas used in all cases was carbon dioxide (CO2). During laparoscopy, the maximum intra-abdominal pressure used was 12mmHg.
The right hemidiaphragm was irrigated at the start of the procedure with 40mL of ropivacaine solution (2mg/mL). Subsequently, at the end of the procedure, 500 cc of 0.9% physiological saline solution at a temperature of 37°C was infused intraperitoneally in the right hemidiaphragm, and suctioned. The surgical time and bleeding during surgery were recorded in each case.
Postoperative management was carried out in a fast-track regimen. All patients were mobilized at an early stage, starting with sitting position in a sofa 4h after the start of surgery and walking 6h after the start of surgery. The start of oral intake was performed with the patient in a sitting position 4h after the start of the anesthetic induction.
During hospital stay, the need for additional non-protocolised analgesics or antinauseant drugs was recorded in the case record form.
Hospital discharge was decided based on the following criteria:
- -
Normal and stable vital signs
- -
Pain controllable with oral analgesics
- -
Absence of nausea and vomiting
- -
Absence of wound bleeding
- -
Established oral tolerance
- -
Ability to walk independently without aids.
Length of stay in hospital was defined as the period ranging from the end of the anesthetic induction to the time of the definitive discharge from the site.
Patients with a length of stay less than 12h were considered outpatients.
Patients with a length of stay equal to or greater than 12h were considered inpatients.
Readmission CriteriaPatients who required a new admission after hospital discharge, regardless of the previous length of stay after surgery, were considered readmissions.
Pain RecordPain was assessed 3, 6, 12, 24 and 72h after the procedure. To measure it, a double procedure was used:
- -
Visual Analog Scale (VAS) of pain, rated from 1 to 10 (from “0=no pain” to “10=the worst pain”)
- -
The need for additional analgesics outside the established protocol for the postoperative period.
These data were recorded per patient in the “patient questionnaire” given to each one of them. Sensation of nausea or vomiting was assessed at the same time points as pain.
All patients filled in a self-administered questionnaire and received instructions on how to assess pain and nausea, as well as the consumption of protocolised and non-protocolised analgesics.
Monitoring and Follow-up of PatientsThe follow-up period lasted one month, following the scheme below:
Seven hours after the end of the surgery, hospital discharge or hospital admission was assessed by a surgeon based on compliance with discharge criteria.
Mandatory personal phone contact with the patient was maintained by a nurse of the Day-case Surgery Unit or a surgeon 24, 48 and 72h after discharge.
Patients were appointed for a follow-up visit seven days after the procedure and after one month.
Outpatients received written postoperative instructions containing general information on postoperative measures and care, as well as signs and symptoms that should alert and oblige them to make inmediate phone contact.
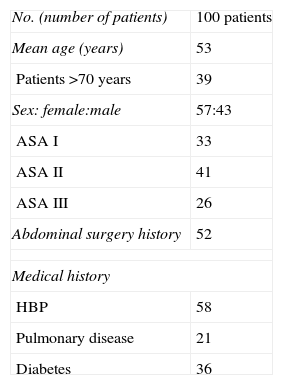
ResultsBetween September 2008 and September 2009, 100 patients underwent an outpatient laparoscopic cholecystectomy (43 men and 57 women). Mean age was 53 years with a range between 18 and 87 years. The mean body mass index of patients was 31, with only 15% with a body mass index less than or equal to 25. Table 2 summarizes the rest of the characteristics of the series.
The mean surgical time was 29min (minimum 17min and maximum 41min). Estimated mean intraoperative bleeding was 50 cc (minimum 0 and maximum 125 cc).
Ninety-six percent of patients (96 patients) were outpatients, with a day-case surgery failure of four patients. The reasons to not perform day-case surgery included: three patients due to medical criteria related to the surgical findings and one patient due to his/her refusal to be discharged despite having signed the consents before the surgery, having been duly informed and meeting all the criteria for the day-case surgery.
The mean postoperative pain did not exceed the value of 3 in the VAS scale (Fig. 1) in any case; 3, 6 and 12h after the procedure, the pain score was 2.1, 2.9 and 1.3; the first postoperative day it was 2.4, the second day 1.5 and the third day 1.1. No patient required non-protocolised analgesics.
Six patients complained of nausea during their hospital stay, five of them 3h after the procedure and one of them 6h after the procedure, which eased with the administration of IV metoclopramide.
Average length of stay in hours in the day-case surgery unit was 7.4h (minimum 7 and maximum 9.6h). For inpatients, length of stay was 3.2, 1.5, 2.2 and 1.3 days. The morbidity of the series was 0% and mortality was also 0%. The rate of conversion to laparotomy of the series was 0%.
