Breast cancer is the most common among women in our country, and its treatment is based on prognostic factors to categorise patients into different risk groups. In this study, the clinical and pathological features that play a role as a prognostic factor in a representative population with breast cancer in Mexico are described.
Material and methodsA descriptive analysis of the clinical and pathological features of women diagnosed with breast cancer, in a period from June 2005 to May 2014; registered in a database and calculated by simple frequencies.
ResultsA total of 4411 patients were included, the average age at diagnosis was 53 years, 19.7% were diagnosed by mammography screening program and 80.3% derived from any signs or symptoms. Regarding the stages at diagnosis, 6.8% were carcinoma in situ, 36% at early stages (I and IIA), 45% locally advanced (IIB to IIIC), 7.7% metastatic and 3.9% unclassifiable. A 79% were ductal histology, lobular 7.8% and the rest, other types. Of ductal carcinomas, 9.1% were grade I, 54.1% grade II, and 34.6% grade III. Regarding the biological subtypes, 65.7% were luminal, 10.9% luminal Her positive, 8.7% pure Her 2 positive and 14.6% triple negative.
ConclusionIn the present study, we described the clinical and pathologic features of a group of Mexican women with breast cancer that might reflect a national landscape, and represent the prognostic factors to determine groups of risk and treatment decisions.
El cáncer de mama es el más frecuente en la población femenina de nuestro país, y su tratamiento se basa en factores pronóstico que categorizan a las pacientes en diferentes grupos de riesgo. En el presente trabajo se describen las características clínicas y patológicas que desempeñan un papel como factores pronóstico, en una serie representativa de la población con cáncer de mama en México.
Material y métodosSe realizó un análisis descriptivo de las características clinicopatológicas de mujeres con diagnóstico cáncer de mama, de junio del 2005 a mayo del 2014, registradas en una base de datos y calculando la información por frecuencias simples.
ResultadosUn total de 4411 pacientes fueron incluidas; la edad promedio al diagnóstico fue de 53 años, el 19.7% fueron diagnosticadas mediante el programa de mastografía de pesquisa y el 80.3% derivadas por algún signo o síntoma. Con relación a las etapas al momento del diagnóstico, el 6.8% correspondieron a carcinoma in situ, el 36% a etapas tempranas (I y IIA), el 45% localmente avanzados (IIB a IIIC), el 7.7% metastásicos y el 3.9% no clasificables. El 79% fueron de tipo histológico ductal, el 7.8% lobulillar y el resto otras histologías. De los carcinomas ductales, el 9.1% fueron grado I, el 54.1% grado II y el 34.6% grado III. Con relación a los subtipos biológicos, el 65.7% fueron luminales, el 10.9% luminales Her positivo, el 8.7% Her 2 puro y el 14.6% triple negativo.
ConclusiónEn el presente estudio se describen las características clinicopatológicas de un grupo de mujeres mexicanas con cáncer de mama que pudieran reflejar un panorama nacional y que representan factores pronóstico para determinar el riesgo y la toma de decisiones terapéuticas.
Breast cancer is the most common malignant tumour in women worldwide. There were an estimated 1.67 million new cases in 2012 (25% of all cancer cases). The global incidence varies significantly, ranging from 27 cases per 100,000 women in some areas of Africa and East Asia, to 96 cases per 100,000 women in Western Europe. It is the fifth cause of death from cancer worldwide, in developing countries it is the primary cause of death from cancer in women, and in developed countries it is the second, after lung cancer.1
In Mexico, breast cancer has also been the most common cancer in the female population since 2006, when it exceeded the incidence of cervico-uterine cancer.2 According to the figures of the Instituto Nacional de Estadística y Geografía (INEGI) (National Institute of Statistics and Geography), in 2012, an incidence was reported of 26.64 cases per 100,000 women over the age of 20 years, and is the second cause of death from cancer in this same age group, at 15.4%.3
The current clinical management of breast cancer is based on a wide variety of clinical and pathological prognostic factors, from which it is feasible to establish risk groups and take individualised therapeutic decisions. These clinical and pathological features of breast cancer can vary in the different populations in relation to genetic and life-style aspects. In terms of age alone, it is reported that in Mexico and in other Latin American countries breast cancer presents 10 years earlier on average than in the developed countries. While the mean presentation age in Europe and the United States is 63 years, in our country it is 51.4 The stage at time of diagnosis, histopathological features and hormone receptor and oncoprotein expression are other prognostic factors for breast cancer. This study was approved by the internal ethics committee of the Instituto de Enfermedades de la Mama FUCAM (IEM-FUCAM) (Institute of Breast Diseases).
