Salmonella are Gram-negative bacilli classified as enterobacteriae that are present worldwide and are a part of the intestinal flora of humans and other animals.1 They are usually non-pathogenic, but in certain situations can become pathogenic and cause a wide variety of diseases in humans.
An example of the infections caused by Salmonella sp. are the extraintestinal manifestations, that are classified into 4 types: primary bacteriemia (PB), enteritis associated with bacteraemia or secondary bacteraemia (SB), focal digestive infection (FDI) and non-focal digestive infection (NFDI).2
Excluding the digestive tract, the most common locations of intraabdominal infection caused by these microorganisms are the spleen in the form of abscesses and the gallbladder as acute cholecystitis. Other less frequent locations are liver abscesses, pancreas, adrenal glands and subphrenic abscesses. Peritonitis caused by Salmonella sp. is extremely rare.
The most important predisposing factors for infection by this microorganism are immunodeficiency or chronic diseases such as diabetes, chronic renal failure, falciform anaemia, alcoholism and the use of immunosuppressive drugs.6 These factors predispose for a primary bacteriemia2–5 with subsequent dissemination of the microorganism.
A 41-year-old man came to the Emergency Department for abdominal pain, nausea and bilious vomiting of 24h duration after and excess of alcohol intake.
He had a prior history of dyslipidemia with elevated triglyceride counts, smoking, and chronic alcohol abuse. Three years prior he had been hospitalised for acute severe pancreatitis with an intraabdominal abscess and a second episode of hospitalization a year and a half later in the intensive care unit for severe acute pancreatitis of the neck and tail. He was diagnosed with a pancreatic pseudocyst and hepatic esteatosis in a control CT.
On admittance he was hemodynamically stable with a temperature of 37.3°C. An emergency CT scan was performed that showed a rupture of the pancreatic pseudocyst into the gastric wall. He was admitted to the Department of Gastroenterology.
In the next few days he needed transfer to the Intensive care Unit due to haemodynamic instability, T 35°C, and important abdominal distension and peritoneal irritation. Blood test revealed leucopenia, altered coagulation tests and acute renal failure. Antibiotics were started a new CT was performed, that showed the appearance of free peri-splenic and peri-hepatic fluid.
With the suspected diagnosis of intraabdominal infection, emergency surgery was indicated. During surgery, acute diffuse purulent peritonitis with fibrin was observed, mostly in the supramesocolic space, with the gastric fundus sealed on the pancreatic surface. A lavage was performed and an abdominal VAC® system was implanted due to the peritonitis. Intraabdominal cultures and blood cultures were positive for group D Salmonella.
During the next few days the patient’ clinical condition deteriorated and mechanical ventilation was necessary. The antibiotic spectrum was broadened and antifungal therapy was added. Serologies for HIV, HB, HC and sifilis were negative.
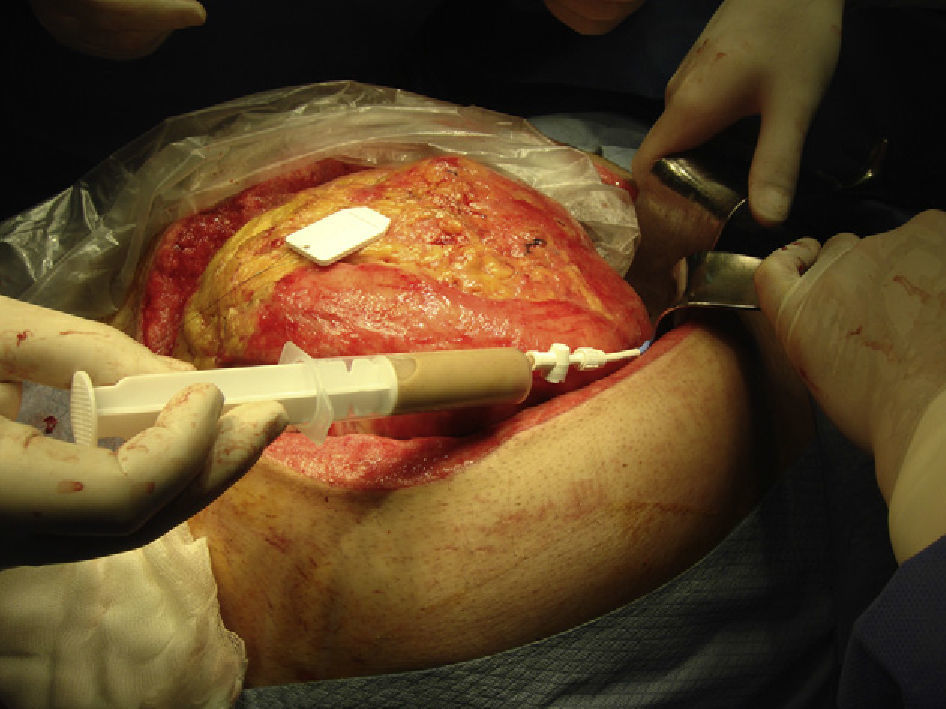
The patient was taken to the operating room in seven occasions to change the VAC® system and perform intraabdominal lavage. In the fourth operation the pseudocyst was located using US and a transgastric drain was performed (Fig. 1). The fluid was cultured and group B Salmonella was isolated. In the next operations the abdomen was progressively closed.
After drainage of the pseudocyst the patient presented a favourable clinical course and was transferred to a regular nursing floor with a final hospital discharge one month and a half after admittance.
Many infectious complications caused by Salmonella have been well described in the literature, but others are less well known and uncommon such as pancreatic abscesses or diffuse peritonitis caused by this microorganism.3,4
This type of infections usually affects patients with immunodeficiency or another predisposing factor for colonization and maintenance of these bacteria in the organism, such as chronic alcoholism.8
Most of the infectious manifestations resolve with the use of appropriate antibiotics, but in some occasions, and especially when the infection is localized and creates abscesses, we believe that the use of surgical manoeuvres is essential for the proper eradication of the pathogen.7
Please cite this article as: Freiría Eiras MÁ, López Saco Á, Gil Gil P. Peritonitis intestinal por Salmonella no tífica. Cir Esp. 2013;94:265–266.
This case was accepted as an oral presentation in the LIV Meeting of the Sociedad de Cirugía de Galicia in Ferrol, 26 and 27 November 2010.