The incisional hernia continues to be a frequent complication of laparotomies. The purpose of study is the analysis of hernia disease relapse after one year after different open plasties methods of the abdominal wall.
Material and methodsA prospective longitudinal study was performed that included 142 patients. An analysis was performed on the individual data, the level of obesity, intra-surgical variations in intra-abdominal pressure, the intensity of post-surgical pain, the post-surgical complications, and the types of plasties of abdominal wall, simple and with polypropylene mesh.
ResultsThe analysis of studied group showed a general rate of relapse of 16.9%, and within the 4 procedures, 40.74% in the case of simple plasties, of 16.07% after the only plasties, 6.97% after the retro-muscular plasties, and 6.25% after the full substitution of parietal defect. On analysing the collected, hernia relapse was statistically significantly related to the level of obesity, variations in intra-abdominal pressure, post-surgical pain, and the type of procedure performed.
ConclusionsHernia is a frequent complication of laparotomies. Hernia relapse was more frequent in the case of simple plasties. Among the mesh procedures, the onlay plasty showed a higher rate of relapse and post-surgical complications. Hernia relapse was more frequent in the case of variations of intra-abdominal pressure, and with increased post-surgical pain. The use of an echography examination may increase the accuracy of the presence of hernia disease.
La hernia incisional sigue siendo una complicación común de las laparotomías. El propósito del estudio es analizar la recidiva de hernia en un año, después de varios métodos abiertos de plastia de la pared abdominal.
Material y métodosEstudio longitudinal prospectivo, en el que se incluyó a 142 pacientes. Se analizaron: los datos individuales, el grado de obesidad, las variaciones intraoperatorias de la presión abdominal, la intensidad del dolor postoperatorio, las complicaciones postoperatorias y los tipos de plastias de la pared abdominal: simple y con malla de polipropileno.
ResultadosEl análisis del grupo estudiado estableció una tasa general de reincidencia de 16.9% y, en los 4 procesos, del 40.74% en caso de plastias simples, del 16.07% después de plastias onlay, del 6.97% después de plastias retromusculares y del 6.25% después de la sustitución completa de la avería parietal. Mediante el análisis de los datos obtenidos, la recidiva de la hernia fue significativamente correlacionada con: el grado de obesidad, las variaciones de la presión intraabdominal, el dolor postoperatorio y el tipo de procedimiento realizado.
ConclusionesLa recurrencia de la hernia fue más frecuente en las plastias simples. Entre los procesos con malla, a la plastia onlay se le asignó una mayor tasa de recaídas y complicaciones postoperatorias. La recurrencia de la hernia fue más frecuente en las variaciones de la presión intraabdominal y con el dolor postoperatorio aumentado. La realización de la ecografía puede aumentar la precisión de la presencia de la hernia.
Incisional hernia is one of the most common complications of abdominal surgery. It is cited in the specialist literature with a frequency of between 2% and 11%, after primary laparotomy.1 Most develop over the first 6 months2 to 3 years after surgery.3 Bearing in mind that between 8% and 29%4 are asymptomatic, and therefore clinically undetectable, the true incidence of incisional hernias remains a subject of controversy. The main determining factors of the disorder are obesity, factors that increase intra-abdominal pressure (IAP), post-operative wound infection and the type of suture used for post-operative wound closure. Surgical treatment for the condition has changed greatly over the last decades with the appearance of prosthetic materials and laparoscopic surgery.5 However, questions remain as to the type of mesh that should be used, where we should we place it in the layers of the abdominal wall and the sort of suture materials that should be used for fixation. These questions all require more precise, better-substantiated answers.6
The purpose of this study was to analyse the rate of recurrence clinically and ultrasonically, within one year of follow-up, and the correlation of recurrence with the type of process used, variations of preoperative intra-abdominal pressure, the onset of complications, and the level of post-operative pain.
