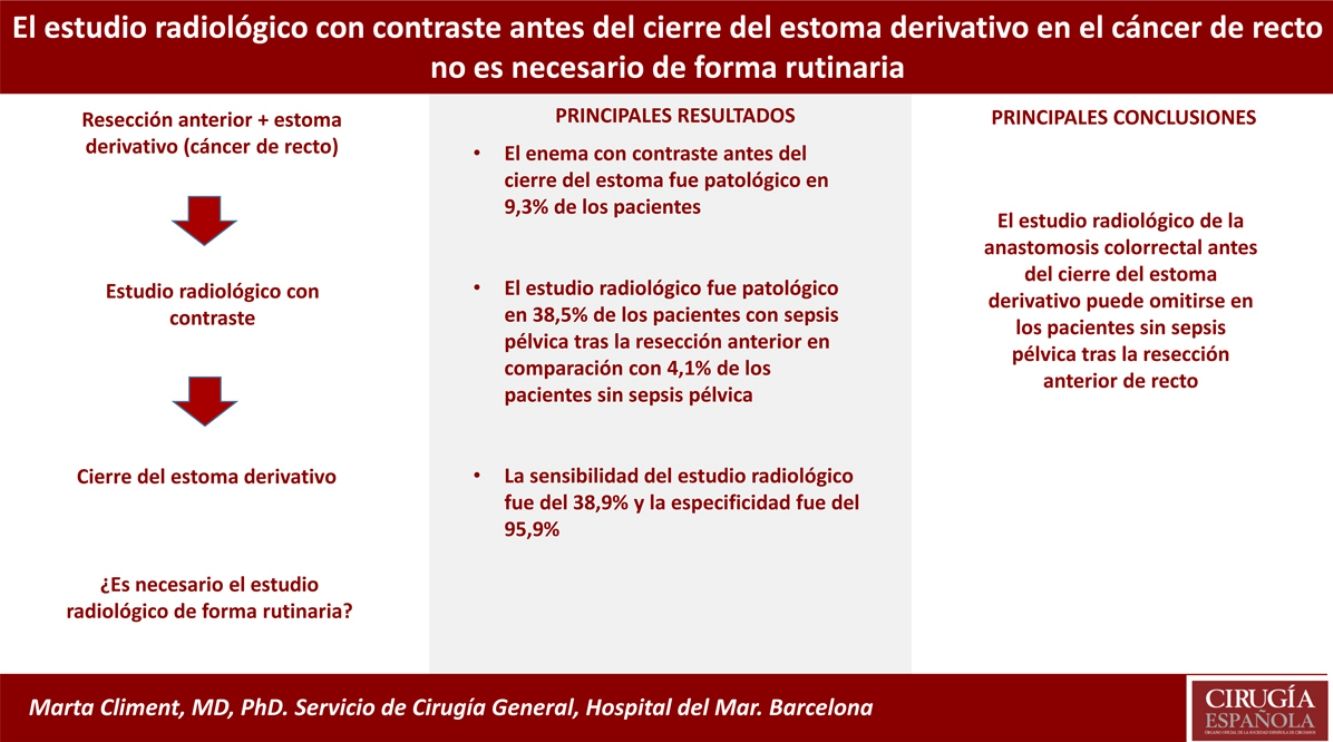
Diverting stomata are recommended in patients with low anterior resection and risk factors in order to reduce the severity of anastomotic leaks. Usually, a radiology study is performed prior to the closure of the stoma to detect subclinical leaks. The aim of the present study is to assess the clinical utility of the radiology study.
MethodsA prospective cohort study of patients undergoing anterior rectal resection for rectal cancer and those who underwent stoma closure without contrast enema. This study was carried out after a retrospective review of radiology study results prior to the closure of the stoma in patients operated from 2007 to 2011.
