Despite its high prevalence, faecal incontinence (FI) is still underrated and underdiagnosed. Moreover, diagnosis and subsequent treatment can be a challenge for the colorectal surgeon because of its associated social taboo and embarrassment, and the wide range of symptoms. The aim of the present study is to describe a new high-resolution circuit (HRC) for FI diagnosis, that was implemented at our centre and to evaluate patient satisfaction.
MethodsThe structure and organisation of the HRC are described. Demographic and clinical data of the patients included in the HRC between February 2014 and June 2016 were collected. Moreover, patients’ satisfaction was measured through a structured survey.
ResultsA total of 321 patients were evaluated in our pelvic floor outpatients clinic during the study period: 65% (210) of them had FI (81% women, median age 66 years). The mean time since FI onset was 24 (range 4–540) months. A total of 79% (165) of the patients were included in the HRC. 62% of them responded to the survey. Of these, only 32% (33) had consulted for FI before coming to our centre. The majority, 88% (90) considered that performing the 2diagnostic tests the same day of the visit was a very good option. And 94% (96) were satisfied with the information received on their FI, with a median satisfaction value of 10 (5–10).
ConclusionWith the HRC, the patient spends about 2h in the outpatient clinic of the hospital, but leaves with the complete diagnostic process performed. The satisfaction survey confirms that most patients prefer this system.
La incontinencia fecal (IF), pese a su elevada prevalencia, sigue estando infravalorada e infradiagnosticada. La potencial afectación psicológica, el tabú asociado y el amplio abanico de síntomas hacen del diagnóstico y tratamiento un reto para el cirujano colorrectal. El objetivo de este estudio es describir un nuevo circuito de atención especializado, el circuito de alta resolución (CAR) para tratar la IF, y evaluar la satisfacción de los pacientes.
MétodosSe realiza una descripción de la organización del CAR. Se analizan los datos demográficos y clínicos de los pacientes incluidos en el CAR entre febrero de 2014 y junio de 2016. Se reportan, además, los resultados de una encuesta de satisfacción sobre el CAR realizada a los pacientes incluidos.
ResultadosDurante el periodo de estudio se realizaron 321 primeras visitas: 65% (210) por IF (81% mujeres; mediana de edad 66 años). El tiempo mediano de evolución de la IF fue de 24 (rango 4-540) meses. El 79% de los pacientes (165) realizaron el CAR. El 62% respondieron a la encuesta. De estos, solo un 32% (33) habían consultado por este problema en otros centros. La mayoría, 88% (90) consideró preferible el hecho de que hicieran las pruebas diagnósticas el mismo día de la visita. El 94% (96) quedó satisfecho con la información recibida sobre la IF, valorando la consulta con una mediana de 10 (5-10) sobre 10.
ConclusiónCon el CAR, el paciente pasa alrededor de 2 h en las consultas externas del hospital, completando el proceso diagnóstico en el mismo día. Los resultados de satisfacción confirman que los pacientes en su mayoría prefieren este sistema.
Until a few decades ago, there was no effective treatment for faecal incontinence (FI) except for surgical repair in cases of sphincter lesions.
In the last 20 years, there has been growing interest in treating these patients, which has led to a greater understanding of what occurs when a patient is not able to properly control faeces as well as the development of new imaging tests, study tools and therapeutic procedures.
In spite of this, the problem continues to be underestimated and underdiagnosed: some physicians are unaware of the therapeutic options, the patients themselves do not know where they should ask for help, and many medical institutions do not support or even contemplate this problem, in spite of its high prevalence.
The reported incidence is variable depending on several factors and the definition of FI,1 but a local study has concluded that it might affect 10.8% of the adult population,2 which is an incidence similar to diabetes mellitus.
The effect on the quality of life in patients with FI is comparable to that of patients with inflammatory bowel disease and surpasses that of other chronic patients, such as those with rheumatoid arthritis. It increases proportionately as the severity of the symptoms increases, especially in the social and emotional domains.3 Furthermore, it has been demonstrated that chronic alterations in quality of life can involve irreversible deficits, essentially in the social dimensions.
