Metastatic disease of the penis is a rare occurrence. In a large series of autopsies performed in the Royal London Hospital on 623 patients who died due to secondary genitourinary tract malignancies, only 5 were located in the penis.1 This clinical condition represents an advanced stage of the primary neoplasm and the overall outcome is generally poor. The most frequent sites of the primary tumor are bladder (34.7%), prostate (29.8%), recto-sigmoid colon (15.7%), and kidney (6.5%).2 Few cases of penile metastasis from colorectal cancer have been reported.3–6 We present a case of penile metastasis from rectal carcinoma. Written informed consent for scientific use of the images was obtained from the patient.
A 70-year-old man was admitted to the hospital with 4 months of penis pain and voiding dysfunction. He had a past history, eight years before, of prostate carcinoma treated with radiotherapy, chemotherapy and hormonotherapy, with no evidence of disease recurrence in routine postoperative follow-up. Thirty months before he had been diagnosed of rectal cancer and underwent neoadjuvant chemotherapy, robot-assisted laparoscopic abdominoperineal resection (Miles’ procedure), colostomy and adjuvant chemotherapy. Radiotherapy was not administrated due to the previous high-dose pelvic radiotherapy treatment that had been given for prostate carcinoma. Pathological examination of the rectal cancer specimen revealed a moderately differentiated adenocarcinoma infiltrating the perirectal fat (pT3), with a radial margin of 0.3cm and perineural and vascular. All the 20 lymph nodes removed were negative for metastasis (N0).
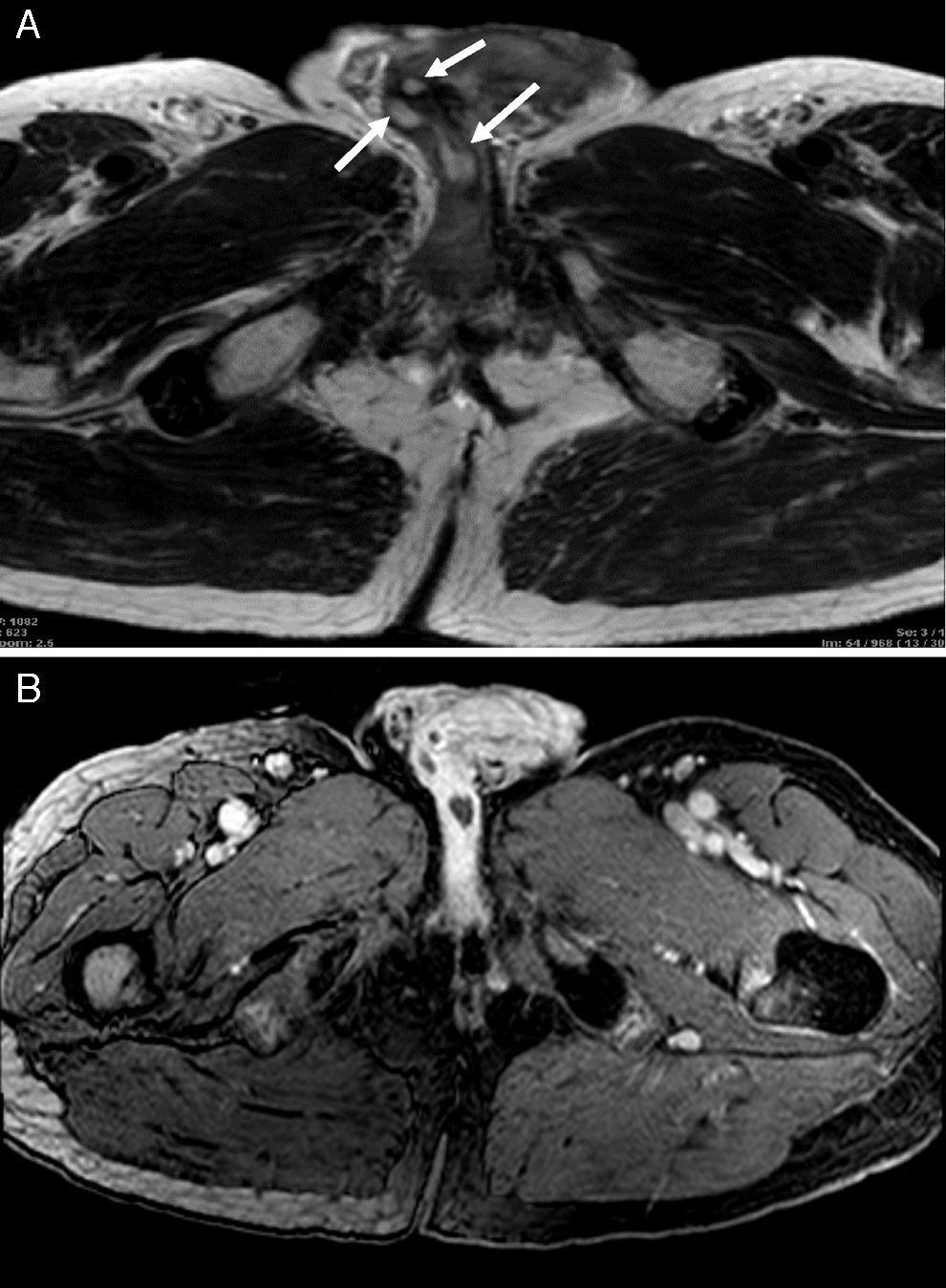
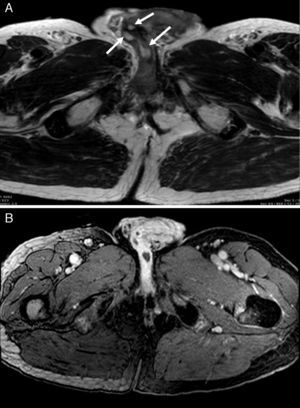
Physical examination revealed a painful induration along the shaft of the penis and ulcers on the glans. Biochemical blood analysis evidenced a progressively rising serum CEA levels from 2.3ng/mL to 10.9ng/mL over the last 8 months. Penile ultrasound showed heterogeneous masses in both corpora cavernosa with interruption of the tunica albuginea. Additionally, three hypoechoic urethral masses were detected, which produced dilation of the proximal urethra. Ultrasound scan findings suggested penile metastases. A suprapubic catheter was inserted into the urinary bladder. A computerized tomography showed postsurgical changes in the pelvis and no other findings. A whole body 18F-FDG PET/CT scan was performed for restaging. Images showed hypermetabolic lesions in the proximal shaft of the penis, distal penis and glans. Furthermore, multiple hypermetabolic bone metastases were detected in the pelvis. Local tumor recurrence was not observed (Fig. 1). Pelvic magnetic resonance imaging showed multiple low-signal-intensity lesions on T1-weighted sequences, involving the corpora cavernosa and the glans. After gadolinium administration, the lesions showed peripheral enhancement (Fig. 2). Pelvic bone metastases were also confirmned. Biopsies of the urethra, glans and corpora cavernosa revealed infiltration of adenocarcinoma. Inmunohistochemical staining of the tumor cells was positive for cytokeratine 20, CDX2 and racemase, and negative for cytokeratin 7 and