Flail chest is managed with mechanical ventilation or inhalation therapy, and analgesia. Mechanical ventilations carry risks by themselves, and disengage with the external fixators, so they must be operated to improve lung ventilatory mechanics and cleaning. Little has been published on the use of bio-absorbable material and its evolution in the setting of flail chest.
Material and methodsA study was made on a material that did not have to be removed, that had the malleability of steel, its inflammatory reaction was minimal, and could be handled in both adults and children. A descriptive study is presented of patients with flail chest under rib fixation with plates and bio-absorbable screws.
ResultsA series of 18 cases are presented, with ages from 33-74 years, three with bilateral flail chest. Fixation was performed between days 1-21 of the accident. In cases that showed no fractures of pelvic limbs, walking was restarted the day after fixing. In all cases mechanical ventilation improved and pain decreased. So far there has been no reaction to the material.
ConclusionsFlail chest has a high (16.3%) mortality when the pathophysiology of the condition (pain, poor mechanical ventilation, alveolar oedema-pulmonary contusion) is not treated. The use of bio-absorbable material has no side effects attributable to material, making it another option for rib fixation.
El tórax inestable se maneja con ventilación mecánica o inhaloterapia y analgesia. Los pacientes ventilados mecánicamente tienen los riesgos de la ventilación misma y se desacoplan con fijadores externos, se debe operar para mejorar la mecánica ventilatoria y la limpieza pulmonar. Poco se ha publicado del uso de material bioabsorbible y su evolución en la fijación de tórax inestable.
Material y métodosSe investigó un material que no tuviese que retirarse, que presentará la maleabilidad del acero y que su reacción inflamatoria fuera mínima, que además pudiese ocuparse tanto en adultos como niños. Se presenta un estudio descriptivo de pacientes con tórax inestable sometidos a fijación costal con placas y tornillos bioabsorbibles.
ResultadosSe presentan 18 casos, con edades entre los 33 y los 74 años, 3 con tórax inestable bilateral; la fijación se realizó entre los días 1 y 21 del accidente. En aquellos casos en que no se presentaban fracturas de extremidades pélvicas, se reinició la deambulación al día siguiente de la fijación, en todos los casos mejoró la mecánica ventilatoria, el dolor disminuyó y ninguno hasta el momento ha presentado reacción al material.
ConclusionesEl tórax inestable tiene una mortalidad alta (16.3%) cuando no se brinda manejo a la fisiopatología del cuadro (dolor, mala mecánica ventilatoria, contusión pulmonar-edema alveolar). El uso de material bioabsorbible no tiene efectos secundarios atribuibles al material, por lo cual es una opción más para la fijación costal.
Thoracic trauma, according to Wilson et al.1 is responsible for 25% of the 50 to 60,000 deaths that annually occur due to car accidents, 25% of which correspond to unstable thorax, or flail chest (FC)2–4, which presents paradoxical respiration. When accompanied by other injuries, FC considerably raises the mortality rate5,6. It was believed that the main lesion was loss of the rib cage architecture, which in turn produced respiratory insufficiency, but it has been demonstrated that other factors cause respiratory insufficiency, such as pulmonary contusion, pain, and shock, among others7,8. The capillary lesion produces an intra-alveolar and interstitial haemorrhage with oedema, which develop an intrapulmonary shunt, with the subsequent reduction of the functional residual capacity and pulmonary compliance, which in turn increases respiratory effort and leads to quick muscle fatigue, mainly if associated with pain and shock. In the absence of shock, this condition develops in an average of 6 to 12hours after trauma9–12. Treatment for unstable thorax has been conditioned by the accepted physiopathology in every stage; that is to say, when the problem was considered to be caused by the instability of the chest wall, treatment was oriented in that sense13–15. In 1956, Avery16 used internal pneumatic stabilization as a treatment for flail chest, with the aim of correcting the wall defect by applying positive pressure ventilation. This favoured bone consolidation16–18, but also respiratory infections from the prolonged ventilation, with subsequent tracheostenosis and death of the patient18. The methods of ventilation used are: positive end expiratory pressure (PEEP), continuous positive pressure ventilation alone, or combined with the intermittent mandatory ventilation. Recently, authors such as Hormaechea19 and Lardinois et al.10 recommended the use of high-frequency positive pressure ventilation combined with low-rate conventional mechanical ventilation, reporting peak pressures and lower PEEP, which minimize barotrauma. They observed less damage to pulmonary tissues from oxygen exposure at a lower concentration of oxygen and better consolidation of the fracture by minimum and strictly necessary movement, as the cycles are adjusted from 130 to 169 cycles/min. In 1975, Trinkle et al.17 supported the conservative management for efficient pulmonary hygiene. Irrespective of the management therapy, we must remember that patients with this lesion frequently present multiple injuries and can present head injury, lesions in the internal abdominal organs, long bone fractures, haemopneumothorax, etc., which worsen prognosis and increase morbidity and mortality. Currently, it is known that when there is flail chest with sternal fracture, external fixation of the sternal fracture or osteosynthesis must be performed as part of the treatment. Rib fixation must be performed when flail chest is diagnosed or when, without being unstable in the strict sense of the definition, there are more than seven ribs fractured in the same hemithorax, which may or may not include the sternum. Whenever fractured, the sternum must be fixed, as it may lead to mechanical instability19.