ObjectiveThe objective of this study is to give a detailed panorama of the clinical and pathological aspects at time of diagnosis involved in the classification and treatment of breast cancer in a Mexican population.
Material and methodsThis is a retrospective, descriptive, cross-sectional study of the clinical and pathological features of patients with a histopathological diagnosis confirming breast cancer on the database of the IEM-FUCAM. The study period was from 1 June 2005 to 31 May 2014. The database is recorded on SPSS software (IBM SPSS Statistics 19.0.1), and the results were calculated using simple frequencies.
The variables analysed were the prognostic factors for breast cancer. These have been widely described and recognised in the literature (age, clinical stage, histological type and grade, lymphovascular invasion and biological subtype). The patients’ information recorded on the database was included with all the variables, although some of the patients diagnosed in the IEM-FUCAM are covered under another healthcare institution such as the Instituto Mexicano del Seguro Social (IMSS), the Instituto de Seguridad y Servicios Sociales de los Trabajadores del Estado (ISSSTE), and others. At the cut-off date there was information on the database on 4411 patients, of whom 3738 received full medical care in the IEM-FUCAM and the remainder were referred to another medical institution to complete their staging and treatment. This is why some of the study variables are calculated with a different number of patients, the specification was made in each; similarly, there were patients who received only part of their care in the IEM-FUCAM, since they had started some treatment in a different hospital and attended to continue a different stage of their care. These patients were included provided the information on them was complete.