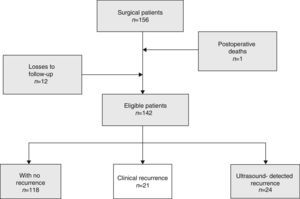
Material and methodsA longitudinal, prospective cohort study, carried out between 23 March 2012 and 30 November 2013, which included 142 patients. Before starting the study, the consent was sought of the Ethics Committee of the institution where the study was to be undertaken, the Emergency Clinical Hospital of Tirgu Mures (Condado Mures, Romania), signed by the Hospital Director and the Manager of Surgical Clinic Number 2. The document was registered in the hospital file as Number 1225/2012. All the patients included in the study gave their specific informed consent prior to surgery.
The patient inclusion criteria were: patients with primary or recurrent post-operative eventration associated with general (hypoproteinaemia, chronic cortico-steroid treatment, leukaemia) and abdominal comorbidities (abdominal cancer). Furthermore, cases of loss to follow-up were removed (Fig. 1). Various individual parameters were followed, such as: age, sex, level of obesity, body mass index (BMI) and associated comorbidities. Recorded trans-bladder indirect IAP was measured twice, at the start of surgery (IAP1) and at the end of surgery, after the plasty and skin closure, maintaining myorelaxation conditions (IAP2). The measurements were taken with a dedicated kit – ABV 611 (Fig. 2).
The types of surgery were chosen according to the size of the parietal defect, found intraoperatively. For defects under 3cm, in young patients or in patients for whom the use of prosthetic materials was contraindicated, single plasties were performed. For defects of 5–9cm, plasties with mesh in a retromuscular position were used, using the eventration sac for protection of the viscera and, for defects of 10cm, full substitution of the parietal defect. Postoperative pain was assessed using a visual analogue scale (VAS) in 6 steps.
General and local postoperative wound complications were followed up in all the patients, both on discharge and in the post-operative checks. Recurrence was evaluated 12 months after surgery, clinically and ultrasonically, recalling the patients and carrying out standard monitoring. All the patients included in the study were given antibiotics on the day of surgery and 2 days after surgery.
Description of the surgical techniquesSimple plasty of the abdominal wall was performed using a single suture or superimposing the edges of the abdominal muscle wall.
Supraaponeurotic positioning of polypropylene mesh was used to perform the simple plasty. After supraaponeurotic suturing of the muscle edges, with thick monofilament sutures of thickness 1 or 2, in order to close the defect, a polypropylene mesh was applied using the on-lay technique. The size varied from between 15cm and 20cm in width and from 25cm to 35cm in length. The method of fixing the anterior lamina of the right abdominal sheath was using multiple separate non-absorbable prolene 2/0 monofilament sutures. At all times the sides of the mesh covered at least a lateral 4cm of the right abdominal muscles. Inferior fixation had to include suturing of the mesh on the surface of the pubic symphysis. The on-lay technique was always followed by active supraaponeurotic suction drainage.
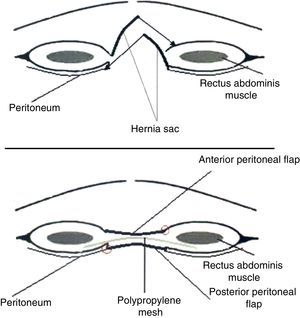
The third procedure comprised placing the mesh on the right abdominal sheath, behind the muscles. For reconstruction of the right abdominal sheaths, through both the anterior and the posterior lamina, the hernia sac was also used in order to allow suturing without tension: this is why we avoid calling it the inlay procedure and we use the term “retromuscular plasty”. Through a minimum lateral dissection of the edges of the defect, the sheaths of the rectus abdominal muscles were opened as follows: on one side of the wound, an incision was made in the anterior lamina and the retromuscular plane entered, keeping the posterior lamina in an inferior position and a fragment of the eventration sac. On the opposite side an incision was made in the posterior lamina, leaving the other peritoneal flap of the sac joined to the anterior lamina. In both cases, the retromuscular dissection was carried out with extreme care to protect the superior and inferior epigastric vessels, and the perforating branches. Then came the repair of the posterior lamina, also using the peritoneal flap joined with a continuous non-absorbable monofilament suture (size 1). After haemostasis the retromuscular mesh was inserted and fixed at a point with fine monofilament suture (prolene 4.0). The dimensions of the mesh varied between 25–35cm in width and 35–45cm in length. The superior fixation point was the xiphoid process, and the inferior fixation point was the pubic symphysis. Laterally, the mesh was implanted at least 4cm retromuscularly. After checking haemostasis, 2 drainage tubes were placed for 48h. The anterior lamina was reconstructed in the same way; the mesh was completely inserted in a new sheath, highly vascularised, and also protected from propagation of infection (Fig. 3).