ResultsEighty-six patients met the study criteria. Thirteen patients (15.1%) presented pelvic sepsis. Contrast enema before stoma closure was pathological in 8 patients (9.3%). Five out of the 13 patients with pelvic sepsis had a pathological radiological study, compared to only 3 out of the 73 patients without intra-abdominal complications after rectal resection (38.5% vs 4.1%; P=.001). Based on these results, we conducted a prospective study omitting the contrast enema in patients with no postoperative complications. Thirty-eight patients had their stoma closed without a prior radiology study. None of the patients presented pelvic sepsis.
ConclusionsRadiology studies of the colorectal anastomosis before reconstruction can safely be omitted in patients without pelvic sepsis after the previous rectal resection.
Es recomendable practicar un estoma derivativo en pacientes con resección anterior baja y factores de riesgo, para reducir la gravedad de la fuga anastomótica. Habitualmente se realiza un estudio radiológico previo al cierre del estoma para detectar fugas subclínicas. El objetivo del presente estudio es evaluar la utilidad clínica del estudio radiológico.
MétodosEstudio prospectivo de una cohorte de pacientes sometidos a resección anterior de recto por cáncer rectal, y a los que se les realiza cierre del estoma sin enema de contraste. Este estudio se lleva a cabo después de realizar una revisión retrospectiva sobre los resultados del estudio radiológico previo al cierre del estoma en pacientes intervenidos entre 2007 y 2011.
ResultadosOchenta y seis pacientes cumplieron los criterios del estudio. Trece pacientes (15,1%) presentaron sepsis pélvica. El enema con contraste antes del cierre del estoma fue patológico en 8 pacientes (9,3%). Cinco de los 13 pacientes con sepsis pélvica mostraron un estudio radiológico patológico, en comparación con solo 3 de 73 pacientes sin complicaciones intraabdominales después de la resección del recto (38,5% vs 4,1%; p=0,001). Basándonos en estos resultados, realizamos un estudio prospectivo omitiendo el enema con contraste en pacientes con curso postoperatorio no complicado. A 38 pacientes se les cerró el estoma sin estudio radiológico previo. Ningún paciente presentó sepsis pélvica.
ConclusionesEl estudio radiológico de la anastomosis colorrectal antes de la reconstrucción del tránsito puede omitirse con seguridad en los pacientes sin sepsis pélvica ni íleo paralítico tras la resección anterior de recto.
The incidence of anastomotic leakage after anterior resection of the rectum ranges from 3% to 20%,1–3 depending on the definition of dehiscence, among other factors. This is a serious complication associated with considerable morbidity and mortality, and the location of the anastomosis is the most important risk factor. A low colorectal or coloanal anastomosis after total mesorectal excision is associated with a greater risk of anastomotic dehiscence compared to a higher anastomosis.4 Male sex, obesity and the absence of a protective stoma are also known risk factors for dehiscence.5,6 For this reason, in the case of low anterior resection, it is recommended to divert the intestinal contents and protect the anastomosis with a stoma. The current trend is to perform a loop ileostomy instead of a colostomy.3 Although it has previously been shown that proximal diverting stomata do not reduce the incidence of dehiscence, they do minimize the severity and septic consequences of anastomotic leaks.3–5
Closure of the ileostomy usually takes place between 6 and 24 weeks after rectal resection, depending on the administration of adjuvant treatment.7,8 In most cases, a radiological study is carried out using contrast enema prior to the closure of the stoma in order to assess the integrity of the anastomosis. Although some authors have questioned the need for systematic radiological studies,9,10 others defend their usefulness in the detection of subclinical leaks, sinus and stenosis.11,12 In fact, despite the delay in stoma closure and the morbidity that the technique can entail, the standard practice in most hospitals is to assess the anastomosis with contrast enema prior to the closure of the ileostomy or colostomy.9,13 The hypothesis of the present study proposes that radiological evaluation of the anastomosis prior to closure of the diverting stoma is only necessary in patients with rectal cancer surgery who presented postoperative pelvic sepsis (abscess or anastomotic leak). Our objective is to evaluate the clinical utility of the routine use of contrast-enhanced radiological studies before closure of the protective stoma in rectal cancer surgery patients.
