The role of oral antibiotic prophylaxis and mechanical bowel preparation in colorectal surgery remains controversial. The lack of efficacy of mechanical preparation to improve infection rates, its adverse effects, and multimodal rehabilitation programs have led to a decline in its use. This review aims to evaluate current evidence on antegrade colonic cleansing combined with oral antibiotics for the prevention of surgical site infections. In experimental studies, oral antibiotics decrease the bacterial inoculum, both in the bowel lumen and surgical field. Clinical studies have shown a reduction in infection rates when oral antibiotic prophylaxis is combined with mechanical preparation. Oral antibiotics alone seem to be effective in reducing infection in observational studies, but their effect is inferior to the combined preparation. In conclusion, the combination of oral antibiotics and mechanical preparation should be considered the gold standard for the prophylaxis of postoperative infections in colorectal surgery.
El papel de la profilaxis antibiótica oral y la preparación mecánica de colon en cirugía colorrectal es controvertido. La falta de eficacia del lavado mecánico para disminuir la infección, sus efectos indeseables y los programas de rehabilitación multimodal han reducido su uso. Esta revisión pretende evaluar la evidencia actual sobre la preparación mecánica anterógrada combinada con el antibiótico oral en la prevención de la infección de localización quirúrgica. En estudios experimentales, los antibióticos orales disminuyen el inóculo intraluminal y en los tejidos intervenidos. Los estudios clínicos muestran disminución de la infección con la profilaxis oral combinada con preparación mecánica. La administración de antibiótico oral en ausencia de limpieza mecánica del colon parece tener eficacia en estudios observacionales, pero su efecto es inferior a la preparación combinada. En conclusión, la preparación oral combinada mecánica y antibiótica debería considerarse el gold estándar de la profilaxis de la infección postoperatoria en cirugía colorrectal.
Surgical site infections (SSI) are the most frequent postoperative complications and the first cause of infection related to medical institutions in Spain (21.6%)1 and in Europe (19.6%).2 Colorectal surgery has the highest associated SSI rate of abdominal surgeries, with figures that can reach 20% in incidence studies with 30-day postoperative follow-ups.3–5
SSI represent an important financial burden for the national healthcare system, with increased consumption of antibiotics and longer mean hospital stay.6 Organ/space SSI (SSI-o/s) in colorectal surgery triples hospital stay and is associated with a 23% rate of readmissions, 60% reoperations and 29% need for intensive care.7
The etiopathogenesis of incisional SSI (superficial or deep) and that of SSI-o/s in colon and rectal surgery are probably different given the influence of suture dehiscence in the latter; therefore, their prevention strategies could be also different. Among the numerous measures proposed for the prevention of SSI in surgery,8 some are exclusive for colorectal surgery. These include mechanical bowel preparation (MBP) and oral antibiotic prophylaxis. Although there is broad consensus that antibiotic prophylaxis is essential before colorectal surgery, it is still debated whether antibiotics should be administered only systemically or through a combination of oral and intravenous therapies. On the other hand, the role of MBP and the option of performing it with or without oral antibiotics has been widely discussed.9–11
For the last two decades, the development of multimodal rehabilitation programs in colorectal surgery12 and the publication of numerous studies have fueled this controversy, leading to the re-evaluation of the indication of MBP and oral antibiotics in patients undergoing elective colon or rectal surgery.13,14 The aim of the present review was to analyze the current evidence on the combination of MBP and oral antibiotics or the use of antibiotics alone in the prevention of SSI.
MethodsWe carried out a narrative review of the literature through PubMed and the following platforms: Tripdatabase, National Guideline Clearinghouse and The Cochrane Library. We also consulted the websites of the Centers for Diseases for Control and Prevention, the European Center for Diseases for Control and Prevention, The National Institute of Health and Clinical Excellence, The Canadian Patient Safety Institute, The Society for Healthcare Epidemiology of America, the Infectious Diseases Society of America and The National Health Service Scotland. For the bibliographic search, MeSH terminology was used under the topics: postoperative complications; surgical wound infection; anastomotic leak; prevention and control; and antibiotic prophylaxis. Additional searches were developed using the terms: colorectal surgery; oral antibiotic prophylaxis; mechanical colon preparation; mechanical colon cleansing; and surgical site infection. The inclusion criteria were: clinical practice guidelines, controlled clinical studies, cohort studies, meta-analyses, and systematic reviews. The bibliographic search was carried out by a single researcher. The review of the selected documents and the inclusion decision was made by the two researchers.