The diagnostic-therapeutic delay in patients with FI is multifactorial, but undoubtedly one of the reasons lies in the healthcare system diagnostic circuits. Some studies indicate that the average time between the onset of the problem until the patient receives care is 55 months (9–360).4 In the specialised healthcare system in Catalonia, the standard circuit consists of an initial visit to the hospital after having been referred from the primary care setting and several months on a waiting list, depending on the hospital. At this initial office visit, at which the specialist has 10min to assess the patient, a series of complementary tests is usually ordered, which may take several months more to complete at most hospitals.
The primary objective of this study is to describe a new specialised care programme, the “high-resolution circuit” (HRC), for defecation disorders and to describe the series of patients included. The secondary objective was to evaluate the satisfaction of the patients treated in this circuit.
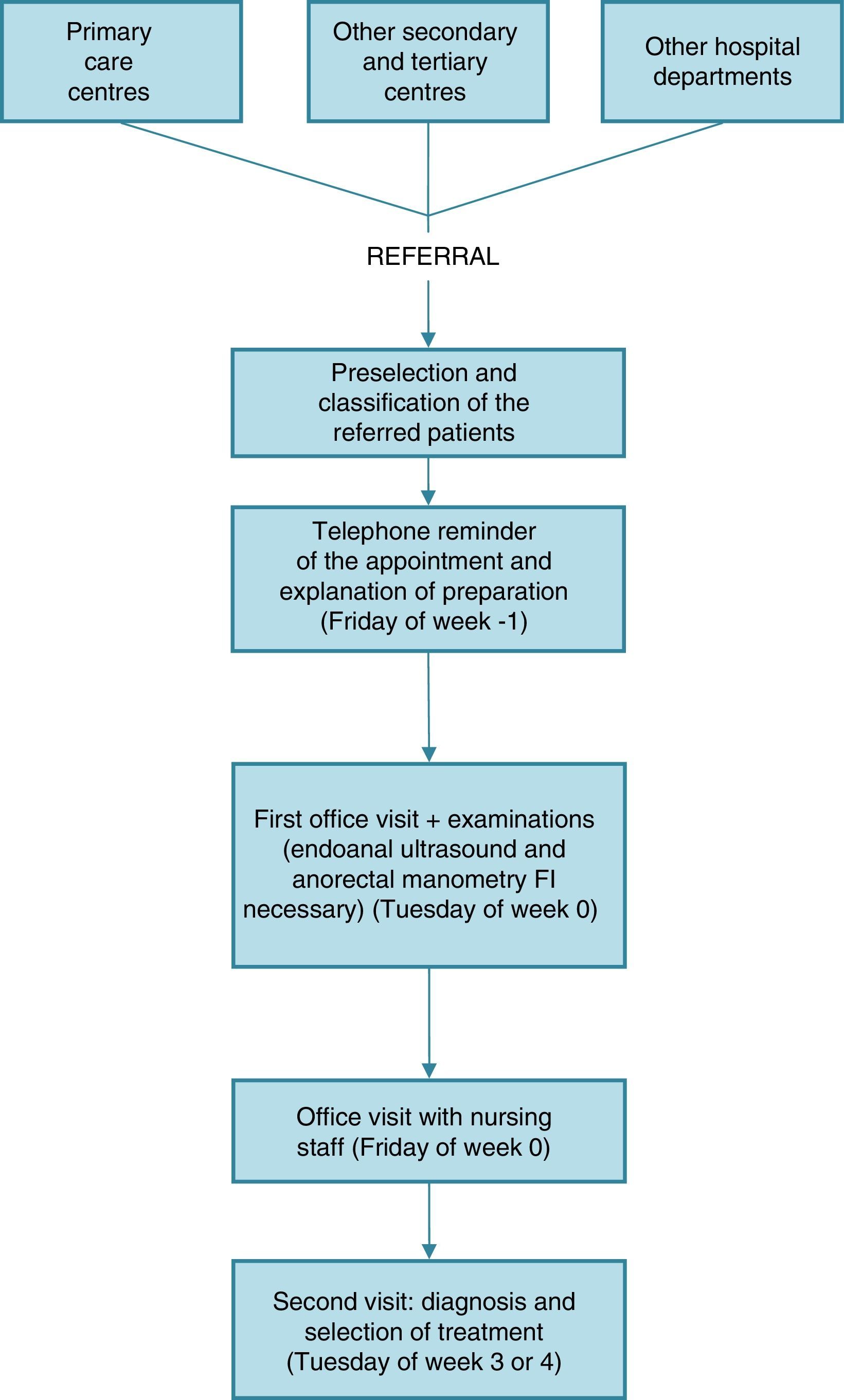
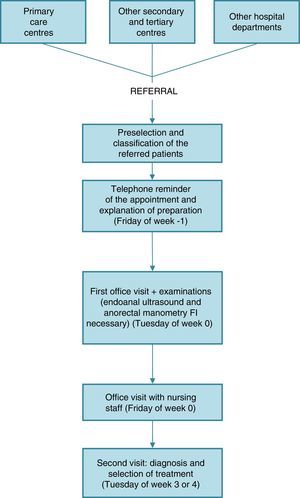
MethodsThe HRC involves an initial office visit for all patients with defection dysfunctions of between 30 and 45min, at which time the surgeon takes a detailed patient medical history and examines the patient as part of the protocol. In patients with FI, the HRC is completed with endoanal ultrasound and anorectal manometry that same morning.
That same week, the patient has a visit with specialised nursing staff for approximately 45min, at which time dietary and hygiene habits are discussed; the nurse addresses any doubts the patient may have and explains any possible aggravating factors of the condition. This visit is not scheduled for the same day because we feel it is important for the patient to have a few days after the appointment with the surgeon to be able to identify any doubts that he/she may have.
In order to optimise patient attendance, auxiliary nursing staff contacts the patients the previous Friday to remind them of their appointment and to explain how they should use an enema beforehand. At that time, patients confirm their intended assistance, with the aim to have as few “no-shows” as possible (Fig. 1).
The anamnesis is systematised and the history of pathological, surgical and obstetrical data is recorded along with any medications currently being taken. In order to better understand the characteristics of the incontinence, the patient is asked about defecation habits, urgency, soiling or passive incontinence. The St. Mark's scale5 is completed as well as a subjective assessment of the patient's condition (visual analogue scale from 0 to 10, with 10 as the best score). The examination includes inspection of defects in the perianal area, evaluation of superficial anal reflex, Valsalva manoeuvre and digital rectal examination. The results of the evaluations are collected in a discreet, qualitative manner.