The bioabsorbable LactoSorb®20 material is the only material proven to be absorbed or to disappear in a year or less. Since its introduction in 1996, it has been particularly used in craniofacial surgery. This material is comparable to titanium plates regarding malleability. The initial strength decreases to 70% after eight weeks of implantation, the time needed for bone consolidation. The minimal inflammatory reaction, the absence of migration, and its high effectiveness have been proven in both children and adults20. The material of the plates used has a time of resorption of approximately 12 months; the implant is sensitive to tissue temperature, diminishes potential growing restrictions and the migration of the screws in paediatric patients, and eliminates the need for implant removal. In paediatric studies, a low incidence of inflammatory and infectious reactions is reported20.
Little has been published in the medical literature on rib fixation with bioabsorbable material, so the aim of this study is to use a material with adequate tensil strength, not comparable to that of the titanium/steel material, but sufficient to maintain the union of the ribs and independently favour consolidation of the fracture site. It has to be a material with a rejection rate which is minimum, that does not need to be removed, which helps to avoid additional surgery in patients with multiple injuries, and that could be handled in patients of all ages, regardless of associated pathologies. For all these reasons, we decided to use a malleable, resistant and biodegradable material to offer another option to rib fixation therapies.
Material and methodsDescriptive, observational, non-blind, controlled clinical study conducted at Instituto de Salud del Estado de México Centro Médico Ecatepec from February 1, 2009 to December 31, 2011. The study included all the patients admitted to the hospital (both to the emergency department [17] and to the outpatient service [1,sent by the Orthopaedics Department]) with a diagnosis of flail chest, who met the following criteria: with or without associated injuries, with or without concomitant diseases, regardless of age and gender and of the mechanism of injury. Patients with single rib fractures and with four or less fractured ribs were excluded. Patients who died from associated injuries and who did not undergo surgical fixation were excluded, as were those who had only chest trauma but no rib or sternal fractures.