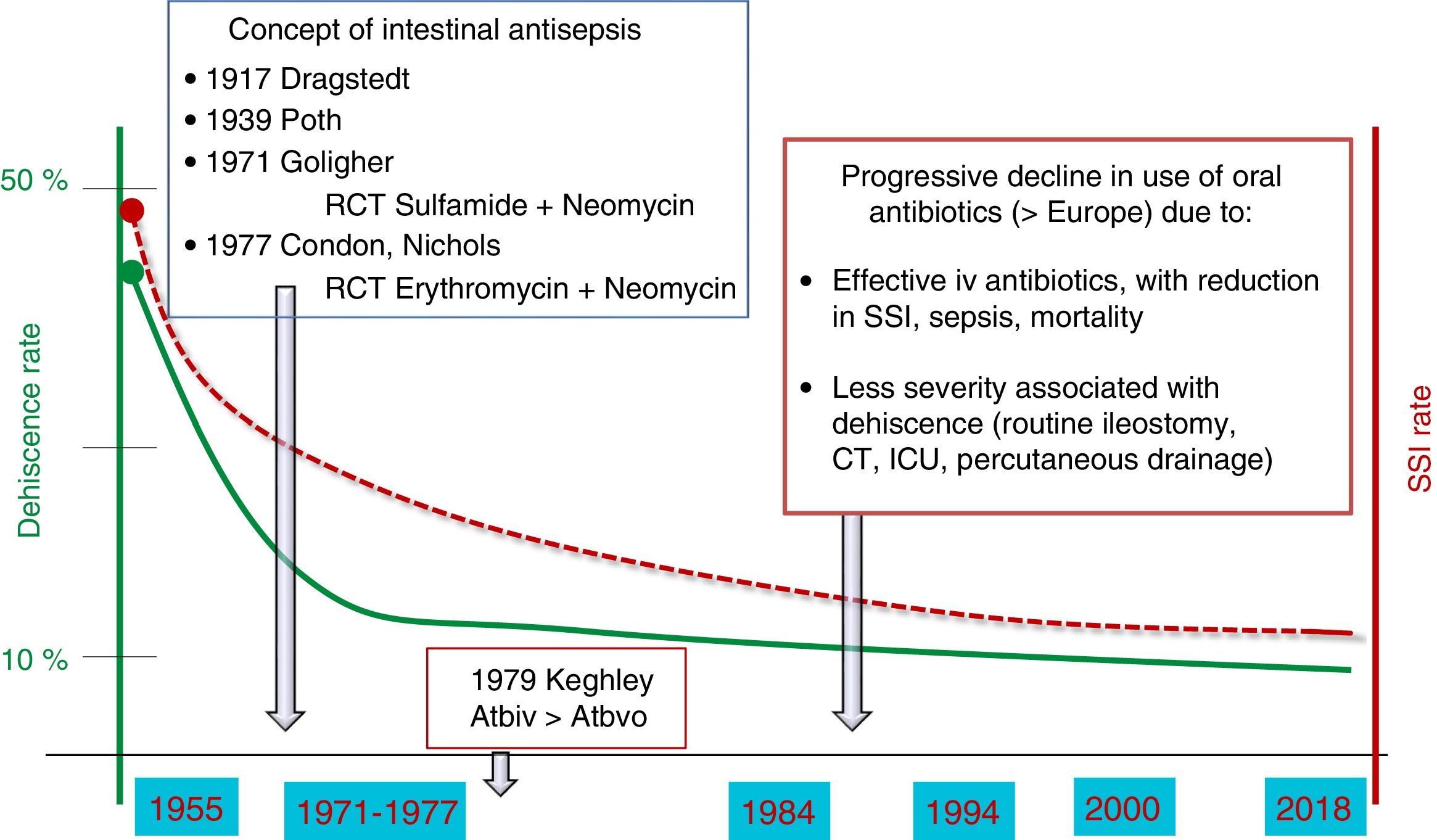
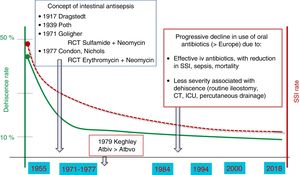
ResultsMechanical Colon PreparationMBP became popular in the 1930s with the intention of reducing the colon fecal content and bacterial inoculum in the tissues during operative manipulation or as a consequence of a suture dehiscence15 (Fig. 1). However, experimental studies pointed out that MBP alone did not obtain a decrease in the bacterial content of the colon16 and began to investigate the effect of adding oral antibiotics to the preparation.17 In 1971, Nichols and Condon experimentally demonstrated that the addition of nonabsorbable oral antibiotics (kanamycin and erythromycin base) to MBP reduced fecal aerobic and anaerobic flora.18 In 1977, in a randomized clinical study (RCT) without systemic antibiotics comparing oral antibiotic and placebo, the same authors correlated the bacterial reduction obtained by oral antibiotics with a lower rate of postoperative SSI.19 In spite of confirming the effect of oral prophylaxis, it was considered that the combination with MBP was necessary to reduce the fecal mass and, in theory, the bacterial inoculum of the intestinal lumen.