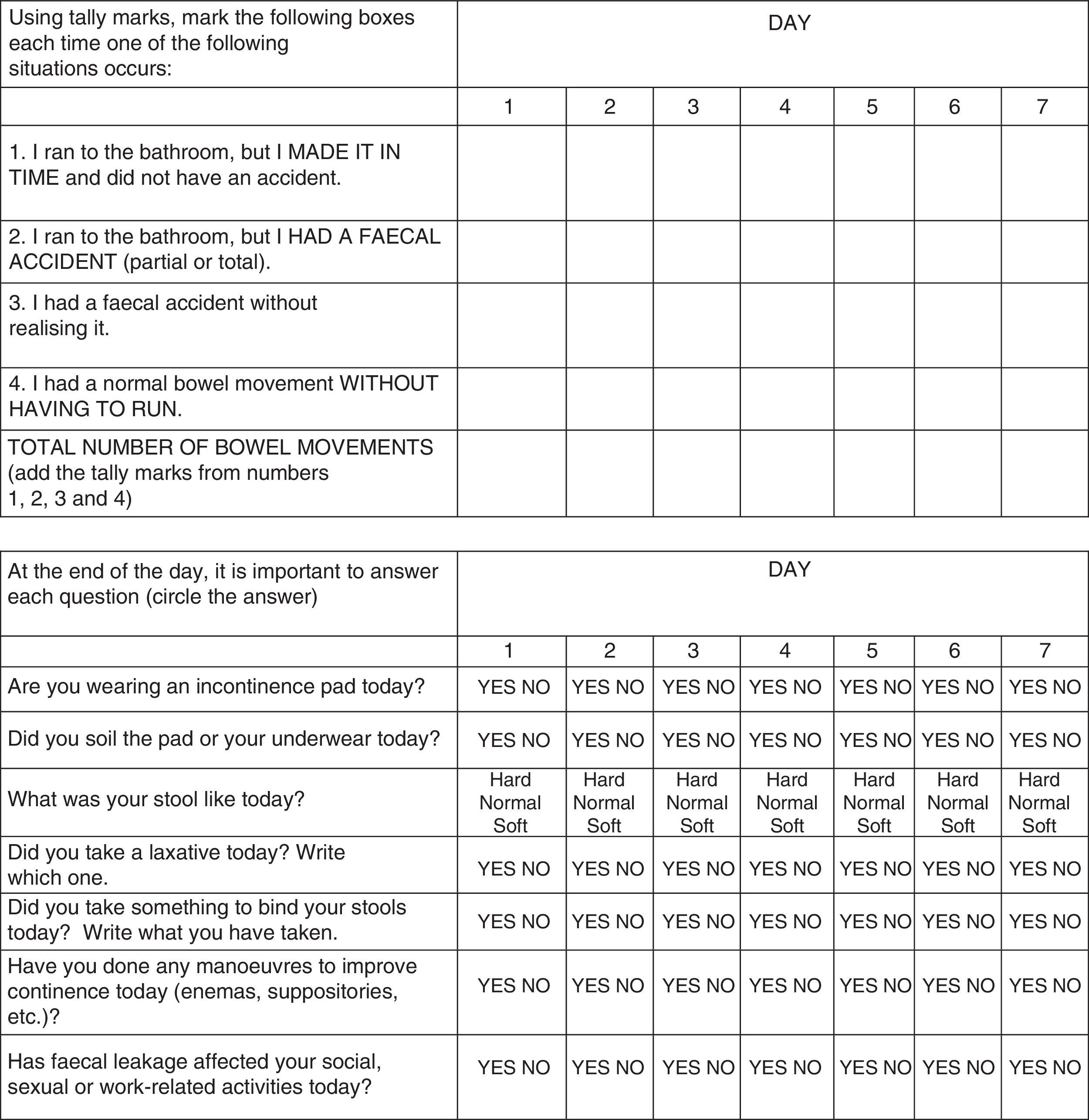
It is important for the patient to understand that he/she must collaborate in the diagnostic process by keeping a 3-week defecation diary developed at our hospital, which consists of 2 main parts: a quantitative part, where each defecation is noted as a single option; and the qualitative part, which records complementary variables (Fig. 2). In addition, the assessment is completed with a specific quality-of-life test for FI (FIQOL).3 Finally, we explain the other complementary examinations that the patients will undergo.
The first office visit should not conclude without explaining to the patient that we can help him/her and that there are appropriate therapeutic tools available. Some initial treatment measures should also be taken.