MethodsRetrospective StudyIn an initial phase, a retrospective review was carried out of patients who had undergone anterior resection of the rectum, identified in a prospectively maintained database, between January 2007 and December 2011. The patients selected had undergone partial or total mesorectal excision for rectal cancer together with a diverting loop stoma. Patients with a diverting stoma created in a second surgery to treat anastomotic leakage were excluded.
Demographic and perioperative data were collected, such as the administration of preoperative chemoradiotherapy, extension of the mesorectal excision, type of anastomosis and the use of a colonic reservoir as a rectal substitute. The most relevant postoperative complication for the present study was the diagnosis of pelvic sepsis, defined as a clinical leak or the presence of a pelvic abscess. The presence of purulent discharge through the anus was also recorded, even in the absence of pelvic abscess, as well as the treatment of these complications.
After completing adjuvant treatment when indicated, patients were evaluated before the closure of the stoma by digital rectal examination and contrast imaging. Following the protocol of our hospital, the contrast enema is carried out through the efferent loop of the stoma. A 16-F Foley catheter is inserted into the efferent loop of the ileostomy or colostomy, and the balloon is inflated with 10mL of serum to anchor it. One liter of water-soluble contrast medium is administered (meglumine amidotrizoate) mixed with the same volume of water to distend the anastomosis, and X-rays are taken once the contrast has reached the anal canal.14 The data from this study were also collected, and tests were considered pathological when a presacral cavity, sinus or stenosis was demonstrated. The sensitivity and specificity of the radiological study were calculated to evaluate its clinical usefulness. Finally, the time elapsed between the anterior resection of the rectum and the closure of the stoma was analyzed.
Prospective StudyGiven the findings of the retrospective study, we prospectively analyzed a selected cohort of patients, omitting the contrast enema prior to closure of the stoma in order to establish a new management protocol at our hospital. All patients with previous rectal cancer surgery who did not present pelvic sepsis in the postoperative period of the previous resection were included prospectively. Pelvic sepsis was defined as suture dehiscence or pelvic abscess diagnosed either by radiological techniques or during surgical reoperation. Patients with paralytic ileus were also excluded from the analysis because of the possible relationship with a subclinical leak. The anastomosis was evaluated by digital rectal examination, and the stoma was closed without a radiological study. Both the retrospective and the prospective studies were approved by the Ethics Committee at the Hospital del Mar, where the study was carried out. Informed consent was obtained from all patients included in the prospective study.
Statistical AnalysisAs part of the descriptive analysis, the data are presented as frequencies and percentages for the qualitative variables and as means and standard deviation for the quantitative variables. To compare results between the group of patients with postoperative sepsis and the group with normal postoperative recovery, a crosstab was performed with Fisher's test, since some of the cells had an absolute value of less than 5. For the analysis of the time transpired between the lower anterior resection and the closure of the stoma, the means between the study groups were compared using a Student's t test for independent samples.
ResultsRetrospective StudyThe study included a total of 86 patients who had undergone previous low anterior resection for rectal cancer during the study period and met the selection criteria. There were 60 men (70%), and the mean age was 64.5 years (Table 1). Diverting loop ileostomy was performed in 84 patients and loop colostomy in the remaining 2 patients. During the postoperative period, 13 patients (15.1%) presented pelvic sepsis: 3 clinical anastomotic dehiscence and 10 pelvic abscesses. Reoperation was necessary in 3 patients with pelvic sepsis, who required lavage of the abdominal cavity and placement of surgical drains. The remaining 10 patients were treated with percutaneous or transanal drainage. Disconnection of the anastomosis was not necessary in any of the cases.