PSA. These findings supported the diagnosis of metastatic lesions from rectal cancer. Surgery, radiotherapy and chemotherapy would have been valid therapeutic options in such a case. Considering the previous pelvic radiotherapy administrated for the prostatic carcinoma, the patient underwent chemotherapy with FOLFIRI® (folinic acid, fluorouracil and irinotecan) plus Bevacizumab. Twelve months after the diagnosis, the patient is still undergoing treatment with minor side effects.
Oncologic male patients can seek medical attention for penile complaints. Most of them come from minor benign problems, but may mask a serious underlying health condition. The most common clinical manifestations of penile metastasis are priapism, penile or perineal pain, and voiding disturbances.4 Despite its rich vascularization, the penis is rarely involved in metastatic spread of tumors located in other organs. In 1956, Paquin and Roland7 described the possible mechanisms of tumor spread to the penis as follows: direct extension, retrograde venous route, retrograde lymphatic route, direct tumor extension into branches of the hypogastric arterial pathway, metastatic tumor emboli from secondary tumor deposits in the lungs, tertiary embolism from liver metastasis producing metastasis to the lung and subsequent penis tumor emboli, and spread by instrumentation (iatrogenic).
The management of patients with serial CEA elevation after resection of rectal cancer includes physical examination, colonoscopy, and chest, abdominal and pelvic computerized tomography. Recently, the National Comprehensive Cancer Network guideline for rectal cancer, version 1.2016, took into consideration the use of 18F-FDG PET/CT scan in patients with rising serum CEA levels after curative resection to detect tumor recurrence.8 Giacomobono et al.9 reported that 18F-FDG PET/CT allowed the identification of distant metastasis in patients with unexplained CEA rise after curative surgery of colorectal cancer. In a meta-analysis on the diagnostic performance of 18F-FDG PET or PET/CT in patients with elevated CEA serum levels, Lu et al.10 found a sensitivity and specificity of 94.1% and 77.2%, respectively of 18F-FDG PET/CT in the detection of tumor recurrence.
Diagnosis of penile metastasis is usually performed by biopsy or fine-needle aspiration. Penile metastasis represents a spread from the primary tumor. Non-invasive imaging methods are performed to determine the extent of the disease.4,6 In the case presented here, penile ultrasound was the first procedure to identify tumor involvement of the penis and the urethra. In addition to penile metastases, 18F-FDG PET/CT scan revealed unknown bone metastatic spread to pelvis, not detected by computerized tomography, but confirmed by magnetic resonance imaging.
Conflict of InterestThey have not received support in the form of scholarships for study.
The information of the manuscript has not been previously presented at a conference.
Please cite this article as: Gómez-de la Fuente F-J, Martínez-Rodríguez I, Alonso-Martín J, Jiménez-Bonilla J, Banzo I. Presentación de un caso de metástasis en pene de carcinoma rectal. Cir Esp. 2017;95:116–118.