Central venous catheters are devices used for therapeutic, diagnostic, and monitoring purposes. Complications associated with central venous catheter use include those related to their insertion, rupture and displacement of the catheter, occlusion, thrombosis, and infection. Of these the latter is important due to the high morbidity and mortality it causes in the patients, and total parenteral nutrition increases the risk. The aim of this study is determine the incidence and risk factors associated with catheter-related infection in patients on parenteral nutrition.
Material and methodsA retrospective, observational, and cross-sectional study was conducted, by analysing patients on total parenteral nutrition who developed a catheter-related infection in a 6-month period. Multiple variables were studied, looking for significance. A statistically significant relationship was considered with a p<0.05.
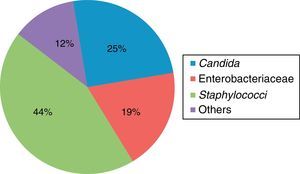
ResultsThe study consisted of 85 patients, of whom 52% were women and 48% men. The median age was 54 years. The most frequent diagnosis was enterocutaneous fistula. Catheter associated infection was present in 19% of patients. The most frequent microorganisms found were Staphyloccocus sp. (44%) and Candida sp. (25%). Median time between central venous catheter insertion and infection was 78±64 days. There was a significance between days with a central venous catheters and infection development (p=0.014). Infection developed in 81% of patients on whom surgery was performed (p<0.05).
ConclusionIt was found that patients with a longer use of a central venous catheter (p=0.014) and those who were operated on in conjunction with total parenteral nutrition (p<0.05) were more prone to develop a catheter-associated infection.
Los catéteres vasculares centrales son dispositivos que permiten el acceso al torrente sanguíneo con fines diagnósticos, terapéuticos y de monitorización. Las complicaciones por su uso incluyen las asociadas a su inserción, rotura o desplazamiento del catéter, oclusión, trombosis e infección. Esta última aumenta la morbimortalidad y el uso de nutrición parenteral aumenta el riesgo.
El objetivo de este estudio es determinar la incidencia y los factores de riesgo relacionados con infección asociada a catéter venoso central, en pacientes con nutrición parenteral total.
Material y métodosEstudio retrospectivo, observacional y longitudinal. Se analizó a pacientes con nutrición parenteral que desarrollaron infección asociada a catéter, durante 6 meses. Se analizaron diversas variables en busca de significación estadística; esta se consideró con una p<0.05.
ResultadosSe revisaron 85 expedientes; el 52% fueron mujeres y el 48%, hombres. La edad media fue 54 años. El diagnóstico más frecuente fue fístula enterocutánea. El 19% de los pacientes desarrolló infección. Los microorganismos más frecuentemente asociados fueron: Staphylococcus sp. (44%) y Candida sp. (25%). El promedio de días entre la colocación de catéter e infección fue 78±64 días. Se encontró significación estadística entre los días con catéter y el desarrollo de infección (p=0.014). El 81% de los pacientes que presentaron infección eran postoperados (p<0.05).
ConclusiónEncontramos que los pacientes con más días de uso de catéter central (p=0.014) y el hecho de estar postoperado y con nutrición parenteral (p=0.05) aumentan el riesgo de presentar infección asociada a catéter, por lo que debe tenerse una mayor vigilancia en estos pacientes para prevenir esta complicación.