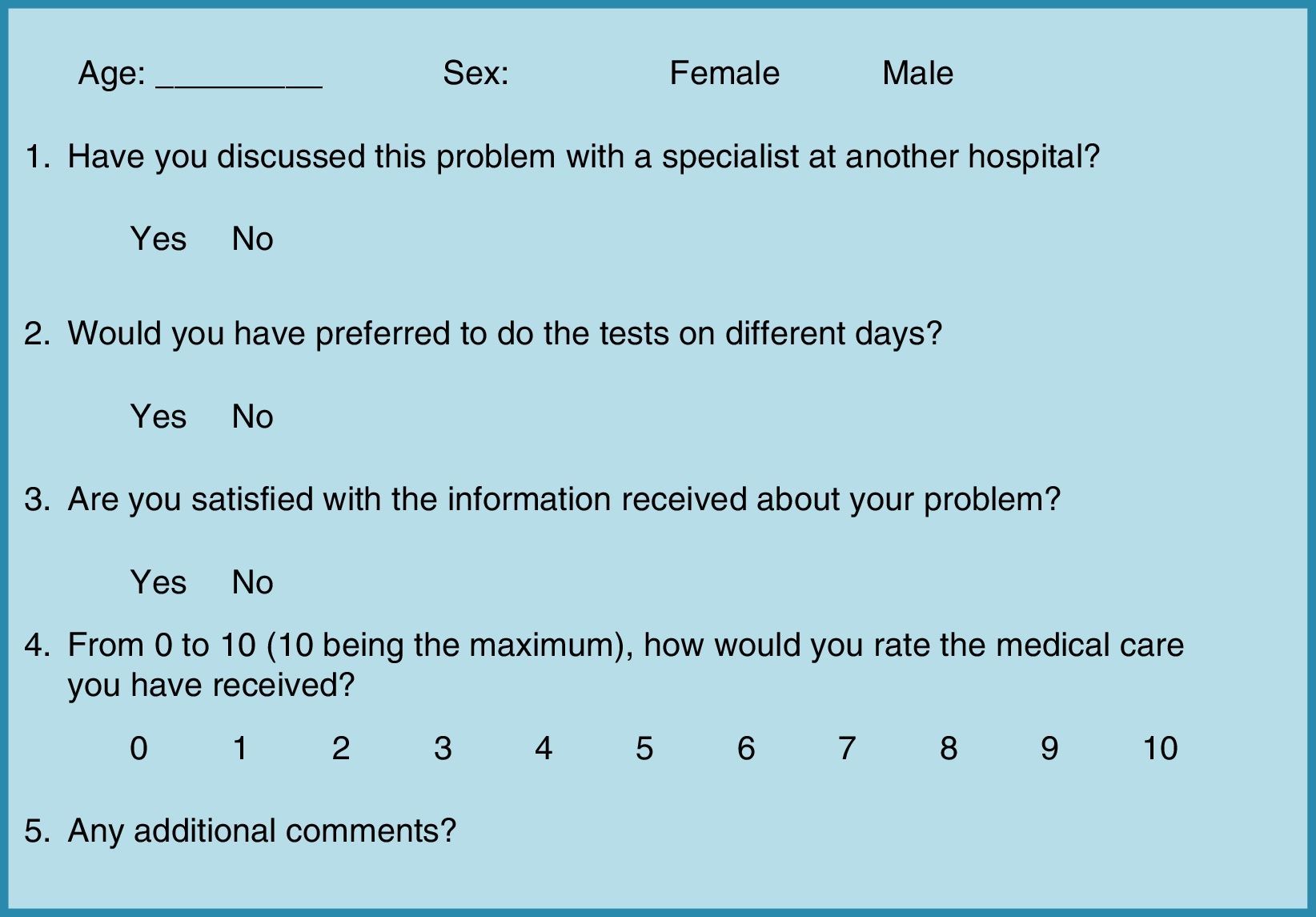
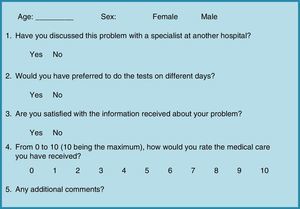
Patient satisfaction with the HRC was surveyed with a structured questionnaire (Fig. 3). This evaluation was retrospectively applied to patients treated between February 2014 and December 2015 by means of a telephone interview. Patients treated between January and June 2016 were given a written survey to be filled out in the waiting room once the HRC had been completed.
The satisfaction survey of this circuit was approved by the Ethics Committee of our hospital. Patients gave their written informed consent to enter the study and for use of their data.