Subsequently, an RCT20 compared intravenous prophylaxis against oral prophylaxis and demonstrated the superiority of the former, universalizing systemic prophylaxis in colorectal surgery. Since the 1980s, intravenous prophylaxis continued to be used in combination with oral antibiotics in the United States and Canada, while oral prophylaxis was gradually abandoned in Europe.
The definitive decline of oral antibiotics began at the beginning of the 21st century, when several RCT compared MBP against non-preparation while maintaining systemic antibiotic prophylaxis in the two study arms.20,21 It demonstrated that omitting MBP did not increase complications in colon and rectal surgery. In addition, severe complications associated with MBP were described, such as electrolyte imbalances, seizures or spontaneous esophageal rupture.23
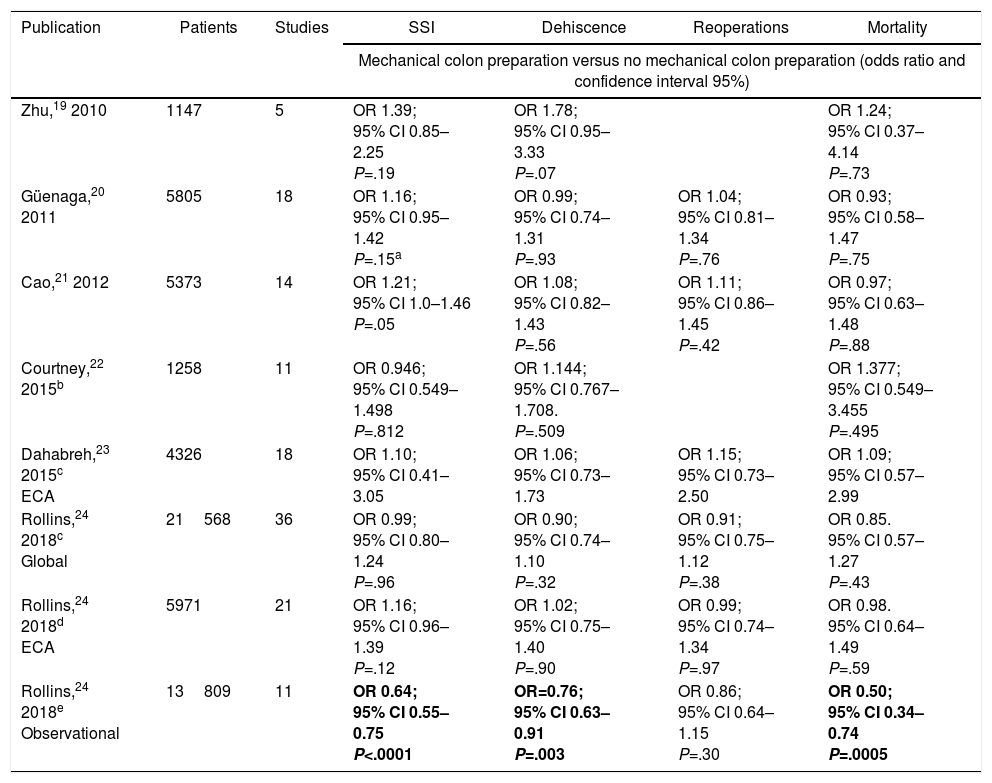
Since 2010, six meta-analyses have been published24–29 comparing MBP versus non-MBP with diverse methodologies, the results of which are summarized in Table 1. In general, there is a lack of effect observed of MBP on the incidence of suture dehiscence, SSI, reoperations and mortality. Some analyze colon or rectal interventions separately and others also compare MBP versus preparation with enemas, with similar results in both comparisons. Recent recommendations of the WHO include a meta-analysis comparing MBP vs no MBP,30 where there are no differences in SSI-o or dehiscence rate either.
Summary of the Results of the Metanalyses About Mechanical Colon Preparation.