Central venous catheters are devices used to gain access to the bloodstream, either for diagnostic or therapeutic purposes, drug administration, total parenteral nutrition or haemodialysis. They are also an invasive cardiovascular monitoring device. It has been estimated that over 80% of hospitalised patients need an intravascular catheter, inserted either peripherally or centrally, during their hospital stay.1,2 The most common approach for central venous catheters are through the subclavian, jugular or femoral vein.3 Approximately 150 million catheters are inserted each year in the USA and of these 5 million are central venous catheters.4
Complications associated with central venous catheter use are common and include those associated with insertion (pneumothorax, vascular injury, cardiac arrthythmias, cardiac perforation with clogging, air embolism, nerve injury or anomalous location of the catheter), rupture or accidental displacement of the catheter, occlusion, thrombosis and infection.5,6 Of these the latter is important due to the high morbidity and mortality it causes in the patients, increasing hospital stay and consequently healthcare costs.7,8 The Centre for Disease Control stated there was a bloodstream infection rate in intensive care units of 4.9–11.9 cases per 1000 central venous catheters inserted within a 5-year period.9 A Spanish study on the prevalence of nosocomial infections in 2010 also demonstrated that the bacteremia related to the catheter is the fourth most common nosocomial infection, with prevalence at around 2 episodes for every 100 patients with a central venous catheter.10
Bacterial colonisation of the catheter generally comes from the skin or where it comes into contact with it and is related to factors such as: the catheter material, location (higher incidence in femoral catheters), the number of lumen, time of usage and patient characteristics.11 The administration of total parenteral nutrition increases the risk of bacteremia or local infection.12 Diagnosis of bacteremia associated with a catheter requires isolating the causal microorganism in a peripheral blood culture and a central blood culture or in one segment of the catheter.13 The microorganisms most common associated with bacteremia are Staphylococcus epidermidis, Enterobacter spp., Escherichia coli, Klebsiella pneumoniae, Pseudomonas aeruginosa, Staphylococcus aureus, Enterococcus (E. faecalis, E. faecium) and Candida albicans.14,15 When a patient receiving total parenteral nutrition has a fever the central venous route should always be a suspected cause of infection and it would therefore be necessary to suspend the total parenteral nutrition, take blood cultures and rule out other possible focus points including: respiratory, urinary, and surgical wound site.16
The aim of this study is determine the incidence and risk factors associated with central venous catheter-related infection in patients on parenteral nutrition in a third level hospital.
Material and methodsA retrospective, observational, and cross-sectional study was conducted, by analysing patients on total parenteral nutrition who developed a catheter-related infection, in the Hospital de Especialidades del Centro Médico Nacional Siglo XXI, between 1st January 2015 and 31st March 2015.
Total confidentiality of data obtained was maintained. The following variables were analysed: age, gender, comorbidities, service treating them, albumin, length of hospital stay, diagnosis on admittance, days with total parenteral nutrition on diagnosis of the infection, isolated microorganism, days with central venous catheter. The number of days with a central venous catheter and the total parenteral nutrition on diagnosis of infection were also analysed.
Descriptive analysis was made using frequencies and percentages for categorical qualitative variables. For quantitative variables the means and standard deviation were estimated, when the data curve was symmetrical. When this curve was not symmetrical it was analysed using medians and ranges. A statistically significant relationship was considered with a p<0.05. Collected data was captured on the statistical package for Social Sciences for Windows (SPSS 17.0 version, Chicago, IL, U.S.A.).
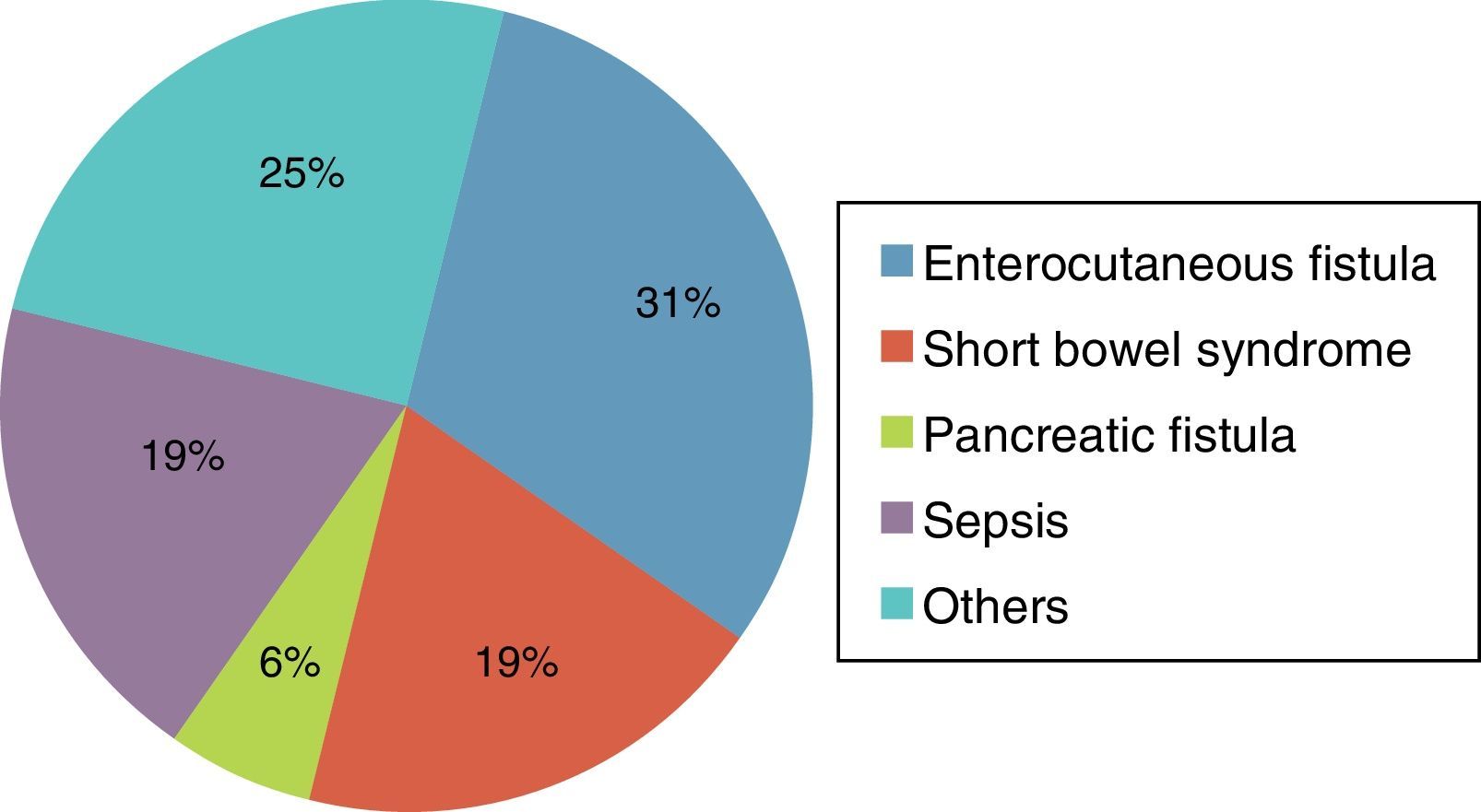
ResultsA total of 89 files were reviewed. 4 were eliminated because no complete data was found or no data had been filed. Of the total patients, 52% were women and 48% were men. The mean age was 54 (range between 18 and 83). Most patients were hospitalised in the Gastrosurgical Department (85%), followed by the departments of Internal Medicine (6%) and haematology (4%). The most common diagnosis was enterocutaneous fistula (23 patients). The remaining diagnoses are listed in Fig. 1. Out of the total patients, 16 (19%) presented with central catheter associated infection. The mean age of this group was 50 (range between 19 and 56).