Patients with full parietal defect substitution with polypropylene mesh were included in the substitution plasty group. The hernia sac was prepared to be inserted in the musculoaponeurotic edges, without being removed. Because the parietal defect was greater than 10cm, it was useless to attempt an onlay process or dissection of the right abdominal sheaths, due to excessive tension on the suture lines. The two peritoneal sac flaps were stitched again with continuous monofilament suture (size 2.0). The mesh was applied to the entire surface of the defect and fixed at several separate points to the musculoaponeurotic edges using monofilament suture (size 1). Supraaponeurotic drainage was carried out routinely (Fig. 4).
ResultsTable 1 presents the main statistical procedures in terms of individual factors, mean parietal defect, levels of obesity, variations in IAP, mean VAS, clinical and ultrasound recurrence, in correlation with the surgical techniques. Distribution by gender group showed the maximum incidence of the disease in women (68.21%) and by age group, at 60–70 years of age (32.95%). A total of 18 patients presented with associated comorbidities: 8 intra-abdominal neoplasms (stomach, colon, and rectum), 6 cases of connective tissue disease which required chronic corticosteroid treatment, 2 cases of nephrotic syndrome with hypoproteinaemia, and 2 cases of chronic leukaemia. Amongst the predisposing preoperative factors, obesity showed a statistically significant association with recurrence of the hernia within one year (p=0.009). The relationship between recurrence and the association of hypoproteinaemia with chronic corticosteroid treatment did not show statistically significant differences compared with the group with no comorbidities (p=0.244). By contrast, the presence of intra-abdominal neoplasms resulted in a significant increase of recurrence (p<0.001). By analysing the variations in IAP at the beginning and at the end of the operation, it was found that the retromuscular and substitution plasty procedures, considered tension free, significantly correlated with the simple and onlay plasty procedures. Therefore, it was established that between simple plasty and onlay plasty there are no statistically significant differences in IAP variation (p=0.058), but between retromuscular and substitution plasties, on the one hand, and simple and onlay plasties, on the other, the IAP varied in a statistically significant way (p<0.0445). By contrast, between retromuscular and substation plasties, the differences were not statistically significant (p=0.257) (Table 2). Furthermore, the 4 types of procedures could significantly correlate with recurrence of the hernia (p=0.01). Post-operative pain was a major predictor of postoperative tension and recurrence. Therefore, on analysing the pain of hernia recurrence, there was a statistically significant association (p<0.001) (Table 3).
Correlations between medium parietal defect, obesity, IAP, evaluation of pain and the number of relapses in relation to the surgical technique.
| Types of plasty | n | MPD | Obesity | IAP2–IAP1 | VASm | Clinical recurrences (%) | Ultrasound-detected recurrences Total n % | ||
|---|---|---|---|---|---|---|---|---|---|
| I | II | III | |||||||
| Simple plasties | 27 | 2576 | 10 | 5 | 0 | 2.254 | 3.623 | 9 (33.34) | 11 (40.74) |
| Onlay plasties | 56 | 3636 | 23 | 7 | 3 | 3.425 | 2.886 | 8 (14.28) | 9 (16.07) |
| Retromuscular plasties | 43 | 6245 | 10 | 15 | 8 | 0.168 | 0.862 | 3 (6.97) | 3 (6.97) |
| Substitution plasties | 16 | 12,470 | 3 | 4 | 5 | 1 | 1.187 | 1 (6.25) | 1 (6.25) |
| Total | 142 | – | 46 | 31 | 16 | – | – | 21 (14.78) | 24 (16.90) |
MPD: medium parietal defect; VAS: visual analogue scale; IAP1: initial intraabdominal pressure; IAP2: end intra abdominal pressure.
In bold, the total number of recurrences.