| Publication | Patients | Studies | SSI | Dehiscence | Reoperations | Mortality |
|---|---|---|---|---|---|---|
| Mechanical colon preparation versus no mechanical colon preparation (odds ratio and confidence interval 95%) | ||||||
| Zhu,19 2010 | 1147 | 5 | OR 1.39; 95% CI 0.85–2.25 P=.19 | OR 1.78; 95% CI 0.95–3.33 P=.07 | OR 1.24; 95% CI 0.37–4.14 P=.73 | |
| Güenaga,20 2011 | 5805 | 18 | OR 1.16; 95% CI 0.95–1.42 P=.15a | OR 0.99; 95% CI 0.74–1.31 P=.93 | OR 1.04; 95% CI 0.81–1.34 P=.76 | OR 0.93; 95% CI 0.58–1.47 P=.75 |
| Cao,21 2012 | 5373 | 14 | OR 1.21; 95% CI 1.0–1.46 P=.05 | OR 1.08; 95% CI 0.82–1.43 P=.56 | OR 1.11; 95% CI 0.86–1.45 P=.42 | OR 0.97; 95% CI 0.63–1.48 P=.88 |
| Courtney,22 2015b | 1258 | 11 | OR 0.946; 95% CI 0.549–1.498 P=.812 | OR 1.144; 95% CI 0.767–1.708. P=.509 | OR 1.377; 95% CI 0.549–3.455 P=.495 | |
| Dahabreh,23 2015c ECA | 4326 | 18 | OR 1.10; 95% CI 0.41–3.05 | OR 1.06; 95% CI 0.73–1.73 | OR 1.15; 95% CI 0.73–2.50 | OR 1.09; 95% CI 0.57–2.99 |
| Rollins,24 2018c Global | 21568 | 36 | OR 0.99; 95% CI 0.80–1.24 P=.96 | OR 0.90; 95% CI 0.74–1.10 P=.32 | OR 0.91; 95% CI 0.75–1.12 P=.38 | OR 0.85. 95% CI 0.57–1.27 P=.43 |
| Rollins,24 2018d ECA | 5971 | 21 | OR 1.16; 95% CI 0.96–1.39 P=.12 | OR 1.02; 95% CI 0.75–1.40 P=.90 | OR 0.99; 95% CI 0.74–1.34 P=.97 | OR 0.98. 95% CI 0.64–1.49 P=.59 |
| Rollins,24 2018e Observational | 13809 | 11 | OR 0.64; 95% CI 0.55–0.75 P<.0001 | OR=0.76; 95% CI 0.63–0.91 P=.003 | OR 0.86; 95% CI 0.64–1.15 P=.30 | OR 0.50; 95% CI 0.34–0.74 P=.0005 |
Summary of results from the metanalyses about mechanical colon preparation (MBP) showing its lack of effect in colon and rectal surgery. Two of them, in addition to randomized studies, include miscellaneous observational and cohort studies.23,24 Only observational studies show a reduction in SSI, anastomotic dehiscence and mortality with the use of MBP. All those comparisons are shown as MBP vs no MBP.
CI: confidence interval; OR: odds ratio.
Statistically significant results are in bold.
Although, in general, the meta-analyses conclude that MBP can be omitted in elective colorectal surgery, it should be noted that these reviews mix studies in which oral antibiotics were administered with MBP together with others in which they were not, so their conclusions can only be considered valid for MBP, not for oral antibiotics. In addition, the conclusions of the RCT and their meta-analyses seem to differ from those of the observational studies that have been published simultaneously. Two of the meta-analyses mentioned include observational studies in addition to RCT28,29 and reach less restrictive conclusions. In 2015,28 Dahabreh et al. classified their evidence as weak. They claim that a change in probabilities (e.g., 30%–50%) cannot be excluded in one way or another in the results due to the lack of information in most RCT, their small number of cases and the low number of events such as death, dehiscence, reoperation and severe SSI. They conclude that “modest beneficial or harmful effects of MBP cannot be excluded”. Oral antibiotics were used as an integral part of the MBP in only three of the studies. In an extensive meta-analysis from 2018, Rollins et al.29 “suggest” that MBP does not positively or negatively affect the incidence of complications. However, when they analyzed the subgroup of observational studies, those who received MBP had less SSI, anastomotic dehiscence, intra-abdominal collections and mortality than the non-prepared ones (Table 1).
The conclusions of the meta-analyses, coinciding in time with the start of the ERAS or Multimodal Rehabilitation programs in colorectal surgery,12,31,32 explain the gradual abandonment of MBP and, with it, oral antibiotic prophylaxis. The guidelines of the British National Institution of Health and Clinical Excellence33 and the ERAS Society (ERAS)34 do not recommend routine MBP for the reduction of SSI. However, the ERAS Society has issued a weak recommendation in favor of MBP in patients undergoing anterior resection of the rectum with provisional stoma.35
In the United States, several surveys specify the progressive reduction of the SSI rate from 88% in 1990,36 86.5% in 1997,37 75% in 200338 and 36% in 2010.39 In Spain, a 2005 survey shows that the use of MBP was 99% in rectal surgery, 90% in left colectomy and 60% in surgery of the right colon,40 percentages that decreased in a 2018 survey, with 95, 59 and 28% preparation rates, respectively (Badia et al., unpublished data).