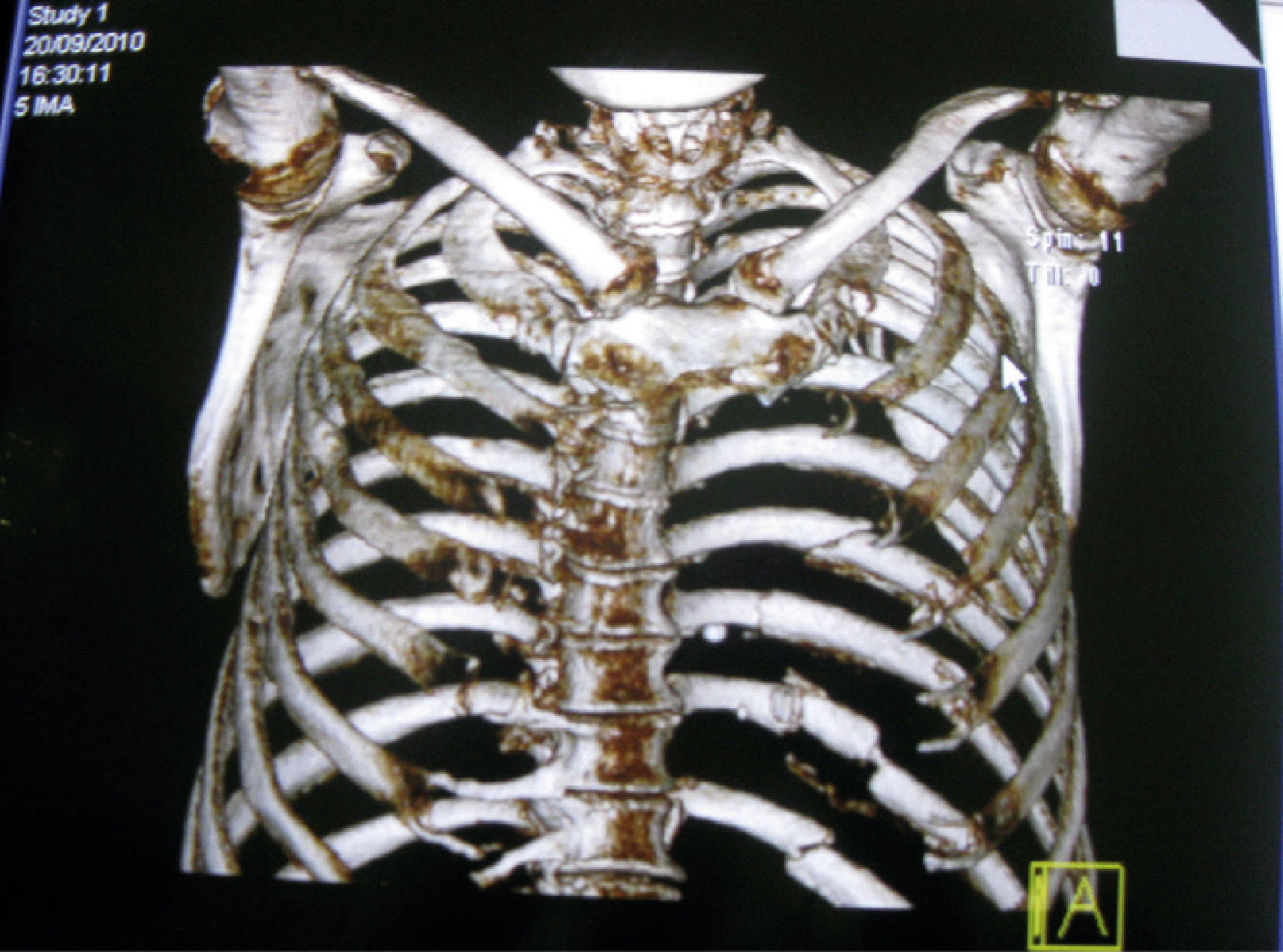
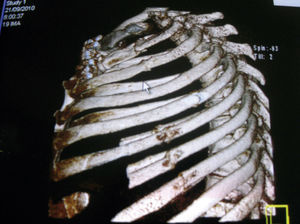
All patients had a computerised tomography of the thorax and bone reconstruction (Fig. 1), teleradiography of the thorax, nine of the cases underwent abdominal ultrasound, and two patients had a cranial tomography. Other studies included postoperative chest x-ray and tomography for monitoring, one month and five months after fixation.
The bioabsorbable LactoSorb®20 material was chosen as it is the only material proven to be absorbed or to disappear in a year or less. It has been used particularly in craniofacial surgery. It is comparable to titanium/steel plates due to its malleability; the initial strength decreases to 70% 8 weeks after implantation, which is the adequate time for bone consolidation. Also, its minimum inflammatory reaction and the absence of migration have been proven, as well as its high effectiveness in both children and adults. The implant is sensitive to tissue temperature, diminishes potential growing restrictions and the migration of the screws in paediatric patients, and eliminates the need for implant removal. A low incidence of inflammatory and infectious reactions has been reported.
