Minimally invasive radioguided parathyroidectomy (MIRP)1,2 has been implemented at the Hospital Universitario de Navarra as part of a Prospective Research Project, authorized by the Ethics Committee (October 2019), with the aim of improving our previous success rate in selective parathyroidectomy (94.6%)3.
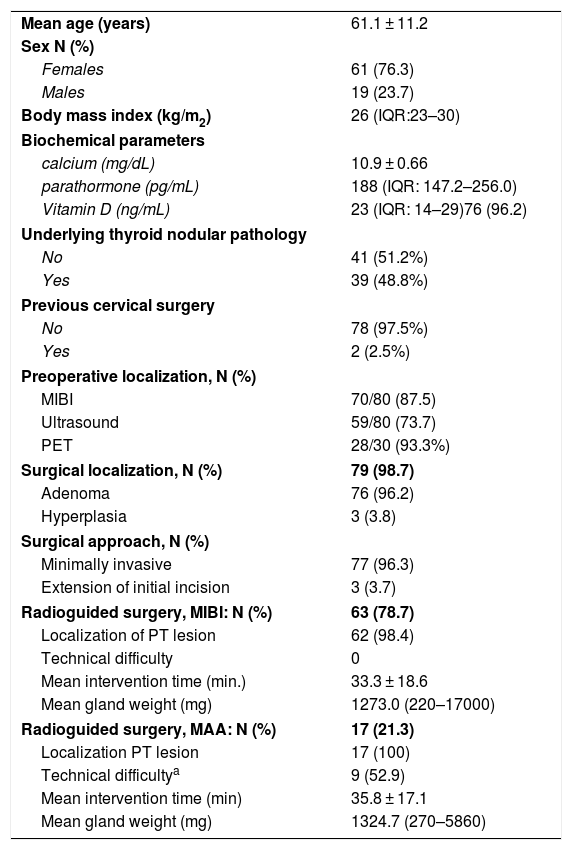
Since its initial implementation in February 2020 and until December 2021, we have performed MIRP (with MIBI or MAA)2 consecutively on all patients with primary hyperparathyroidism and an indication of minimally invasive parathyroidectomy (80). Mean age was 61.1 years (±11.2), and 61 patients were women (76.3%). Clinical and analytical data are shown in Table 1.
Patients with indication for MIRP. Results.
| Mean age (years) | 61.1 ± 11.2 |
| Sex N (%) | |
| Females | 61 (76.3) |
| Males | 19 (23.7) |
| Body mass index (kg/m2) | 26 (IQR:23–30) |
| Biochemical parameters | |
| calcium (mg/dL) | 10.9 ± 0.66 |
| parathormone (pg/mL) | 188 (IQR: 147.2–256.0) |
| Vitamin D (ng/mL) | 23 (IQR: 14–29)76 (96.2) |
| Underlying thyroid nodular pathology | |
| No | 41 (51.2%) |
| Yes | 39 (48.8%) |
| Previous cervical surgery | |
| No | 78 (97.5%) |
| Yes | 2 (2.5%) |
| Preoperative localization, N (%) | |
| MIBI | 70/80 (87.5) |
| Ultrasound | 59/80 (73.7) |
| PET | 28/30 (93.3%) |
| Surgical localization, N (%) | 79 (98.7) |
| Adenoma | 76 (96.2) |
| Hyperplasia | 3 (3.8) |
| Surgical approach, N (%) | |
| Minimally invasive | 77 (96.3) |
| Extension of initial incision | 3 (3.7) |
| Radioguided surgery, MIBI: N (%) | 63 (78.7) |
| Localization of PT lesion | 62 (98.4) |
| Technical difficulty | 0 |
| Mean intervention time (min.) | 33.3 ± 18.6 |
| Mean gland weight (mg) | 1273.0 (220–17000) |
| Radioguided surgery, MAA: N (%) | 17 (21.3) |
| Localization PT lesion | 17 (100) |
| Technical difficultya | 9 (52.9) |
| Mean intervention time (min) | 35.8 ± 17.1 |
| Mean gland weight (mg) | 1324.7 (270–5860) |
We performed MIRP-MIBI after intravenous administration of 5 mCi 99mTc-MIBI, with immediate scintigraphy study and radioguided surgical procedure approximately 60 minutes later. To perform MIRP-MAA, 0.5 mCi of intralesional 99mTc-macroaggregated albumin is administered under ultrasound guidance on the same day of the intervention, with subsequent scintigraphic acquisition (SPECT/CT). Intraoperatively, we use a Neo2000® (Neoprobe Corporation, Dublin, EE.UU.) gamma probe (9 mm head) and a Sentinella® portable gamma camera (Oncovision, Valencia, Spain).
The preoperative MIBI-SPECT/CT and ultrasound diagnostic studies had identified the pathological gland in 70 (87.5%) and 59 (73.7%) patients, respectively, the rest being negative or inconclusive (Table 1). In the 30 cases (37.5%) in which one of the tests was negative or not totally concordant, choline and/or methionine PET were performed, which were diagnostic in 28 (93.3%).