Demographic Data and Clinical Characteristics.
| n=86 (%) | ||
|---|---|---|
| Sex | Female | 26 (30.2) |
| Male | 60 (69.8) | |
| Age (yrs) | 64.5±12 | |
| Neoadjuvant radiotherapy | 46 (53.5) | |
| Anastomosis | Manual | 15 (17.4) |
| Mechanical | 71 (82.6) | |
| Type of reconstruction | End-to-end | 54 (62.8) |
| Side-to-end | 18 (20.9) | |
| Colonic J-pouch | 13 (15.1) | |
| Ileal J-pouch | 1 (1.2) |
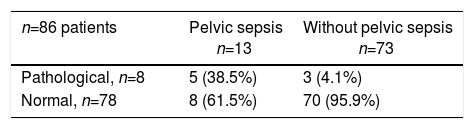
The time interval between rectal resection surgery and the enema with water-soluble contrast through the efferent loop of the stoma was 5.2±3.9 months. Usually, the test is requested from the colorectal surgery outpatient clinic, coinciding with one of the postoperative office visits. In one patient, the stoma was perforated during the procedure, which required urgent surgery. The radiological study was pathological in 8 out of 86 patients (Table 2). In 5 out of 13 patients who had presented pelvic sepsis after the anterior resection of the rectum, the contrast study was pathological (presacral cavity in 4 patients and sinus in one case). In contrast, in the group of 73 patients without pelvic sepsis, only 3 studies with contrast were pathological: one anastomotic stenosis successfully treated with dilatations, and two sinuses at the anastomosis that resolved without treatment 3 months after diagnosis. The sensitivity of the radiological study was 38.9% and the specificity was 95.9%.
The time interval from rectal resection until closure of the stoma was 7.8±4.7 months in the group of patients without pelvic sepsis and 9.1±3.3 months in the group of patients with pelvic abscess or leak. Stoma closure was performed in all patients except one, who had presented anastomotic leak and developed a local recurrence. The time interval was 7.7±4.6 months in patients with normal contrast studies, compared to 10.6±2.5 months in the group of patients with presacral cavity or sinus (P=.087). The morbidity of the stoma closure was 12.8%: 5 wound infections and 5 anastomotic dehiscence (percutaneous drainage in 3 patients and 2 surgical reoperations with anastomotic reinforcement).
Prospective StudyFrom January 2012 to December 2016, 38 patients (48.1% of patients with anterior resection and a diverting stoma in this period of time) underwent stoma closure without prior contrast study, following the inclusion and exclusion criteria. The mean time from the low anterior resection until the closure of the stoma was 7±3.6 months. Morbidity after stoma closure was 18%, and the most frequent complication was wound infection in 3 cases (7.9%). No patient presented immediate or late-onset clinical pelvic sepsis.
DiscussionThis study demonstrates that contrast radiography of a low colorectal anastomosis before the closure of a diverting stoma does not reveal abnormalities in the vast majority of patients with no postoperative complications. Therefore, it can be safely omitted. In contrast, almost half of the patients who presented pelvic sepsis in the postoperative period after anterior rectal resection had a pathological radiological test, revealing a presacral cavity or a sinus. In our opinion, radiological studies are only necessary in these patients. Both the retrograde technique (enema through the anal canal) and the antegrade technique (contrast through the efferent loop of the stoma) are considered standard methods for assessing anastomotic integrity,14,15 but the incorrect position of the catheter over the suture in the retrograde technique can lead to incorrect evaluation of the anastomosis and overlook a dehiscence. Furthermore, in early stoma closure, there is a risk of traumatizing the anastomosis with the catheter, so the retrograde technique is not recommended.14
Our data confirm the results of other groups suggesting that routine contrast-enhanced radiological studies are not necessary after anterior rectal resection.9,10,16 In a series of 81 patients who underwent low anterior resection with loop ileostomy due to rectal cancer, the incidence of contrast leakage in the group without complications was low (5.8%); stoma closure was carried out either with or without water-soluble enema, and the authors concluded that routine enemas in the absence of clinical suspicion of anastomotic leakage are of little value.13 Kalady et al.10 reviewed 211 patients who had temporary loop ileostomy after a previous resection for rectal cancer or to protect an ileal reservoir after proctocolectomy. As in the present study, the imaging study did not reveal an anastomotic leak that was not already suspected clinically. In addition, a patient with a normal contrast study presented a leak after the ileostomy was closed. The same results were obtained when the usefulness of the radiological evaluation was analyzed in patients with colonic J-pouch after total excision of the mesorectum.9