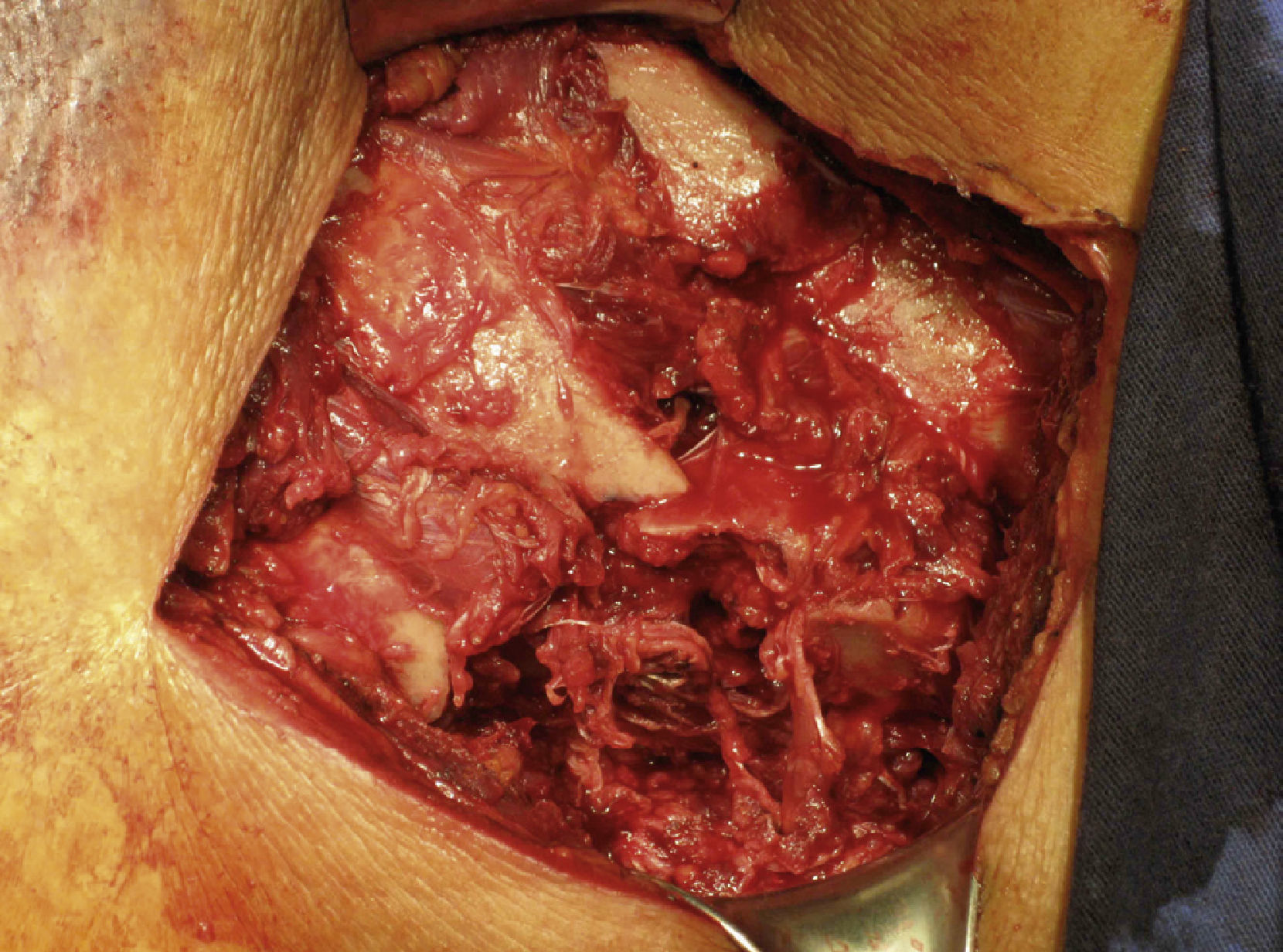
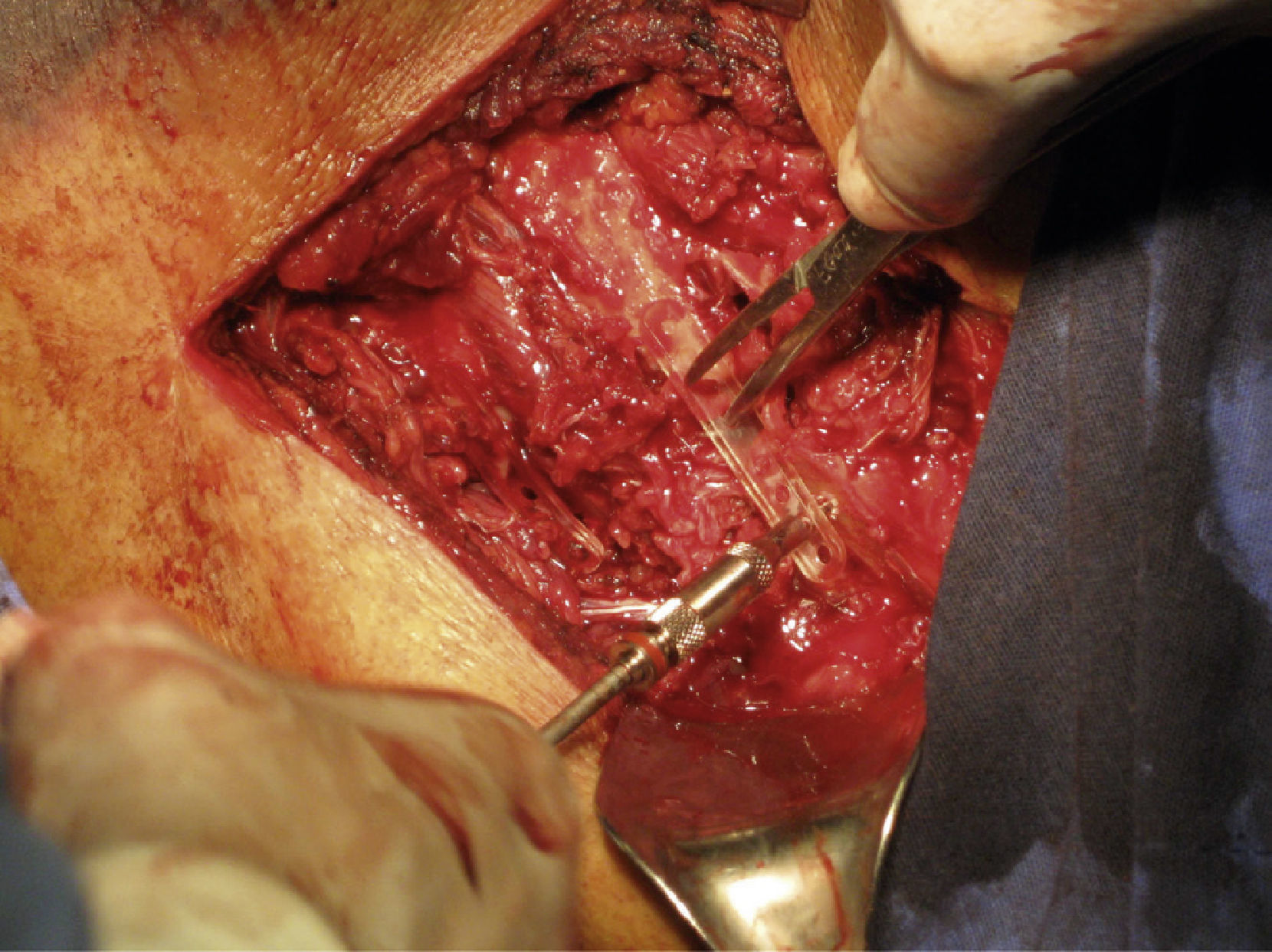
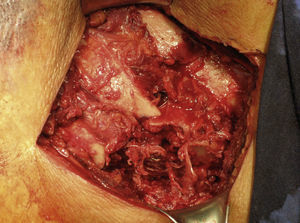
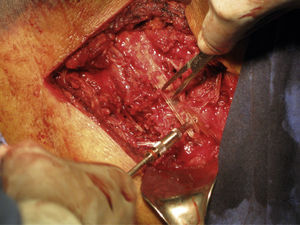
Surgical technique for fixationAn axillary mid-line incision was made in all patients. When patients presented only unilateral unstable thorax, they were placed in lateral recumbent position; in bilateral cases, an axillary incision in dorsal recumbent position (Fig. 2) and an anterior clavicular incision were made for the fixation of the chondrosternoclavicular articulation. Muscles were dissected to discover and fix the costal arches; the periosteum of the affected costal arches was removed; holes were drilled using a tap and the bioabsorbable plates and screws were placed (Fig. 3). When required, the haemothorax was evacuated before fixation and an endopleural tube was placed. In those patients who already had the tube, it was simply replaced. Haemostasis was verified, the endopleural tube was fixed to the skin, the muscles brought together after haemostasis and the Penrose was placed between the costal arches and muscles. Fat tissue and skin were brought together. No fixation was performed in the first two costal arches to prevent vascular risk, nor of the eleventh and twelfth costal arches, as they have little participation in the ventilatory mechanics. Only 4 patients were intubated due to previous instability and/or severe head injury; the rest of the patients were extubated at the end of the surgery.
