In recent years, different endoscopic techniques have been described as alternatives to minimally-invasive surgery for the treatment of obesity.1 Among these, the Primary Obesity Surgery, Endoluminal (POSE) procedure is an innovative technique that is less invasive and safer for the treatment of obesity. In this procedure, the stomach is plicated at 8–9 locations of the fundus and another 3–4 in the antrum, using specific sutures. Supposedly, these mechanically and physiologically plicated areas restrict the contact of food with the total surface of the stomach. The antrum folds modify its shape and cause slower gastric emptying, which increase the satiating effect.2,3
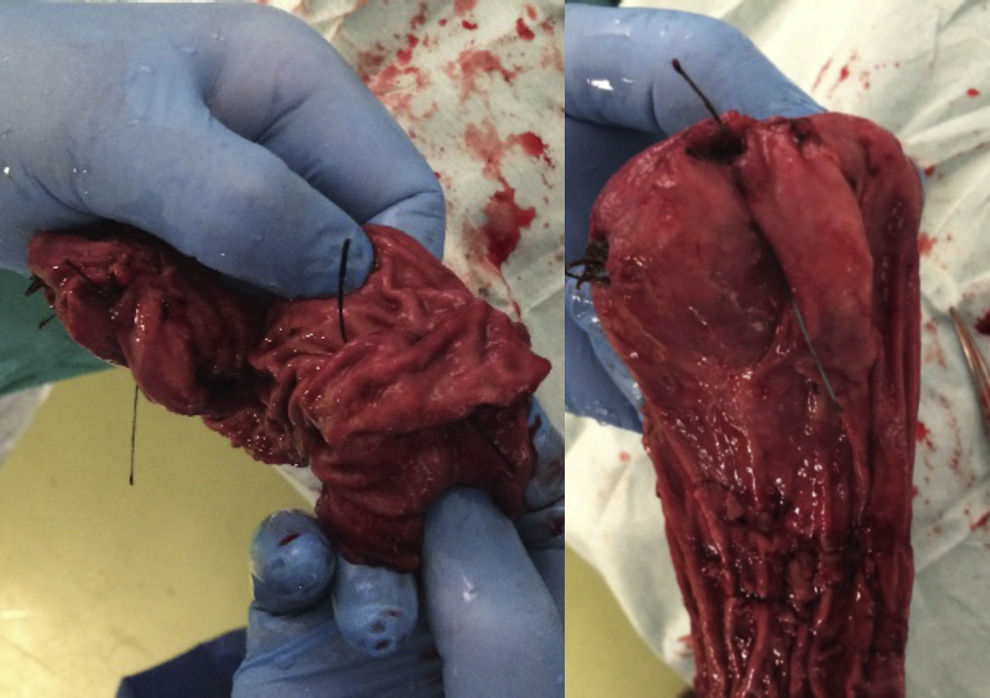
We present the case of a 41-year-old patient who underwent a POSE procedure after 18 months of failed weight loss attempts. She came to our consultation due to a weight gain of 12kg after POSE and was interested in bariatric surgery. The patient had presented a BMI of 33kg/m2 and arterial hypertension before the endoscopic procedure. When she came to our office, the patient had a BMI of 35kg/m2. During preoperative testing, the patient refused gastroscopy, so an upper gastrointestinal series was done; there was no evidence of reflux, the stomach demonstrated good motility and emptying, and the fold pattern was normal. No ulcerous images were observed (Fig. 1).
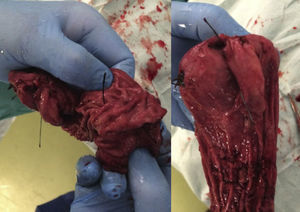
After a complete study by our multidisciplinary team, the patient was scheduled for laparoscopic vertical sleeve gastrectomy. During surgery, we found a series of small adhesions to the liver and on the posterior side of the stomach (the large majority). During dissection of the greater curvature, no plications or torsion were detected, except for the adhesions, and there were 2 areas of thickening (one at the greater curvature and another in the antrum). The stomach seemed to be completely normal. Surgery was completed with dissection up to the cardiac notch; gastrectomy was performed with an endocutter and reinforced with 2–0 barbed suture. During these maneuvers, we encountered no difficulties that would distinguish our patient from subjects who had not undergone previous surgery. When we examined the surgical specimen, we observed the 2 areas of folds (fundus and antrum), but no evidence of reduced gastric capacity (Fig. 2). After 48h, the patient was discharged from the hospital.
During recent years, a number of endoscopic techniques like the POSE technique have tried to reproduce the manipulations and physiological effects of minimally-invasive surgery for the treatment of morbid obesity.1,4 In this manner, POSE tries to reduce the capacity for food storage and induce early satiety while slowing gastric emptying by creating folds in the gastric fundus and antrum.
To date, only one study has been published by Espinós et al.,5 which included 45 obese patients with a mean BMI of 36.7 and a follow-up of only 6 months. They presented a reduction in BMI of 5.8 (31.3) and an SPSS of 49.4%. Their conclusion was that POSE seems to be a safe and effective weight loss procedure without the pain, scars or long recovery of surgery. Deitel and Greenstein6 propose using the percent of BMI lost (PBMIL) to assess the results, considering 65% or more to be excellent, 50% to 65% good, and less than 50% as poor. In the study mentioned the authors did not use PBMIL but used percent of excess weight lost and BMI lost instead.
In their response to the cited article, Vilallonga and Himpens7 are aware of the limited number of publications that seem to support the efficacy of plication of the gastric fundus or even the antrum, presumably activating the receptors of satiety, or slowing gastric emptying. They believe that the mechanisms related with satiety, motility or even gastric volume are complex and cannot be explained simply by an unmeasurable reduction of the gastric fundus.
In any case, conclusions cannot be drawn from such a small cohort and a follow-up of only 6 months. Well-designed, randomized, controlled studies are necessary to determine short- and long-term efficacy and safety.
It is possible that we may find ourselves treating more and more patients, in whom treatment of this type has failed, and who are looking for a definitive solution. As we have commented, in our case laparoscopic vertical sleeve gastrectomy after a previous POSE procedure is not much different than in a patient who has not had a previous gastric technique. In our patient, we only found a small amount of thickening in the area of the fundus and antrum, which did not complicate dissection or gastrectomy with the use of an endocutter. In any event, a careful, precise technique is recommended since, as in any revision surgery, there may be a higher percentage of complications in these patients.8,9 Adhesions should be freed to maintain normal gastric anatomy, and areas of fibrosis and edema should be located in order to avoid resection in such areas, if possible. We also recommend reinforcing the resection line in these patients, even though it has not been shown to reduce the risk of fistulas.10
Please cite this article as: Ferrer-Márquez M, Ferrer-Ayza M, Rubio-Gil F, Torrente-Sánchez MJ, Martínez Amo-Gámez A. Revisión quirúrgica bariátrica tras POSE. Cir Esp. 2015;93:353–354.