Statistical comparisons between the surgical procedures with IAP2–IAP1 as the variable.
| IAP2–IAP1 | Simple plasties | Onlay plasties | Retromuscular plasties | Substitution plasties |
|---|---|---|---|---|
| Simple plasties | – | 0.058 | 0.0037 | 0.0445 |
| Onlay plasties | – | <0.001 | <0.001 | |
| Retromuscular plasties | – | 0.257 |
IAP1: initial intraabdominal pressure; IAP2: end intraabdominal pressure.
In bold, statistically significant data.
Comparisons of the surgical procedures with the variable of pain assessment on the visual analogue scale.
| VAS | Simple plasties | Onlay plasties | Retromuscular plasties | Substitution plasties |
|---|---|---|---|---|
| Simple plasties | – | 0.026 | <0.001 | <0.001 |
| Onlay plasties | – | <0.001 | <0.001 | |
| Retromuscular plasties | – | 0.254 |
VAS: visual analogue scale.
In bold, statistically significant data.
The total post-operative complications were found in a proportion of 19.01%. Of these, 6.33% were general extraabdominal complications (bronchopneumonias, cerebro-vascular accidents and pulmonary emboli, which resulted in one death) and 1.40% intra-abdominal complications (intestinal obstruction and haemoperitoneum). In general, the postoperative complications resulted in a significantly greater number of recurrences (p=0.03). Analysing wound infection separately, this significantly increased the recurrence of hernia disease (p=0.01). An important factor contributing to complications was neoplastic disease, 1 case of thromboembolism and 2 wound infections (Table 4).
Postoperative complications.
| Postoperative complications | Simple plasties | Onlay plasties | Retromuscular plasties | Substitution plasties | Total |
|---|---|---|---|---|---|
| General complications | 2 | 5 | 0 | 2 | 9 |
| Intraabdominal complications | 0 | 2 | 0 | 0 | 2 |
| Supraaponeurotic haematoma | 1 | 2 | 0 | 0 | 3 |
| Supraaponeurotic seroma | 1 | 3 | 1 | 1 | 6 |
| Intraparietal haematoma | 0 | 0 | 1 | 0 | 1 |
| Wound infection | 2 | 3 | 0 | 1 | 6 |
| Total | 6 | 15 | 2 | 5 | 27 |
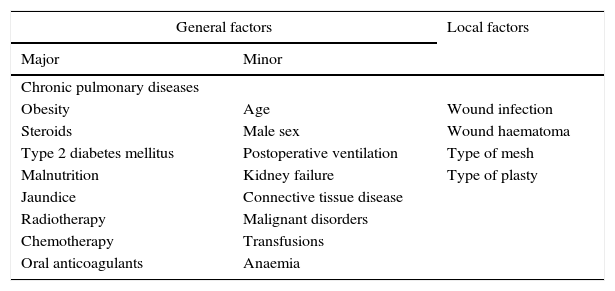
There are many studies in the specialist literature which highlight the common factors of the onset of incisional hernia. These are general7 and local. Postoperative wound infection substantially increases the incidence of the disease, and is considered the most important factor (Table 5). Carrel8 was the first to describe the relationship between wound infection and the onset of a hernia. Bucknall et al.9 demonstrated that 48% of patients with postoperative wound infection developed a hernia. In our study, wound infection was a major, statistically significant factor contributing to recurrence, of the 6 cases of wound infection, 5 presented hernia recurrence. In traditional surgery, the mid-line incision is the easiest, as it provides adequate exposure, irrespective of the disease, and because there is the least blood loss; therefore it is the most used.10
General and local predisposing factors of hernia recurrence.
| General factors | Local factors | |
|---|---|---|
| Major | Minor | |
| Chronic pulmonary diseases | ||
| Obesity | Age | Wound infection |
| Steroids | Male sex | Wound haematoma |
| Type 2 diabetes mellitus | Postoperative ventilation | Type of mesh |
| Malnutrition | Kidney failure | Type of plasty |
| Jaundice | Connective tissue disease | |
| Radiotherapy | Malignant disorders | |
| Chemotherapy | Transfusions | |
| Oral anticoagulants | Anaemia | |
Other research studies have looked at repair of the linea alba. Tera and Aberg11 demonstrated that sutures placed widely up to the edges of the abdominal rectus muscles were followed by a lower number of incisional hernias than sutures placed directly through the linea alba, which is a weak structure that predisposes to spontaneous hernia and diastasis. Lateral paramedian incisions were followed by lower morbidity compared to mid-line incisions, in a study by Cahalane et al.12 on a total of 1203 patients. With regard to transverse or even oblique incisions, outcomes are controversial in terms of the onset of incisional hernia.13 However, in the last 3 cases of patients included in the study, the greatest disadvantage was exposure of the inferior part of the peritoneal cavity and denervation, followed by weakening of the muscles.14 In the patients included in the study, since mid-line incisions were performed in almost all cases, only two being subcostal and one lateral, we cannot reach statistically significant conclusions about hernia recurrence according to the type of incision.