No patient required readmission after discharge. Postoperative follow-up was 100%.
Regarding patient's satisfaction level, 97% of outpatients were very satisfied with the procedure and 100% of them would recommend it to a family member or friend.
DiscussionThe mechanisms that produce pain after laparoscopic cholecystectomy have not been completely clarified, although it is known that they include different components, such as abdominal wall trauma, intra-abdominal trauma secondary to gallbladder removal, distended abdomen due to the insufflated gas and the pneumoperitoneum created by the CO2.16 However, some factors may influence the postoperative pain level, such as the residual intra-abdominal gas volume at the end of the surgery or the temperature of the insufflated gas.1 The remaining CO2 that stays in the peritoneal cavity for a couple of days and local hypothermia induced by the insufflated gas generally cause pain in shoulders and abdomen, especially when early walking is started, and pain starts a few hours after the procedure and lasts for 48h on average.2
Infiltration of local anesthesia in the surgical ports provides some benefit for reducing pain, although its real effect has not yet been studied.17–20 Moreover, previous studies have analyzed the use of several local intraperitoneal anesthetics such as bupivacaine or ropivacaine, as well as infusions with saline solutions to reduce postoperative pain in laparoscopic surgery, with variable results. The results of the studies with bupivacaine used as local intraperitoneal anesthesia have shown that length of pain suppression was limited and no benefits were recorded regarding hospital discharge and early return to activity.17 Other authors have observed a decrease in postoperative pain after intraperitoneal instillation with ropivacaine. Ropivacaine is a long-acting, amide-type local anesthetic with pharmacodynamic and pharmacokinetic properties similar to those of bupivacaine, although it has less adverse effects than the latter in terms of the central nervous system and circulatory system.
Labaille et al.18 found that 100mg of ropivacaine instilled intraperitoneally at the start of the procedure is the optimal dose to reduce postoperative pain, although no benefit was obtained in terms of postoperative demand of analgesics.
Kucuk et al.19 using 150mg of ropivacaine, observed a decrease in postoperative pain and in the consumption of analgesics. Pappas-Gogos et al.20 used 155mg of ropivacaine distributing them in the trocar wounds (75mg) and intraperitoneally (80mg), after which a decrease in postoperative pain sensation was observed. No ropivacaine-related side effects were observed in any of the three studies.
All these studies were conducted with inpatients, and in none of them the possibility of a major ambulatory surgery regime was considered.
In our study, control of pain and nausea was optimal, which has undoubtedly contributed to the rate day-case surgery achieved, although there are certainly other factors of vital importance that depend both on the surgeon and the patient.
In recent years, several series of outpatient laparoscopic cholecystectomy with good results have been published.4–14,21,22 However, outpatient laparoscopic cholecystectomy is not widely disseminated yet,3 since, as we have already mentioned, the day-case regimen depends on the patient and the surgeon.9 In this sense, we believe that prior selection and education of patients is crucial before surgery, during the consultation, as well as a personalized surgeon-patient relationship, in order to eradicate the old popular belief unsupported by scientific data related to the fact that the longer the hospital stay, the better the health care.
Furthermore, as stated by Planells et al.,9 for the day-case surgery to be successful it should be performed by surgeons trained for a reduced postoperative course, since the clinical practice heterogeneity already mentioned by Bisgaard et al.,2 has a catastrophic effect, given that it combines old-fashioned postoperative practices with the postoperative recovery in this kind of fast-track regimen, thus decreasing the process success rate. Moreover, patient satisfaction analysis shows that in this study, as well as in previous ones, the patient is satisfied with the process, and the management is even more satisfied, since day-case surgery involves savings by reducing average length of stay and minimizing postoperative care and treatment, as stated by Planells et al.,9 who indicate that a conversion rate of 70% in cholecystectomies to day-case regimen would involve a saving of 76 million Euros considering only length of stay.
ConclusionOur study supports that outpatient laparoscopic cholecystectomy is a safe and feasible technique. Postoperative pain, classically the main reason to not perform a day-case surgery, shows good control after the combined use of local anesthesia and warm physiological saline solution administered intraperitoneally and in the entry ports, enabling early mobilization and oral intake, necessary conditions for day-case surgery, although the correct selection of patients and the personalized surgeon–patient relationship for patient education on the process is a key factor for success.
Conflicts of InterestThe authors declare that they do not have any conflicts of interest.
Please cite this article as: Jiménez Fuertes M, Costa Navarro D. Colecistectomía laparoscópica ambulatoria y control del dolor postoperatorio: presentación de una serie de 100 casos. Cir Esp. 2015;93:181–186.