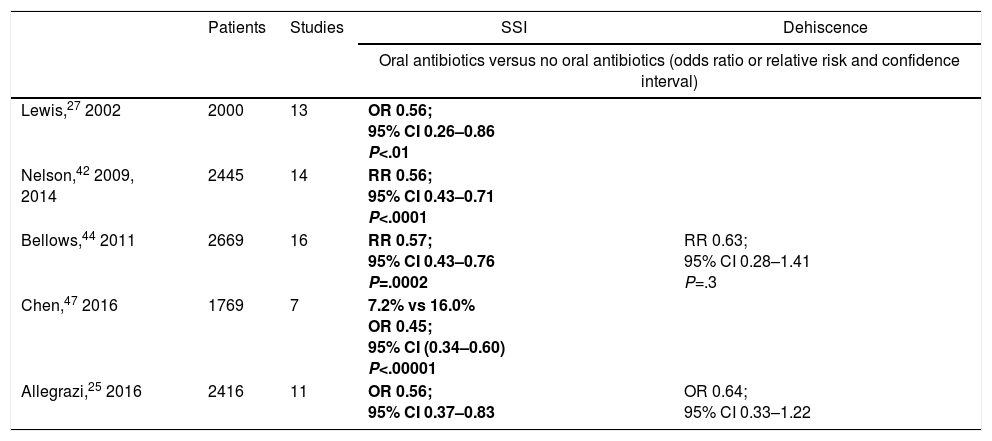
Oral AntibioticsRandomized controlled trials and meta-analyses comparing combined prophylaxis (oral antibiotic with MBP) against isolated MBP (Table 2). Interest in the effect of oral antibiotics combined with MBP re-emerged in 2002 with the publication of a randomized study and a meta-analysis.41 In the double-blind RCT, all patients received MBP along with intravenous prophylaxis. In the group of combined oral and systemic prophylaxis, a decrease in incisional infection (superficial and deep SSI) was observed (from 17 to 6%) with no significant differences in the rates of dehiscence or SSI-o/s. The bacterial content of the colon and the degree of contamination of the subcutaneous tissue was significantly higher in the isolated MBP group and correlated with the infection rate and infecting flora. The meta-analysis summarizes the evidence published in the previous 20 years and reveals a significantly lower rate of incisional infection with combined prophylaxis. The author concludes that combined oral and systemic antibiotic prophylaxis is superior to systemic prophylaxis alone for the prevention of postoperative infection and subtitles his article: “… a message since the 90s”.
Summary of the Results of the Metanalyses About the Utilization of Oral Antibiotics Combined with Mechanical Colon Preparation and Intravenous Prophylaxis in Colon and Rectal Surgery.
| Patients | Studies | SSI | Dehiscence | |
|---|---|---|---|---|
| Oral antibiotics versus no oral antibiotics (odds ratio or relative risk and confidence interval) | ||||
| Lewis,27 2002 | 2000 | 13 | OR 0.56; 95% CI 0.26–0.86 P<.01 | |
| Nelson,42 2009, 2014 | 2445 | 14 | RR 0.56; 95% CI 0.43–0.71 P<.0001 | |
| Bellows,44 2011 | 2669 | 16 | RR 0.57; 95% CI 0.43–0.76 P=.0002 | RR 0.63; 95% CI 0.28–1.41 P=.3 |
| Chen,47 2016 | 1769 | 7 | 7.2% vs 16.0% OR 0.45; 95% CI (0.34–0.60) P<.00001 | |
| Allegrazi,25 2016 | 2416 | 11 | OR 0.56; 95% CI 0.37–0.83 | OR 0.64; 95% CI 0.33–1.22 |
All show a reduction in SSI with the use of combined oral antibiotics and MBP. All the comparisons are shown as oral antibiotics versus no oral antibiotics. Statistically significant results are shown in bold.
Although the initial concept of oral prophylaxis was based on the administration of nonabsorbable antibiotics, this has not been maintained over time, given that some of them, such as erythromycin base, have been discontinued. Currently, some of the combinations used include absorbable antibiotics such as metronidazole or ciprofloxacin.
Since the Lewis study,41 several RCT have been published, some in favor of MBP with oral antibiotics42,43 and others against.44,45 However, the Cochrane reviews and the new meta-analyses that include them provide unanimous results in favor of combined prophylaxis.30,46–49
The Cochrane review by Nelson et al. in 2009,46 updated in 2014,49 compares systemic prophylaxis with combined systemic and oral prophylaxis. Its objective is the incisional infection rate of the abdominal wound, not contemplating SSI-o/e or anastomotic dehiscence. A benefit is shown in favor of combined prophylaxis. This review includes a comparison between combined prophylaxis and oral prophylaxis alone that also finds a clear superiority of combined prophylaxis and demonstrates again that systemic antibiotics should not be eliminated. The evidence obtained in the two comparisons is considered high-grade, implying that it is unlikely that future studies will change the results. The authors accept the dilemma of recommending combined prophylaxis when other Cochrane reviews recommend not performing MBP25 and point to the question of the efficacy of oral antibiotics in an unprepared colon.