All patients signed the informed consent form of the institution and provided their authorisation to perform the procedure and to participate in the study. They were informed that bioabsorbable plates would be implanted on them. The study was submitted to the Ethics and Research Committee of the hospital subsequently authorised.
ResultsEighteen patients were reported, 16 males and 2 females, with ages ranging from 33 to 74 years and a mean age of 53 years. The cause of trauma in 15 patients was pedestrian-motor vehicle collision; 4 patients presented left humerus fracture, sternal fracture was associated in 3 patients and sternal fracture-dislocation in 1; 3 patients presented bilateral flail chest, one of which had an upper sternal fracture and bilateral sternoclavicular dislocation; another patient presented patellar and tibia fractures contralateral to the unstable thorax and 2 of those patients with bilateral flail chest also presented scapula fracture; 2 of the 18 patients presented acute abdomen, which was solved at the initial treatment, both underwent splenectomy; 2 patients presented associated moderate to severe head injury and one patient also had influenza A (H1N1). Four of the 18 patients required orotracheal intubation, 2 of them due to the state of shock and the other 2 due to the head injury. The period of intubation did not exceed 7 days, except for one patient who required intubation for 22 days (with severe head injury and humeral fracture), who underwent a tracheotomy. Ten patients presented mediastinum trauma, with minimum pericardial effusion; all of them developed pulmonary and cardiac contusion.
The initial management consisted of clearing the respiratory tract and assuring ventilation by placing an endopleural tube in the 16 cases that required it, orotracheal intubation in the 4 cases that required it and exploratory laparotomy to control abdominal haemorrhages in 2 patients, with splenectomy conducted in both. Furthermore, all patients were administered analgesics for pain management and to reduce breathing effort, complementary oxygen support with Puritan system at 35%, micronebulisation with steroids and bronchodilator, antibiotics, diuretics for the management of the mediastinum trauma, reduction of oedema and prevention of vena cava syndrome, management of the pericardial and alveolar effusion, and low molecular weight heparin to reduce the risk of pulmonary thromboembolism. Only six patients required pressor amines like dopamine, at 5 gammas during an average of three days, ranging from two to seven days. The APACHE II classification was 6-17 points, with an average of 10.