Despite this evidence, several authors still defend that contrast enema studies are useful to detect anastomotic complications before stoma closure. Arumainayagam et al.17 published a retrospective review of a series of 86 patients who underwent ileostomy closure after total mesorectal excision. A contrast enema was performed before closure of the ileostomy. Thirteen patients (15%) presented radiological anastomotic leak (sinus in the anastomosis), only 5 (6%) of which were symptomatic. In a recent study aimed at evaluating the results of an early stoma closure protocol, asymptomatic radiocontrast leaks were observed in 6 out of 64 patients (9.3%). The authors defend the use of routine enemas, especially when early stoma closure is planned, because many clinical leaks in patients with stoma may appear late, occurring several weeks after surgery.7
The results of our study favoring the omission of radiological studies are likely due to the selection of patients without postoperative complications. The contrast studies were normal in 95.9% of the patients without postoperative pelvic sepsis after rectal resection, but they were only normal in 61.5% of the patients who had presented anastomosis-related complications. Therefore, we excluded from the prospective study not only patients with clinical anastomotic leak or pelvic abscess after low anterior resection, but also those with symptoms or signs suggestive of leakage, such as transanal purulent secretion or prolonged paralytic ileus. Although the number of patients is a clear limitation of this study and we cannot exclude a type II error in the prospective analysis, we can affirm that contrast enemas can safely be omitted in most patients. If we compare the morbidity between the two patient series, the complication rate in the prospective group without radiological study was slightly higher than in the series of patients without contrast, but the most frequent complication was wound infection, whereas in the retrospective group anastomotic dehiscence required reoperation on 2 occasions.
It may be argued that the benefit of omitting the radiological study is limited. It is true that the morbidity of the test is low and the cost is not very high. However, it delays stoma closure, as we have demonstrated in our analysis. Another advantage of not performing the pre-closure study is to avoid potential complications, such as perforation of the ileostomy, as described in our series, or other complications described in the literature.18 Therefore, if contrast studies are not useful and rarely change the management of these patients, their use should no longer be routine. In this regard, several studies have found low sensitivity of the radiological evaluation of the anastomosis for the prediction of complications after stoma closure. In a series of 84 patients who had undergone a colonic J-pouch procedure, the sensitivity of the contrast enema to detect pouch complications was low (25%) and changed the treatment in only one out of 84 patients.9 Hong et al.19 retrospectively reviewed 145 patients who underwent temporary loop ileostomy to protect a low colorectal or coloanal anastomosis. A late-onset anastomotic leak occurred after stoma closure in 3 patients (2.1%). One of them had presented stenosis in the contrast enema study, while the radiological studies of the other 2 patients had been normal.
In conclusion, contrast radiography in patients with low colorectal anastomosis before diverting stoma closure is not routinely necessary and can safely be omitted in patients who do not present with pelvic sepsis or paralytic ileus in the postoperative period after anterior resection.
FundingNo funding was needed to conduct this study.
Authorship- •
Marta Climent: study design, data collection, analysis and interpretation of the results, article composition and approval of the final version.
- •
Marta Pascual: analysis and interpretation of the results, approval of the final version.
- •
Sandra Alonso: analysis and interpretation of the results, critical review and approval of the final version.
- •
Silvia Salvans: analysis and interpretation of the results, critical review and approval of the final version.
- •
M. José Gil: analysis and interpretation of the results, critical review and approval of the final version.
- •
Luis Grande: analysis and interpretation of the results, critical review and approval of the final version.
- •
Miguel Pera: study design, analysis and interpretation of the results, article composition, critical review and approval of the final version.
There were no conflicts of interests.
Please cite this article as: Climent M, Pascual M, Alonso S, Salvans S, Gil MJ, Grande L, et al. El estudio radiológico con contraste antes del cierre del estoma derivativo en el cáncer de recto no es necesario de forma rutinaria. Cir Esp. 2019;97:145–149.