The way the abdominal wall is closed is another factor to distinguish hernia morbidity. The consequence of with continuous double loop suture is a slight increase in IAP. In a study by Niggebrügge et al.15 in which they compared morbidity after closure with continuous suture with morbidity after closure with separate sutures, the continuous suture technique was followed by a greater number of early wound dehiscences, and a higher incidence of hernia. However, if the continuous method is chosen for closing the abdominal wall, it is recommended that nonabsorbable monofilament sutures are used, and if interrupted closure is preferred, absorbable sutures should be chosen.16 Continuous, double loop, monofilament sutures were used on the patients in the study who underwent simple plasties.
The time of onset of hernia varies, according to the authors, between several months and several years. Mudge and Hughes17 demonstrated in their study that 50% of hernias appeared in the first year of follow-up and 80% in the first 3 years. Another study undertaken by Akman18 reported a 52% onset of hernias in the first 6 months, 68% in the first year and 79% in the first 2 years. Langer and Christiansen,19 and other authors,20,21 reached the conclusion that most recurrences occurred in the first 3 years, and the majority of these in the first year.
The aim in this study was to monitor recurrence over one year's follow-up. In order to increase the reliability of the diagnosis, clinical examination was backed up with ultrasound tests, which detected 3 cases that were not diagnosed clinically.
Obesity is another major risk factor in open hernia surgery; however, this risk was significantly reduced when laparoscopic techniques were introduced into medical practice. Thus, in a study by Saureland y Korenkov in 2004,22 it was demonstrated that out of a total of 160 patients followed up over 2 years, the general rate of recurrence was 11%, obesity being a statistically significant predisposing factor (p=0.03). In our study, obesity significantly correlated with recurrence of the hernia. Furthermore, a good number of the patients in the study presented varying levels of obesity (69.27%).
The difficulty in finding the “ideal” mesh has resulted in the development of the hole characteristics of compound meshes. These combine various materials and are based on the latest models of mesh. The main advantage of the compound meshes is that they can be used in the intraperitoneal space, and reduce the formation of adherences. Despite the wide availability of brands, they all still use one of the 3 basic materials: polypropylene, polyester and ePTFE.23
In plasties using mesh, irrespective of the method, polypropylene was used fixed with separate monofilament sutures. For visceral protection, in order to avoid fistulae and sores, in retromuscular and full defect substitution plasties, the peritoneum of the hernia sac was used, or suturing the omentum to the muscle/nerve edge of the wound.
Finally, a very important factor in recurrence is the type of abdominal wall plasty. In addition to technical and posttraumatic defects, the surgical techniques should include the routine use of meshes. The only exception being defects smaller than 3cm, according to Jenkins, who recommends closure using continuous suture.24 Hernia recurrence after simple repair of the abdominal wall is cited in several studies in the literature, varying between 35% and 50%. In our study, simple plasty using continuous double loop monofilament suture resulted in a greater recurrence rate (40.74%), but also in high postoperative pain intensity. Postoperative supraaponeurotic complications, although present, were fewer than with the onlay plasties. The use of meshes significantly reduced the relapse rate, but complications occurred associated with the presence of the mesh and the surgical technique employed to implant it. The onlay technique comprises implanting the supraaponeurotic mesh in order to reinforce a simple plasty. A study by Venclauskas et al.25 on 161 patients identified a relapse rate of 31% with simple sutures and of 11% for onlay positioning (p<0.05). However, in patients who underwent the onlay technique, the postoperative complications (seroma, wound infection) were significantly higher and resulted in a longer hospital stay. Kingsnorth et al.26 found the same in their study, where recurrence was very low (3.4%), but the postoperative complications increased (>10%). The results of this study confirm the data in the specialist literature, in that postoperative complications associated with the wound involved haematoma, supraaponeurotic seroma and wound infection. Furthermore, there were high levels of postoperative pain. Recurrence registered after the onlay process was 16.07%, lower than with plasties with no mesh. In all cases, recurrence after an onlay plasty occurred on the edges of the mesh, between this and the xiphoid (one case), between the mesh and the pubis symphysis (2 cases), and the remainder on the side of the mesh. In the specialist literature, the recurrence rate depends on the process used and the material used in the plasty and varies with time and from one author to another (Table 6).21,27–32
Recurrence rate reported in various studies with long-term follow-up.