ResultsBetween February 2014 and June 2016, 321 initial office visits were scheduled in the Pelvic Floor Unit. Diagnoses included: incontinence 65% (210), constipation 16% (52), prolapse 3% (8), chronic perineal pain 3% (10), and others 13% (41).
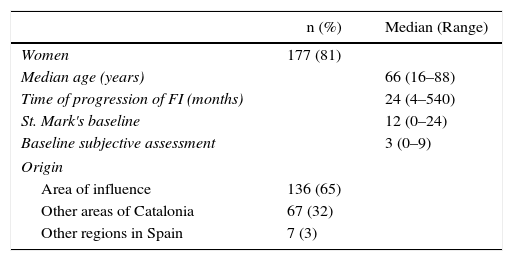
The patients diagnosed with incontinence (81% women; mean age 66 [range 16–88]) came from our area of influence (65%; n=136) as well as other hospitals in Catalonia (32%; n=67) and other regions of Spain (3%; n=7). The rate of absences at this office visit (no-shows for scheduled appointments) was 5%.
At baseline, patients with incontinence (n=210) had a mean score on the St. Mark's scale of 12 (range 0–24) and a mean subjective quality-of-life score of 3 (range 0–9) out of 10. The mean progression time of the incontinence prior to the consultation was 24 months (range 4–540) (Table 1).
Baseline Characteristics of the Patients With Faecal Incontinence (n=210).
| n (%) | Median (Range) | |
|---|---|---|
| Women | 177 (81) | |
| Median age (years) | 66 (16–88) | |
| Time of progression of FI (months) | 24 (4–540) | |
| St. Mark's baseline | 12 (0–24) | |
| Baseline subjective assessment | 3 (0–9) | |
| Origin | ||
| Area of influence | 136 (65) | |
| Other areas of Catalonia | 67 (32) | |
| Other regions in Spain | 7 (3) | |
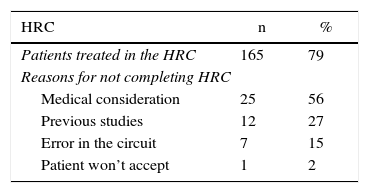
79% of these patients (165) were included in the HRC. The reasons for exclusion were: medical reasons (56%, n=25), already had a complete study (27%, n=12), patient did not accept testing (2%, n=1) or error in the circuit (15%, n=7).
Out of the patients evaluated between February 2014 and December 2015 (241 first visits, 67% of them due to incontinence), 105 patients were contacted by telephone, and 69 (66%) answered. The reasons for not contacting the rest of the patients were: having a low cognitive level (n=4) or being over the age of 75 (n=13) (Table 2). Starting in February 2016, the written survey was given to 33 patients (77%) with incontinence who were included in the HRC during this period.
Variables of the High-Resolution Circuit and Satisfaction Survey (n=210).
| HRC | n | % |
|---|---|---|
| Patients treated in the HRC | 165 | 79 |
| Reasons for not completing HRC | ||
| Medical consideration | 25 | 56 |
| Previous studies | 12 | 27 |
| Error in the circuit | 7 | 15 |
| Patient won’t accept | 1 | 2 |
| Telephone Survey (February 2014–December 2015) | ||
|---|---|---|
| Patients called | 105 | 86 |
| No answer | 36 | 34 |
| Answer | 69 | 66 |
| Patients not called | 17 | 14 |
| Older than 75 | 13 | |
| Low cognitive level | 4 | |
| In-Person Survey (January–June 2016) | ||
|---|---|---|
| Answered the survey | 33 | 77 |
| Did not answer the survey | 10 | 23 |
| Total patients who responded | 102 | 62 |
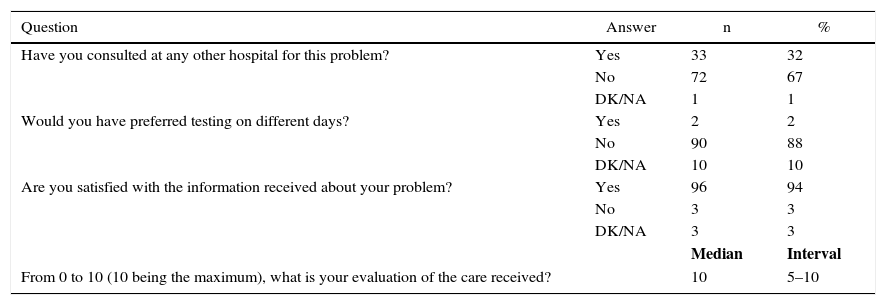
In total, 62% of the patients (102) with FI who completed the HRC answered the survey. Out of these, only 32% (33) had consulted about this problem at other medical centres. The majority (88%, 90 patients) considered it preferable to have the diagnostic tests done the same day of the visit. 94% (96) were satisfied with the information received about FI and gave the consultation an average of 10 points (range 5–10) out of 10 (Table 3).