Three meta-analyses between 2011 and 201630,48,50 compared the combination of intravenous and oral antibiotics with intravenous antibiotics in the presence of MBP. Patients assigned to combined oral and intravenous prophylaxis groups had a reduced risk of global and incisional SSI compared to those who received only intravenous antibiotics. In contrast, combined prophylaxis had no significant effect on SSI-o/e or the risk of suture dehiscence. They concluded that the combination of MBP with oral and systemic antibiotics significantly reduces SSI when compared to MBP associated only with systemic antibiotics.
It is worth mentioning an RCT51 comparing the efficacy of two groups or bundles of measures for the prevention of colorectal SSI. A bundle of six standard measures, which included MBP and oral prophylaxis, was compared with an “extended bundle” that omitted them. The group in which MBP was not performed with oral antibiotics almost doubled the global (45 vs 24%, P=.003) and incisional (36 vs 19%, P=.004) SSI rates.
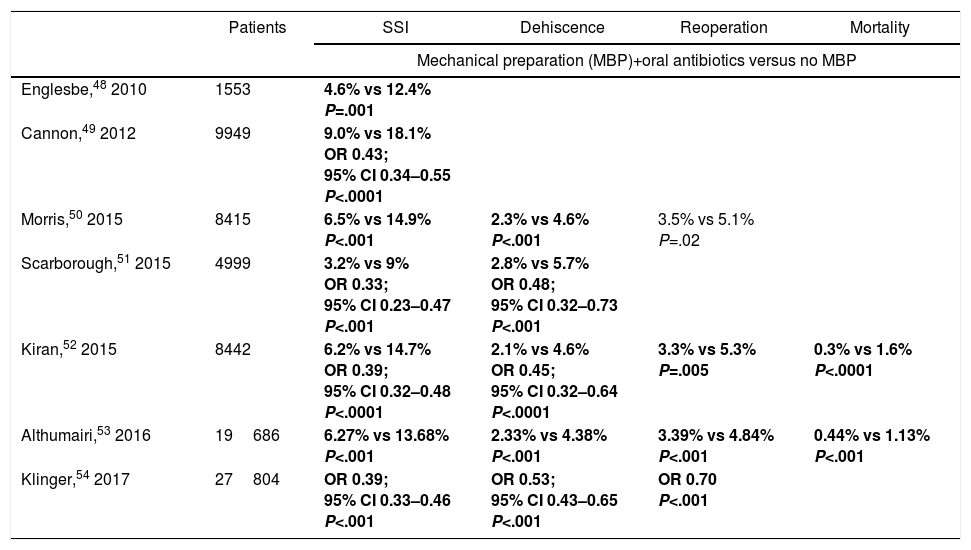
Observational studies comparing combined prophylaxis (oral antibiotic with MBP) versus absence of preparation (Table 3). In addition to RCT and meta-analyses, several observational studies have been published analyzing the effect of oral antibiotics using large North American population databases.52–58 Three of them showed an MBP utilization rate between 70 and 85%.52–54 All patients received systemic antibiotic prophylaxis. Patients who received oral antibiotics had less global SSI, incisional SSI and SSI-o/s. Additionally, with MBP associated with antibiotics, less prolonged postoperative ileus was observed.
Summary of Results of Observational Studies About the Use of Oral Antibiotics Combined with Mechanical Colon/Bowel Preparation (MBP) and Intravenous Prophylaxis in Colon and Rectal Surgery.
| Patients | SSI | Dehiscence | Reoperation | Mortality | |
|---|---|---|---|---|---|
| Mechanical preparation (MBP)+oral antibiotics versus no MBP | |||||
| Englesbe,48 2010 | 1553 | 4.6% vs 12.4% P=.001 | |||
| Cannon,49 2012 | 9949 | 9.0% vs 18.1% OR 0.43; 95% CI 0.34–0.55 P<.0001 | |||
| Morris,50 2015 | 8415 | 6.5% vs 14.9% P<.001 | 2.3% vs 4.6% P<.001 | 3.5% vs 5.1% P=.02 | |
| Scarborough,51 2015 | 4999 | 3.2% vs 9% OR 0.33; 95% CI 0.23–0.47 P<.001 | 2.8% vs 5.7% OR 0.48; 95% CI 0.32–0.73 P<.001 | ||
| Kiran,52 2015 | 8442 | 6.2% vs 14.7% OR 0.39; 95% CI 0.32–0.48 P<.0001 | 2.1% vs 4.6% OR 0.45; 95% CI 0.32–0.64 P<.0001 | 3.3% vs 5.3% P=.005 | 0.3% vs 1.6% P<.0001 |
| Althumairi,53 2016 | 19686 | 6.27% vs 13.68% P<.001 | 2.33% vs 4.38% P<.001 | 3.39% vs 4.84% P<.001 | 0.44% vs 1.13% P<.001 |
| Klinger,54 2017 | 27804 | OR 0.39; 95% CI 0.33–0.46 P<.001 | OR 0.53; 95% CI 0.43–0.65 P<.001 | OR 0.70 P<.001 | |
In the result, oral antibiotic prophylaxis combined with MBP reduces the rates of SSI, suture dehiscence, reoperations and mortality. All the comparisons are shown as MBP+oral antibiotics versus no MBP. Statistically significant results are shown in bold.