The study was undertaken in the IEM-FUCAM, a private not-for-profit institution with a specialist unit for the diagnosis and treatment of breast disease. The Institute has all the services for integral management of breast cancer and works in collaboration with the Comisión Nacional de Protección Social en Salud (Seguro Popular) within the guidelines of their technical protocol for breast cancer care in phases (diagnosis, surgery, chemotherapy, radiotherapy, hormone therapy, targeted therapy, palliative care and breast reconstruction).5 The IEM-FUCAM also has a breast cancer screening programme offering mammography to asymptomatic women over the age of 40 years. This study also makes a distinction between the clinical stage at time of diagnosis of the patients diagnosed through the screening programme, compared to those already diagnosed from a breast cancer sign or symptom.
ResultsData was included from a total of 4411 women with breast cancer recorded on the IEM-FUCAM database. A diagnosis of breast cancer was made in 80.3% of the cases due to the presence of a symptom (palpable tumour, nipple discharge, skin changes, etc.) that caused them to seek medical attention. The remainder, 19–7% of the patients, were diagnosed through the mammogram screening programme carried out in mobile units and the Institute's radiology department, in other words, these were asymptomatic patients.
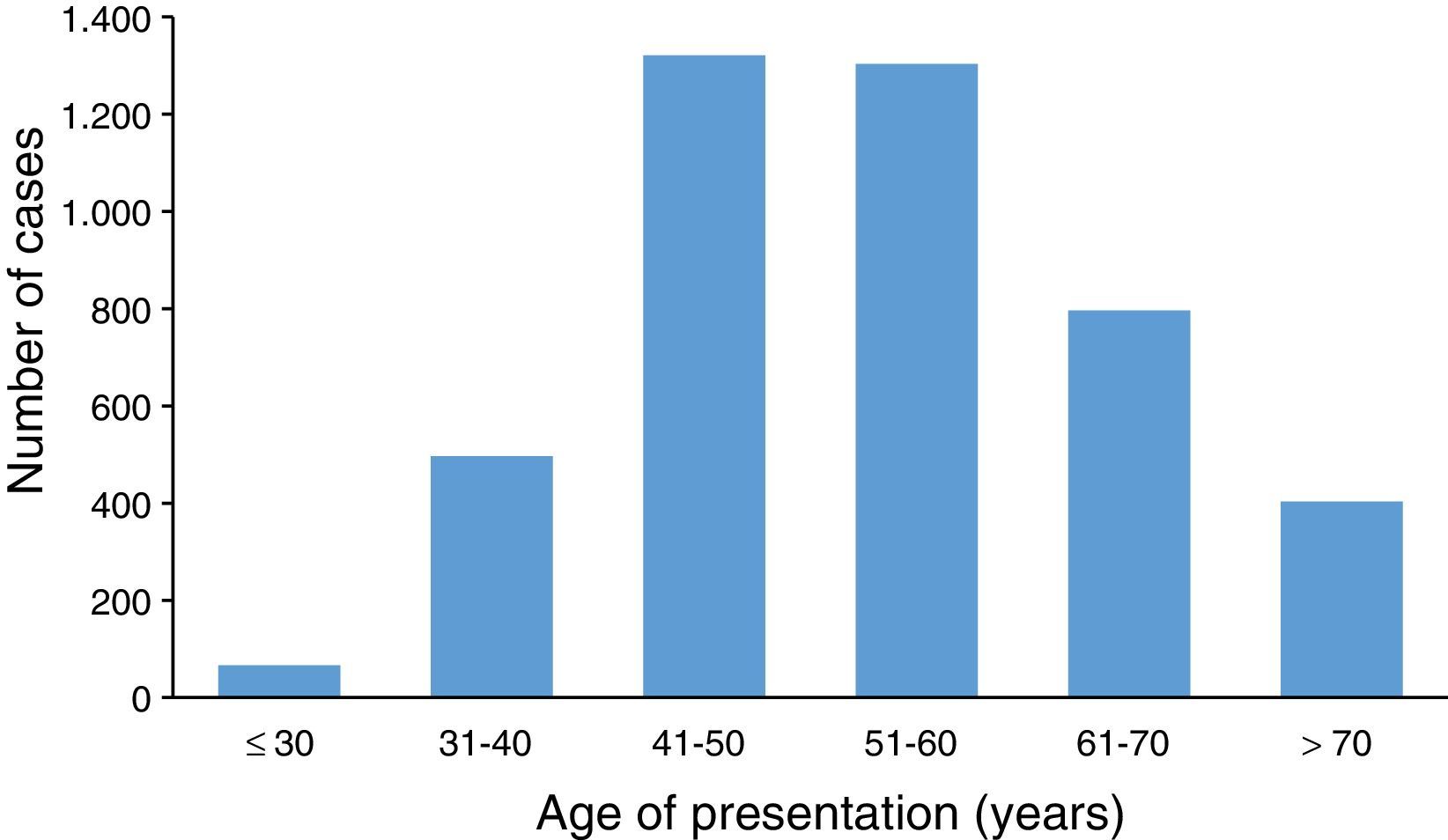
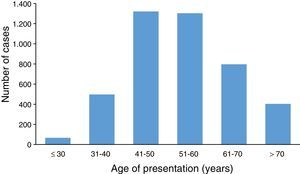
Age. We established that the average age at time of diagnosis was 53.7 years (SD±12.2 years). Fig. 1 shows the distribution by age group, the 41 to 50 year age group being the most affected, closely followed by that of 51 to 60.