Radioguided surgery was minimally invasive in 77 patients (96.3%), including the two with a history of cervical surgery (one total thyroidectomy, one previous failed selective parathyroidectomy). Three (3.7%) required extension of the initial incision: 2 due to involvement of two contralateral glands, one due to the posterior ectopic location of the adenoma.
Surgical resection of the lesion was achieved in 79 patients (98.7%), 76 (96.2%) of which were adenomas and 3 (3.8%) hyperplasia (Table 1). Two presented double lesions: one adenoma, one hyperplasia. Mild surgical complications were recorded in 4 (5%): one small self-resolving subcutaneous hematoma, two transient hypocalcemia, and one vocal cord paresis.
According to the previous evaluation of the localization study4, we indicated MIRP-MAA in 18 patients (Table 1) and performed it in 17 (in one patient, scintigraphy showed extensive skin contamination due to radiotracer leakage during ultrasound inoculation, invalidating the procedure). Since the parathyroid lesion was MIBI-positive, MIBI was then injected and finally excised. The lesion marked with MAA was resected in the remaining 17, and the mean surgical procedure time was 35.8 min. In 9 patients, we observed significant residual uptake in the surgical bed after resection of the radiolabeled gland (dispersion of the radiotracer to the thyroid or pre-thyroid muscles during its administration). In one, scintigraphy also demonstrated abnormal localization of MAA in the lungs (partial intravascular administration – innocuous); in another, a discreet post-injection subcutaneous hematoma, which resolved itself.
MIRP-MIBI was performed in 63 patients (Table 1), confirming resection of the parathyroid lesion in 62 (98.4%). In the only ‘failed’ surgery, a weakly MIBI-positive lesion was removed, which was macroscopically suggestive of parathyroid; however, the histopathology results identified it as an adenopathy, which can uptake MIBI on occasion5. The mean time between MIBI administration and the start of the procedure was 90 min. The mean duration of the MIRP-MIBI was 33.3 min, shorter than the MAA (not significant, p = .349). There were also no significant differences in the size of the excised lesion (p = .504).
In total, 22 ectopic adenomas (27.5%) were resected using MIRP-MIBI: 9 paraesophageal, 7 mediastinal, 3 pretracheal, 2 prevertebral, and 1 intrathymic.
During the 6-month follow-up, the only MIRP in which a pathological parathyroid gland was not demonstrated histopathologically presented biochemical cure, which is an exceptional clinical circumstance6. Two presented persistent hypercalcemia, despite resection of an adenoma; one was recently and successfully reoperated on (Fig. 1) after finding a new parathyroid lesion (MIBI and PET-positive). The provisional cure rate was 97.5%.
Patient with PHPT who underwent resection of a parathyroid adenoma (yellow arrow) located posterior to the caudal pole of the left thyroid lobe (A) by means of MIRP after ultrasound-guided administration of 99mTc-MAA. The transaxial fusion SPECT/CT image shows the correct intralesional location of the radiotracer (B). Hypercalcemia persisted one year later, and a new parathyroid lesion was observed (C) in a more caudal right paraesophageal ectopic location (red arrow) with significant uptake of 99mTc-MIBI as shown in the SPECT/CT fusion image, (D) which was satisfactorily removed in a second surgery, this time radioguided with MIBI.
MIRP-MIBI requires strict coordination between the nuclear medicine unit and the operating room, which has been satisfactory in our setting. However, the time between injection and start of surgery exceeded the initially set objective due to intra-hospital patient transfers. The physiological fixation of MIBI in nearby tissues (thyroid, muscle), can make surgical detection difficult, especially in the case of parathyroid glands with low intensity of uptake7 and/or ‘rapid washout’ (preoperative study). Thus, the intraoperative image (portable gamma camera) is very useful, as it minimizes this drawback and confirms excision of the lesion.
MIRP-MIBI allows for minimally invasive resection of ectopic lesions8.
Although the surgical procedure with MAA is, in principle, technically simpler, difficulties in ultrasound-guided intralesional administration are not uncommon, probably due to the depth and small size of the lesions and/or the learning curve.
In conclusion, we have implemented MIRP with both MIBI and MAA at our hospital, and these interventions have developed smoothly thanks to the close collaboration of the professionals involved. The surgical team finds the MIRP to be easier. We believe that the method used is reproducible in any Endocrine Surgery Unit. Although the number of cases and follow-up are limited (including most interventions in the last few months, due to the interruption of surgical activity as a result of the pandemic from March-September 2020), the favorable results allow us to dispense with the intraoperative histological study. Nonetheless, the inclusion of more patients will determine the impact on surgical success and cure rate, as well as the duration of the intervention and the rate of complications.
FinancingThis research has not received specific aid from agencies of the public sector, commercial sector or Non-profit entities.
Conflict of interestsThis study has received no specific funding from public, commercial or non-profit entities.