In one of the studies,53 no MBP was performed in 19.9% of colectomies, and a group of 7.3% received oral prophylaxis without MBP. No significant differences were found comparing MBP alone with no MBP (20 vs 18.1%, P=.08), confirming its null effect on SSI. However, the use of oral antibiotics (with or without MBP) reduced SSI significantly compared to the non-MBP group (9.0 vs 18.8%, P<.0001). Another of the studies included 62.9% of laparoscopic colectomies.54 According to the preparation received, the SSI figures were 14.9% in the group without MBP, 12% in the group of MBP and 6.5% in the group that received oral antibiotic. The infection rates of the oral antibiotic group combined with MBP and the isolated oral antibiotic group did not show significant differences (6.3 vs 9.4%, P=.09). When compared with the absence of preparation, the administration of oral prophylaxis (with or without MBP) showed a significant association with shorter hospital stay and lower percentages of readmissions, anastomotic dehiscence, postoperative ileus, reoperation and sepsis. In the multivariate analysis, the oral antibiotic was a protective factor against SSI (OR=0.46), an effect that was maintained in both open and laparoscopic surgery.
Since 2015, several studies have been published based on the database of the American College of Surgeons National Surgical Quality Improvement, all of them with a similar methodology, a large number of included colectomies and similar results.55–58 In general, significant differences were found in incisional SSI and anastomotic dehiscence rates when non-MBP was compared with MBP alone or oral antibiotic alone (Table 3). In contrast, the oral antibiotic group combined with MBP showed a reduction of incisional SSI and anastomotic dehiscence when compared to the absence of MBP. In the multivariate analysis by Kiran et al.,56 MBP with antibiotics (but not alone) was independently associated with a lower rate of anastomotic dehiscence, SSI and postoperative ileus. In Althumairi et al.,57 the univariate analysis also showed a lower incidence of sepsis, readmissions and reoperations in patients with MBP combined with oral antibiotics.
Only two of the most recent international guidelines for the prevention of SSI deal with the topic of oral antibiotics in colorectal surgery: the American IDSA/SHEA guidelines from 201459 and the WHO guidelines from 2016.30 Both agree to recommending them in combination with MBP.
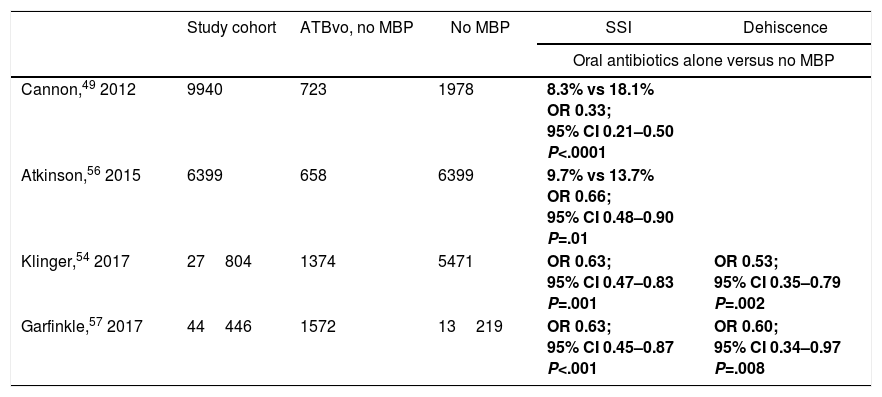
Oral Antibiotics With No MBPThe effect of oral antibiotics in the absence of MBP is not well defined due to the absence of RCT and the small number of patients with this preparation method in retrospective studies. However, some observational studies published in recent years53,58,60 provide clues that encourage us to explore this possibility (Table 4).