The average albumen in infected patients was 2.9±0.8g/dl, whilst for those who were not infected it was 2.7±0.89g/dl. Statistical analysis of this variable revealed a value of p=0.41.
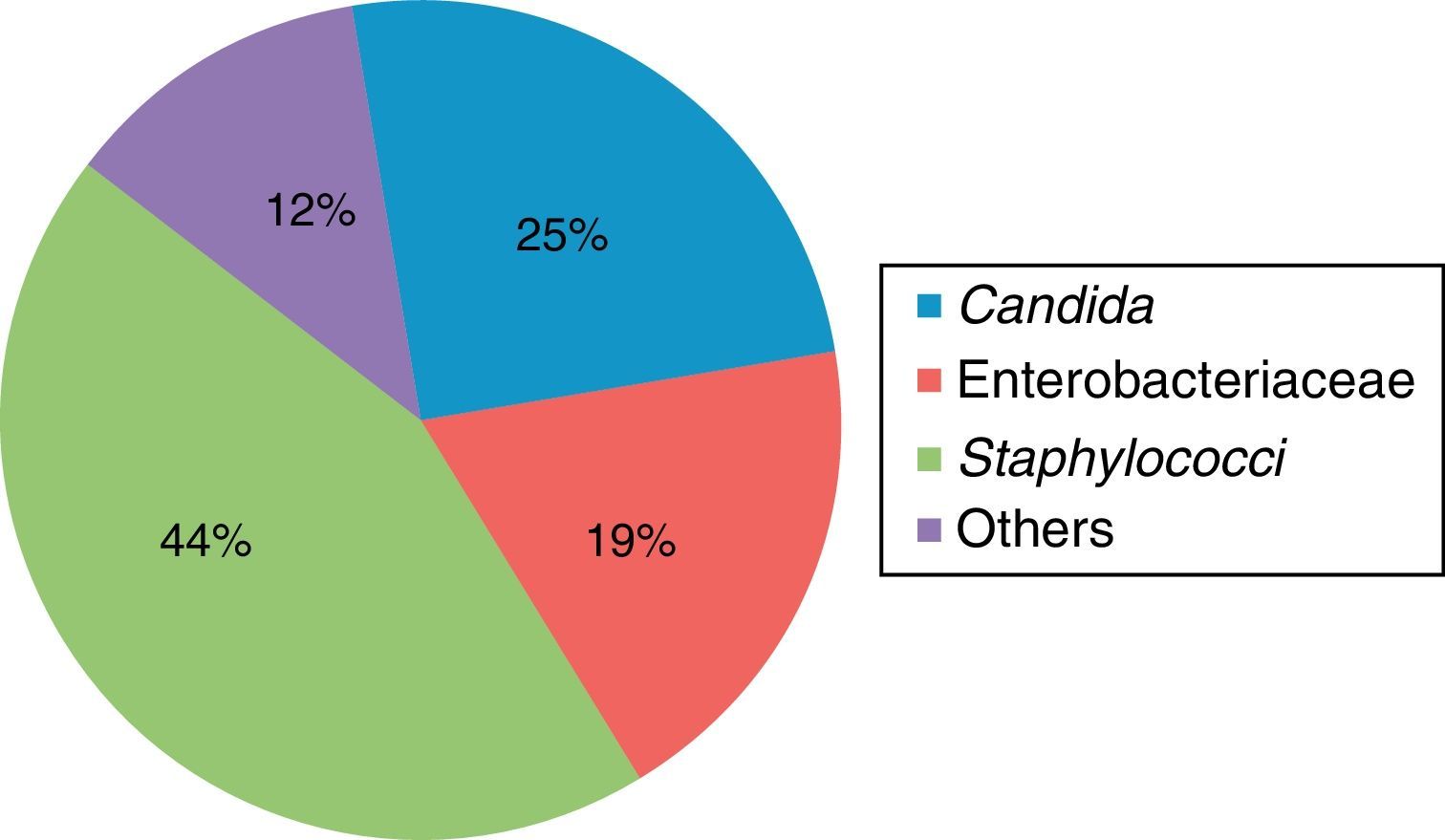
The microorganisms most frequently associated with infection were gram-positive bacteria, with a predominance of the Staphylococcus spp. at 44%, followed by opportunist microorganisms, and in particular Candida spp. in 25% of patients (Table 1 and Fig. 2).
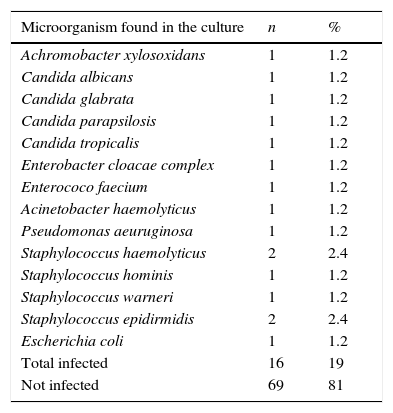
Frequency and isolated microorganism in 19 patients receiving total parenteral nutrition with catheter-associated infection.
| Microorganism found in the culture | n | % |
|---|---|---|
| Achromobacter xylosoxidans | 1 | 1.2 |
| Candida albicans | 1 | 1.2 |
| Candida glabrata | 1 | 1.2 |
| Candida parapsilosis | 1 | 1.2 |
| Candida tropicalis | 1 | 1.2 |
| Enterobacter cloacae complex | 1 | 1.2 |
| Enterococo faecium | 1 | 1.2 |
| Acinetobacter haemolyticus | 1 | 1.2 |
| Pseudomonas aeuruginosa | 1 | 1.2 |
| Staphylococcus haemolyticus | 2 | 2.4 |
| Staphylococcus hominis | 1 | 1.2 |
| Staphylococcus warneri | 1 | 1.2 |
| Staphylococcus epidirmidis | 2 | 2.4 |
| Escherichia coli | 1 | 1.2 |
| Total infected | 16 | 19 |
| Not infected | 69 | 81 |
56% of infected patients had at least one associated disease, whilst for those who were not infected there was a 36% comorbidity rate. The Chi-square test was performed and analysis showed a value of p=0.11.
The average number of days between insertion of the central venous catheter and the onset of infection was 78±64 days. Non infected patients needed central venous catheter for 34±33 days. A statistically significant relationship was found between the days with the catheter and the development of infection with a value of p=0.14. In over 50% of patients infection of the central venous catheter was reported during the first 20 days, after initiation of total parenteral nutrition. Of these patients, 22 had been treated in the Intensive Care Unit and out of the total 36% presented with catheter-associated infection.
81% of patients presented with infection associated with a catheter and were operated on again. On analysing this variable and comparing it to postoperative patients without infection there was a p value significantly lower than 0.05.