Responses to the High-Resolution Circuit Satisfaction Survey (n=102).
| Question | Answer | n | % |
|---|---|---|---|
| Have you consulted at any other hospital for this problem? | Yes | 33 | 32 |
| No | 72 | 67 | |
| DK/NA | 1 | 1 | |
| Would you have preferred testing on different days? | Yes | 2 | 2 |
| No | 90 | 88 | |
| DK/NA | 10 | 10 | |
| Are you satisfied with the information received about your problem? | Yes | 96 | 94 |
| No | 3 | 3 | |
| DK/NA | 3 | 3 | |
| Median | Interval | ||
| From 0 to 10 (10 being the maximum), what is your evaluation of the care received? | 10 | 5–10 |
DK/NA: Don’t know/No answer.
Patients with defecation problems usually present with greatly varying symptoms. The potential psychological effect (embarrassment and the taboo associated with this condition), as well as the limited medical attention that the patients had received before arriving at our consultations, mean that diagnosis and later treatment can pose a challenge for colorectal surgeons. Because of these circumstances, the time spent with each patient at the initial consultation should not be strictly limited.
In patients with FI, the diagnostic process should be empathetic and provide sufficient time for a detailed anamnesis and meticulous physical examination. Likewise, one must be very rigorous in the collection of information in order to draw effective conclusions.
The design of this type of care in an organised high-resolution circuit entails a considerable increase in office visit times to 1h 15min, including consultation, examination, ultrasound and anorectal manometry. With HRC, the patient spends about 2h in the outpatient clinic of the hospital, but leaves after a completed diagnostic process. The satisfaction survey confirms that most patients prefer this system.
Given that considerable time is spent on HRC visits, administrative organisation is essential. This requires calling patients a few days in advance to confirm their assistance and thereby have the lowest number of no-shows possible. In our first experience using this measure, there were only 5% absences.
The establishment of this type of treatment tracks involves many advantages: the patient has fewer visits to the hospital, he/she prepares for examinations only once, and the waiting time for a final diagnosis is shorter. Moreover, the physician who has just taken the anamnesis can take greater advantage of the examination carried out during the same consultation.
However, other measures that improve the circuit should be incorporated to avoid spending healthcare resources on patients who do not need them. In our experience, 12% (25/210) of patients scheduled for the HRC did not complete the circuit in the end because the specialist did not consider the patient a candidate for complementary testing. With the training of primary care physicians in hygienic-dietary management or, in some cases, pharmacological treatment of FI, this aspect could be improved.
Another way to improve the circuit is through increased participation of skilled nursing staff in defecation disorders. In some European medical centres, patients are first seen by nursing staff, except for those patients who are direct candidates for surgical treatment. Patients are referred to colorectal surgeons only if the conservative treatment offered (diet, medication, biofeedback) is not effective. According to the experience of hospitals with large patient volumes, up to 40% of patients can be managed from the nursing consultation.6 In a second phase, our thought is to improve the HRC by incorporating an initial consultation with nursing staff before the appointment with the surgeon in a select group of patients. This improvement in the circuit may lead to significant savings in complementary tests, as patients responding to conservative treatment will no longer enter the testing circuit.