| Study | Year | N. of patients | Follow-up | Type of plasty | Relapse in % |
|---|---|---|---|---|---|
| Usher VAS: visual analogue scale | 1962 | 541 | – | Marlex | 10.2 |
| Stoppa28 | 1989 | 751 | 12 years | Mesh | 6 |
| Liakakos et al.29 | 1994 | 102 | 7.6 years | Marlex | 6 |
| Schumpelick et al.30 | 1996 | 272 | 22 months | Preperitoneal mesh | 5 |
| Leber et al.31 | 1998 | 119 | 6.7 years | Mesh | 14 |
| Langer et al.21 | 2003 | 155 | 44 months | Autodermal mesh | 14 |
| Basoglu et al.32 | 2004 | 264 | – | Mesh | 6.4 |
Placement of retromuscular mesh and the use of the eventration sac to protect the viscera, proved to have better outcomes thanks to better blood supply to the area where the mesh was implanted, and therefore resulted in fewer postoperative complications.23 Vries Reilingh et al.,33 when they compared the 3 techniques (onlay, inlay, sublay), concluded that the sublay procedure was superior in terms of recurrence and complications. The lowest rate of relapse in our study was registered for retromuscular mesh placement and complete replacement of the parietal defect with mesh. Moreover, the postoperative complications were reduced and the intensity of postoperative pain was lower than that after simple and onlay plasties.
The variations of IAP in the 4 types of plasty could correlate with the extent of tension created by the sutures. Analyzing the outcomes and correlations, we can state that variations in IAP were a true indicator of the tension-free principle, with statistically significant differences between the retromuscular procedures and the replacement procedures, against procedures performed with greater suture tension, simple and onlay plasties.
The association of the comorbidities is, without doubt, a risk factor in hernia recurrence.7 In our study, hypoalbuminaemia, corticosteroid treatment, leukaemia did not significantly contribute to an increased number of recurrences or postoperative complications, probably due to the help of exclusive surgical treatment with meshes (6 onlay plasties and 4 retromuscular plasties) with the appropriate adjuvant therapy of the underlying disease during follow-up. By contrast, neoplastic disease contributed to the number of relapses, mainly the association with wasting syndrome.1 Relapse can also be explained by the plasties undertaken. The intraoperative septic time was the factor that dictated the choice of plasty in the cancer patients, which contraindicated the use of mesh in 5 cases. Postoperative wound complications were also associated with septic times and with the immunosuppression characteristic of all neoplasms.20
ConclusionsHernia is a common complication of laparotomy. The individual factors which favour the onset of relapse include obesity and the association with neoplasms. Hernia recurrence was more frequent in simple plasties than in those using mesh. Amongst the procedures using mesh, plasty had a higher rate of recurrence. Postoperative complications were generated and associated with the wound, and were more common in simple and onlay plasties. Hernia recurrence correlated significantly with greater variations in IAP and increased postoperative pain. Ultrasound might increase the accuracy of hernia diagnosis.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingThis article was published thanks to the Human Resources Development Operational Programme of the European Social Fund, 2007–2013, project Number POSDRU/159/1.5/S/136893.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Mureşan M, Mureşan S, Bara T, Neagoe R, Sala D, Suciu B. Seguimiento remoto de la recaída de hernia después de procesos abiertos de plastia de la pared abdominal–estudio prospectivo que incluye 142 pacientes. Cir Cir. 2016;84:376–383.