DiscussionComplications involving infections in central line access is the cause of high morbidity and mortality in hospitalised patients. Approximately 25% of central venous catheters inserted present with asymptomatic colonisation and the rate of infection varies between 7% and 42%.17,18 It is believed that many factors are involved in the physiopathology of catheter associated infection, and it may also to be noted that when a microorganism enters the bloodstream there is a trigger effect. It has been proposed that this may happen when the normal flora of the skin invade the insertion site and move around in proximal direction around the external site of the catheter up to the vascular lumen.12,19 It has been seen that the use of total parenteral nutrition increases the risk of infection associated with the catheter since the latter is the potential means of culture.20,21 In the study conducted by Marra et al.22 it was demonstrated that 80.9% of patients with prolonged total parenteral nutrition developed a bloodstream infection. In our population incidence was lower (19%), probably due to the total parenteral nutrition usage time, since in our study results were only given for 6 months.
Our study also demonstrated that patients with total parenteral nutrition and infection had required the use of a central venous catheter for almost double the amount of time as those patients with nutrition who had not developed infection (78 vs. 34 days). A statistical significance of p=0.014 was found from analysis of this variable. Given these results, it is important that a monitoring protocol be established for patients receiving total parenteral nutrition for over a month's duration, so that early identification of infection may be made and procedures such as changing the catheter or using antibiotics be performed, to reduce the rate of this complication. It is striking that the majority of patients were diagnosed with a catheter associated infection within the first 20 days, indicating that prospective studies which analyse the cost-benefit of taking a prophylactic blood culture could be beneficial against symptoms. Investigation should also be made of those patients who have a central venous catheter for over 50 days, with a prior blood culture, to determine whether it is infected or not, prior to the commencement of the total parenteral nutrition.
Many factors have been reported to contribute to infection in patients with central venous catheters, and these include: catheter characteristics; insertion site; skill of the health care person inserting it; carrying out emergency procedures. Patient characteristics are: age, severity of the base disease, extremes of age and immunocompromise.21,23 In our series the extremes of age or gender were not shown to increase the risk of infection. Furthermore, it is interesting that of the infected patients 56% had at least one associated disease. A further, broader study could be made with a sub-analysis of specific comorbidities to identify risk factors for infection in our hospital. What is striking in our sample is that a risk factor related with infection was that the patient was postoperative. This factor is probably explained by the fact that these patients present a metabolic trauma response, which reduces their immunological status and increases the development of complications.
Another factor associated with the increase in the rate of catheter-associated infection in patients who were receiving total parenteral nutrition is how long they were in the ICU.23 In 2003, the Centro para el Control y Prevención de Enfermedades published a report that 55% of patients hospitalised in the ICU had a central venous catheter, compared with just 24% of patients in other areas of the hospital. This factor increases catheter-associated infection risk rates.24 Our study sample did not show an increase in the rate of frequency of this complication.
Lastly, the aetiological agents most commonly related to catheter-associated bacteremias, in order of frequency, are: coagulase-negative straphylococci (primarily S. epidermidis) at 36%, enterococci at 16%, gram-negative aerobic bacilli (P. aeruginosa, K. pneumoniae, E. coli) at 16%, S. aureus at 13%, Candida spp. at 11% and other microorganisms at 8%.25,26 As mentioned in the literature, in our study there was a predominance of coagulase-negative straphylococci and types of Candida, which led us to believe that the normal flora of the skin is the initial starting point of this type of infection. A correct asepsis and antisepsis procedure prior to the insertion of any central venous catheter is therefore important.
Central venous catheter infection in patients receiving total parenteral nutrition is a risk for those patients. The incidence in our study was 19% compared with the 42% reported in the literature. We found that a longer time of central venous catheter (p=0.014) usage and when the patient was postoperative (p=0.05) were factors with an increased risk in presenting this complication. Increased patient monitoring should be made for patients with these risk factors.
This study may act as guide for a broader study with greater follow-up time, to determine further risk factors and hazards to be considered for the implementation of new and better strategies for nosocomial infection care from valuable, costly products such as those associated with total parenteral nutrition.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors have no conflict of interest to declare.
Please cite this article as: Parra-Flores M, Souza-Gallardo LM, García-Correa GA, Centellas-Hinojosa S. Incidencia de infección asociada a catéter venoso central y factores de riesgo relacionados en pacientes con nutrición parenteral total en un hospital de tercer nivel. Cir Cir. 2017;85:104–108.