The establishment of an HRC reduces the time in which the patient's diagnosis is made and treatment is initiated. However, it does not improve the problem of the delay in the access of the patient to a specialised unit.
In one study done to determine the incidence of FI among primary care patients, only one of the 56 patients with FI (10.8% out of 518 patients interviewed) had come to their primary care physician for this reason2; the remainder admitted having this problem only after the physician had specifically asked them. Thomas et al. showed evidence in the United Kingdom of significant differences between the prevalence detected in a mail-in survey and the data obtained from the community healthcare services, which identified the lack of patients with this problem requesting treatment.7
Several studies have been centred on defining the reasons why patients do not discuss FI with their physicians. Barlett et al. identified the following main factors: lack of FI symptoms at the time of the office visit; the patient did not consider the FI a problem; embarrassment; the patient considered that the physician was very busy; the patient preferred to concentrate on the main reason for the office visit.8 In a later study, Kunduru et al. concluded that embarrassment, while quite important for many patients, is not a differential factor between patients who discuss the problem with their physicians an those who do not. They detected two main factors related with more frequent consultation: the severity of the condition, and knowledge about FI and possible treatment options available.9
From our experience, we know that many primary care professionals confess that they do not ask their patients about FI because, among other reasons, they do not have sufficient knowledge to address it and propose an effective solution. A recent study demonstrates that the implementation of training measures and a proactive attitude with direct questions about FI can improve detection in primary care centres.10
On the other hand, some studies discuss who is more responsible for the detection of FI: should the doctor ask, or should the patient consult? Patients interviewed in one study confessed that they would answer questions about this condition if asked by a healthcare professional and they would prefer that the doctor initiated the conversation. Meanwhile, some physicians considered it the responsibility of the patient to comment on the symptoms in cases of wanting to receive treatment, and very few considered FI a medical diagnosis.8,11
In this regard, it is the responsibility of colorectal surgeons to disseminate information about the disease and its treatments in professional forums. On the other hand, the work of the patients themselves is also key. The Association for Anal Incontinence (ASIA; www.asiasuport.org) was created in 2012 and currently conducts several support activities for patients with FI, as well as important work in de-stigmatisation. It also contributes to the dissemination of information and tries to help patients in their access to specialised centres. A recent study on the barriers of patients for asking for help proposes information programmes on FI and possible treatments.12
Finally, we should not forget that the access to certain specialised healthcare resources is limited in some regions; meanwhile, patients are confined to their area of influence within the Spanish national healthcare system and cannot be referred to hospitals with specialised teams or access to specific treatment. This situation should be reported to regional healthcare administrations in order to raise awareness and for changes to be made.
FI affects several patient quality-of-life dimensions. Because it is somewhat taboo, patients do not discuss their problem and, due to the multiple problems involved in the management of healthcare resources, the access to specialised medical centres is not easy for many. With the HRC programme, our intention is to improve the quality of patient care, while optimising the use of resources and reducing testing time in order to receive treatment as soon as possible. According to the results of the questionnaire, patients are satisfied with the medical care received in this type of setting and prefer to complete all the diagnostic tests on the same day.
Authorship/CollaborationAM-D, study design; LL-T and HV-P, data collection; AM-D and LL-T, analysis and interpretation of the results; AM-D, LL-T and AN-L, composition of the article. All the authors participated in the critical review and approval of the final version of the article.
Conflict of InterestsThe authors have no conflict of interests to declare in relation with this study.
The authors would like to thank Cristina Pérez for coordinating the patients treated in this circuit programme.
Please cite this article as: Muñoz-Duyos A, Lagares-Tena L, Vargas-Pierolas H, Rodón A, Navarro-Luna A. Circuito de alta resolución en el diagnóstico de la incontinencia fecal. Satisfacción de los pacientes. Cir Esp. 2017;95:276–282.