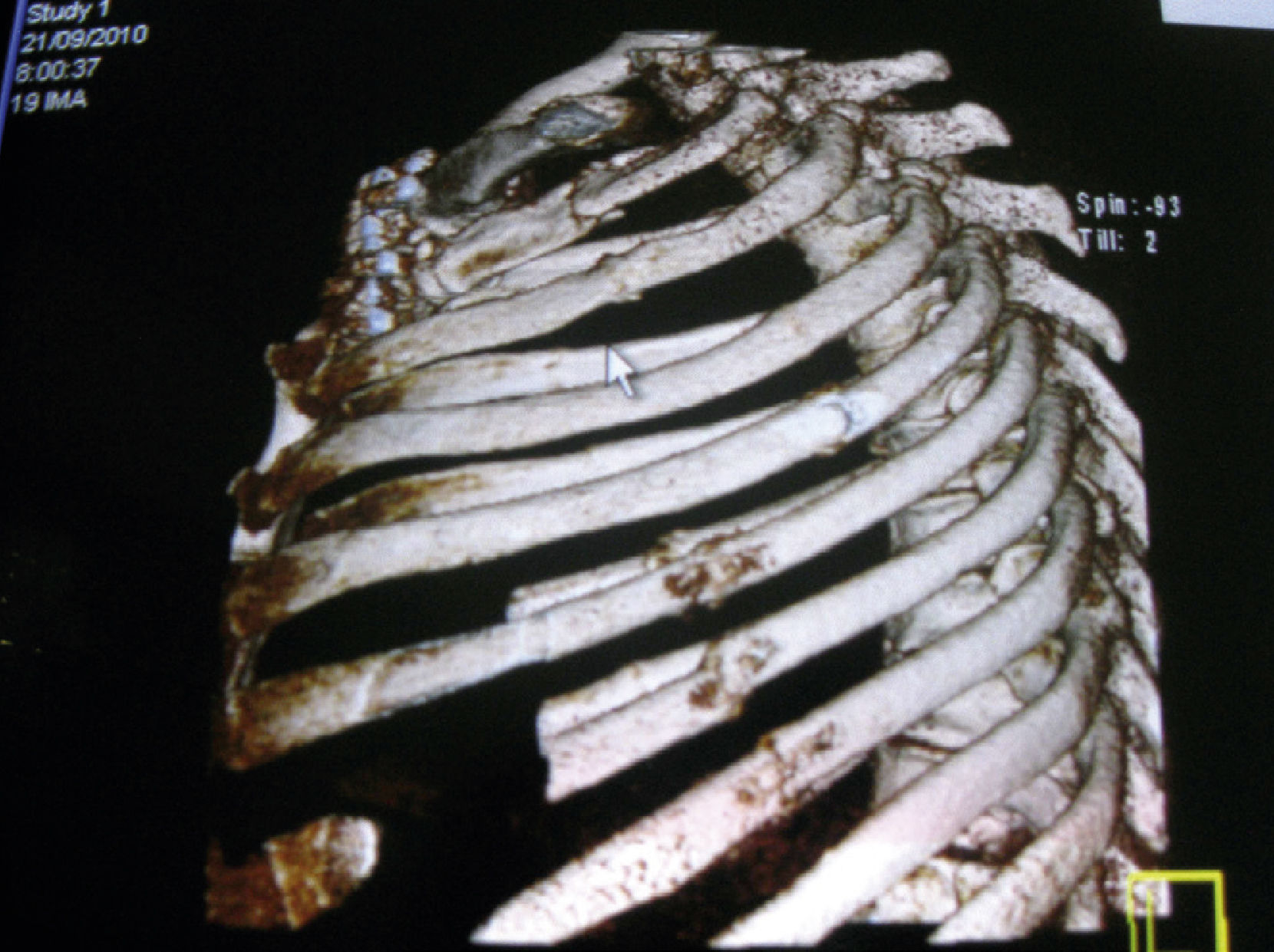
Six patients were diabetic and two had chronic hypertension. All patients were metabolic and haemodynamically stabilized and the fixation surgery was performed between 1 and 21 days (patients who were operated at day 11 and 21 were admitted in other departments of the hospital) with a mean of 1.5 days; 2 patients with bilateral injury underwent bilateral rib fixation at the same time (Fig. 3) with bilateral axillary incision in dorsal recumbent position; the rest of the patients were placed in lateral recumbent position; an axillary incision was made with anterior and posterior dissection (Fig. 4); the patient who presented bilateral sternocostoclavicular dislocation underwent fixation of the dislocation with titanium plates. Two of the four patients with humerus fracture underwent fixation for said fracture during the same procedure as the other fixations required.
There were no deaths during the study; there was a wound infection in a diabetic and obese patient who underwent bilateral rib fixation as well as fixation of the sternoclavicular articulation. The infection was treated with dressings and quinolone for 10 days. Patients with head and abdomen trauma were intubated for a period of no more than seven days, with the exception of the patient with severe head injury, who required a tracheotomy due to prolonged intubation. The rest of the patients were intubated only for surgery and were extubated when the surgery was finished; the plates did not need to be removed, the paradoxical motion stopped and pain was more tolerable after fixation. The visual analogue pain scale moved from 9 before surgery to 3-4 after fixation; it was possible to practice ventilatory exercises and the patient's capacity to expectorate improved; the heart rate and respiratory rate diminished after fixation, from a mean of 90 beats per minute (ranging from 82 to 100) and 26 inspirations per minute (ranging from 22 to 28 per minute) before surgery to a mean of 84 beats per minute and 22 inspirations per minute during the postoperative period.