Summary of the Results from Observational Studies About the Use of Oral Antibiotics Without Mechanical Colon Preparation (MBP) in Colon and Rectal Surgery.
| Study cohort | ATBvo, no MBP | No MBP | SSI | Dehiscence | |
|---|---|---|---|---|---|
| Oral antibiotics alone versus no MBP | |||||
| Cannon,49 2012 | 9940 | 723 | 1978 | 8.3% vs 18.1% OR 0.33; 95% CI 0.21–0.50 P<.0001 | |
| Atkinson,56 2015 | 6399 | 658 | 6399 | 9.7% vs 13.7% OR 0.66; 95% CI 0.48–0.90 P=.01 | |
| Klinger,54 2017 | 27804 | 1374 | 5471 | OR 0.63; 95% CI 0.47–0.83 P=.001 | OR 0.53; 95% CI 0.35–0.79 P=.002 |
| Garfinkle,57 2017 | 44446 | 1572 | 13219 | OR 0.63; 95% CI 0.45–0.87 P<.001 | OR 0.60; 95% CI 0.34–0.97 P=.008 |
Even without MBP, the oral antibiotics reduce the rates of SSI and anastomotic dehiscence. All the comparisons are shown as oral antibiotics alone (ATBvo) versus no MBP. Statistically significant results are shown in bold.
In the analysis by Cannon et al.53 the patients who received oral antibiotics had a significantly lower SSI rate than the group without MBP. The use of oral antibiotics alone or combined with MBP decreased the incidence of SSI by 67 and 57%, respectively. These results would support the administration of oral antibiotics even in the absence of MBP.
In a similar study, Atkinson et al.60 analyzed patients undergoing colectomy without MBP, 658 of whom received oral antibiotics. The incidence of SSI was significantly lower in this group when compared to surgery without MBP or oral antibiotic. After controlling the results according to patient type and SSI risk factors, the administration of oral antibiotics achieved a significant reduction of the SSI. The authors concluded that, contrary to their initial hypothesis, the preoperative administration of oral antibiotics can reduce the SSI rate even when MBP is omitted.
An extensive matched cohort study61 found that oral antibiotic without MBP reduces SSI, anastomotic dehiscence, ileus and major complications, without the association of MBP improving these results. However, MBP combined with oral antibiotic also reduced mortality. In another large cohort,58 the group prepared only with oral antibiotics had less probability of SSI, SSI-o/s and dehiscence than those who were not prepared. However, when the MBP or oral antibiotic alone were compared with the combined preparation, the superiority of the combination of MBP and oral antibiotic was also observed, both in terms of SSI (OR 1.61, P=.002) and dehiscence (OR 1.60, P<.001).
It should be noted that studies suggesting the efficacy of oral antibiotics without MBP have important limitations, are retrospective, present results that cannot be adjusted according to the risk factors or type of preparation, and it is not possible to know under what criteria the oral antibiotic was indicated without MBP or the degree of compliance with the prescribed protocol. In addition, the databases on which they are based do not reflect the degree of compliance with systemic antibiotic prophylaxis and only follow patient during the first 30 days after surgery.
Risk for Pseudomembranous ColitisAn increased risk of pseudomembranous colitis due to Clostridium difficile (C. difficile) has been reported in MBP associated with antibiotics. In general, they are single-center studies with a low number of patients, such as that by Wren et al.,62 which finds a C. difficile infection rate of 7.4 vs 2.6%; P=.03). In contrast, in the 2014 Cochrane review, the risk of pseudomembranous colitis due to C. difficile seems low if oral and intravenous prophylaxis is limited to the preoperative dose.49
In addition, the cohort analyses show rates of C. difficile infection equal to preparation without antibiotics (1.3 vs 1.8%, P=.58)52 or even lower.58,63 The study by Klinger et al.58 showed that patients who received combined preparation had a lower probability of infection than those without preparation (OR 0.53, P=.035). A multicenter study of 24 hospitals also found a proportion of patients with less C. difficile infection in patients who had received oral antibiotics (1.6% vs 2.9%, P=.09).63
ConclusionsIsolated mechanical bowel preparation is not an effective measure to decrease the rate of infection. On the contrary, there is experimental evidence that correlates a significant reduction of the bacterial inoculum in the colon mucosa, peritoneal surface and subcutaneous fat with the use of oral antibiotic prophylaxis. The data generated by randomized studies, meta-analyses that group them and observational studies suggest that oral antibiotics combined with MBP play a crucial role in reducing the risk of superficial, deep and organ/space SSI as well as suture dehiscence, postoperative ileus, readmissions and mortality, without being associated with an increased risk of C. difficile infection.
The role of oral antibiotics in the absence of MBP has only been analyzed in the framework of observational studies. The results of randomized prospective studies that are currently underway, which analyze the effect of oral antibiotics without mechanical preparation, can yield valuable information in this regard. In the meantime, the practice of elective colorectal surgery without adequate colon preparation including oral antibiotic prophylaxis seems hardly justifiable, as this strategy should be considered, for the time being, the gold standard for the prevention of SSI in this type of surgery.
Conflict of InterestThe authors have no conflict of interests to declare.
Please cite this article as: Badia JM, Arroyo-García N. Preparación mecánica y profilaxis antibiótica por vía oral en cirugía colorrectal. Análisis de la evidencia científica y revisión narrativa. Cir Esp. 2018;96:317–325.