Patients were assessed (Fig. 4): a thorax teleradiography and a lateral hemithorax teleradiography were performed on all of them, one month and five months after fixation, as well as a tomography for monitoring (Fig. 5); in the areas where discrete costal separation was observed due to bone loss caused by the injury, an adequate consolidation was finally confirmed. When there were associated sternal fractures and sternocostoclavicular dislocations, fixation of sternal fracture and dislocation was performed with titanium plates and the rib fixation was made using bioabsorbable material without any problems. In the postoperative period, normal wandering initiated the following day, whenever possible; the mean length of hospital stay after surgery was 4 days, ranging from 3 to 25 days (patients with head injury). During the fixation procedure, drainage of haemothorax was performed in two patients who required it.
DiscussionFlail chest has a high mortality rate (16.3%); the degree of severity is related to underlying pulmonary and myocardial contusions as well as the pain caused by rib fractures and not necessarily by the thorax instability itself or the paradoxical respiration. Therefore, a careful selection of the patients must be conducted to determine who will be treated with mechanical ventilation or without it, and the decision to withdraw this complementary treatment at the earliest convenience to avoid greater complications. Regarding the abovementioned information, only those patients presenting a state of shock caused by intra-abdominal injuries and those with severe head injury were mechanically supported; for the rest of the patients, management without ventilatory support was possible and only the pain, the mediastinal and pulmonary contusions were treated. Fluid management improved the quality of bronchial secretion, kept the airway open and reduced oedema. All of this compensated the physiopathology of the flail chest.
The indication for rib and sternal fracture fixation was made only when the patient presented flail chest; the objective of this procedure was to improve the respiratory mechanism, diminish the pain and reduce the return-to-work time, which was achieved, as four years after the beginning of the study no deaths, plate removals or rejection of plates have been reported, which demonstrates that the cost-benefit ratio is lower, as compared to other metallic materials, and that the use of bioabsorbable material favoured the harmony in the ventilation mechanism with sufficient tension and without the rigidity of the metallic materials.
Although it increases the cost of the procedure, conservative management, if applied, would increase the length of hospital stay and the return-to-work time, which would raise the cost-benefit ratio, without adverse effects attributable to the material used.
On the other hand, the patients presenting four or less rib fractures in a single place were not submitted to rib fixation and only an endopleural tube was placed for pneumothorax or haemothorax drainage, as the case may have been. Pain management was also conducted, together with fluidification of the bronchial secretions; antibiotics were administered and complementary oxygen was provided when needed. However, despite the fact that they did not present flail chest, recovery time was longer, as the rib pain remained for a longer time and the return-to-work time was at least 15 more days (in contrast with those who underwent rib fixation and who did not present concomitant limb injuries). Thus, in patients with flail chest, the length of hospital stay and the cost for the institution for the longer time of labour disability would have increased, as well as the complications for prolonged length of hospital stay, poor management of the secretions, often times associated with pain and alterations in the respiratory mechanics. All these aspects show the importance of rib fixation with a bioabsorbable material that does not need to be removed, and which presents minimum inflammatory reactions.
Level of evidence4th Level of evidence.
FundingThere was no defined source of funding for this study; the funding came from the institution itself, which is a governmental institution.
Conflict of interestThe authors declare that there are no conflicts of interest.
Please cite this article as: Barrón-Torres et al. Perfil clínico-epidemiológico de las fracturas supracondíleas de húmero en pacientes pediátricos en un hospital general regional. Cirugía y Cirujanos. 2015; 83: 29-34.
Corresponding author. Calle 34N. 439 por 41, Ext Terrenos el Fénix. C.P. 97150. Mérida, Yucatán. México. Teléfono: +5299 9928 5656, ext.: 62314.