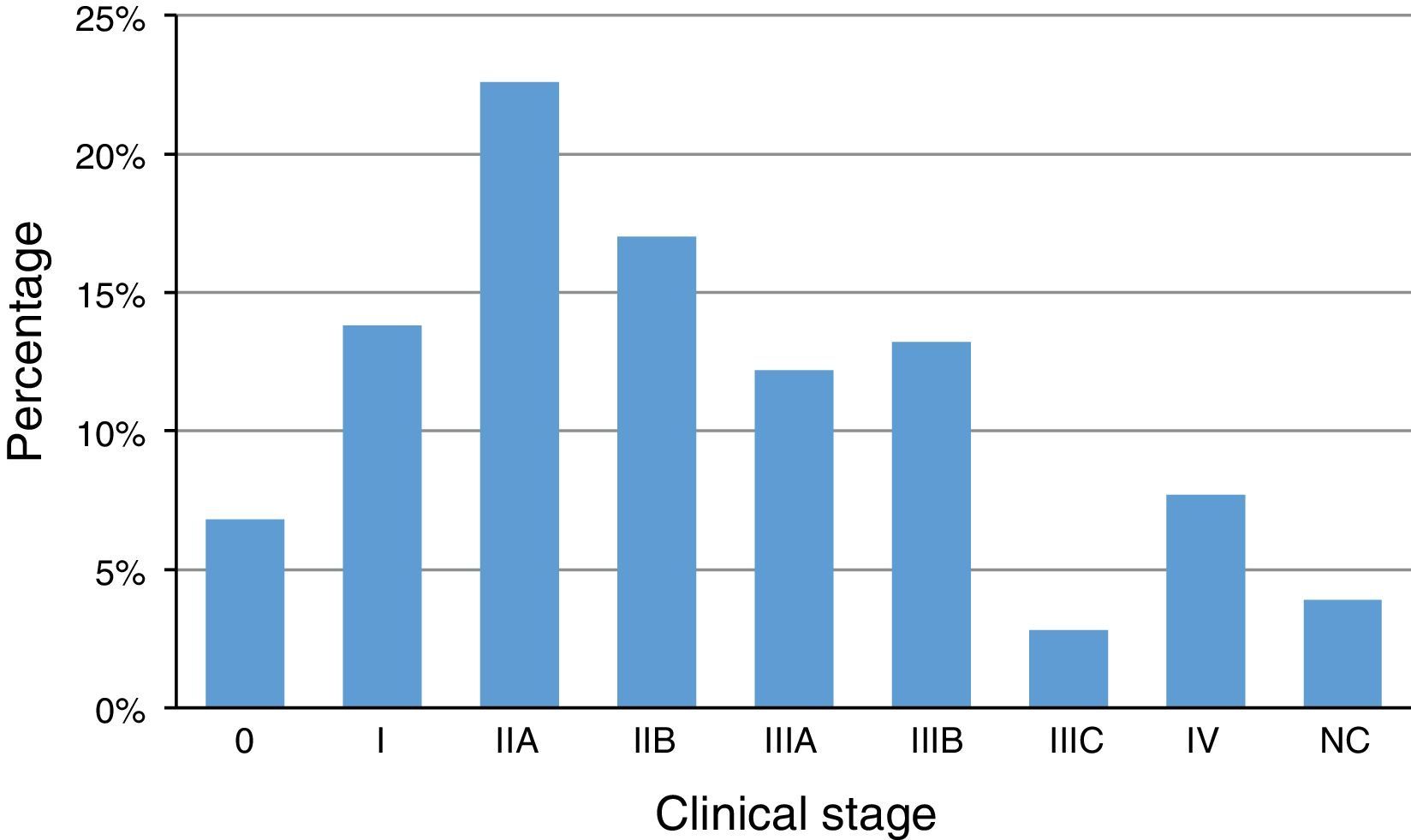
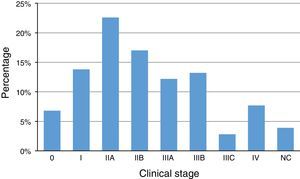
Clinical stage. In terms of clinical stage, according to the Unión Internacional Contra el Cáncer (UICC) and the American Joint Committee on Cancer (AJCC),6 at time of diagnosis, 6.8% were carcinomas in situ (stage 0), 36.4% early stage (I and IIA), 45.2% in locally advanced stages (IIB, IIIA, IIIB and IIIC), 7.7% with metastatic disease, and 3.9% were unclassifiable due to initial external management and without sufficient information to stage. Fig. 2 shows the distribution by stage.
Detailed distribution with regard to clinical stage, specifically to the characteristics of the primary tumour and also according to the UICC and AJCC's6 classification, was 6.8% Tis, 16.3% T1, 38.2% T2, 14.2% T3, 20.7% T4 and 3.8% TX; lymph node stage at the time of diagnosis was 46.2% at N0, N1 in 33%, N2 in 12.7%, N3 in 5.8% and NX in 2.3%, and assessment of remote disease, M0 in 80.7%, M1 in 7.9% and MX in 11.4%. Of the 339 patients who at time of diagnosis had distant metastatic disease (stage IV), the metastatic sites found most frequently were bone in 40.6%, followed by lung in 21.3%, liver in 11%, soft tissues in 7.6%, central nervous system in 3%, and other sites in 16.5%.
Four point six percent of the patients had bilateral breast cancer at time of diagnosis (synchronous bilateral breast cancers).
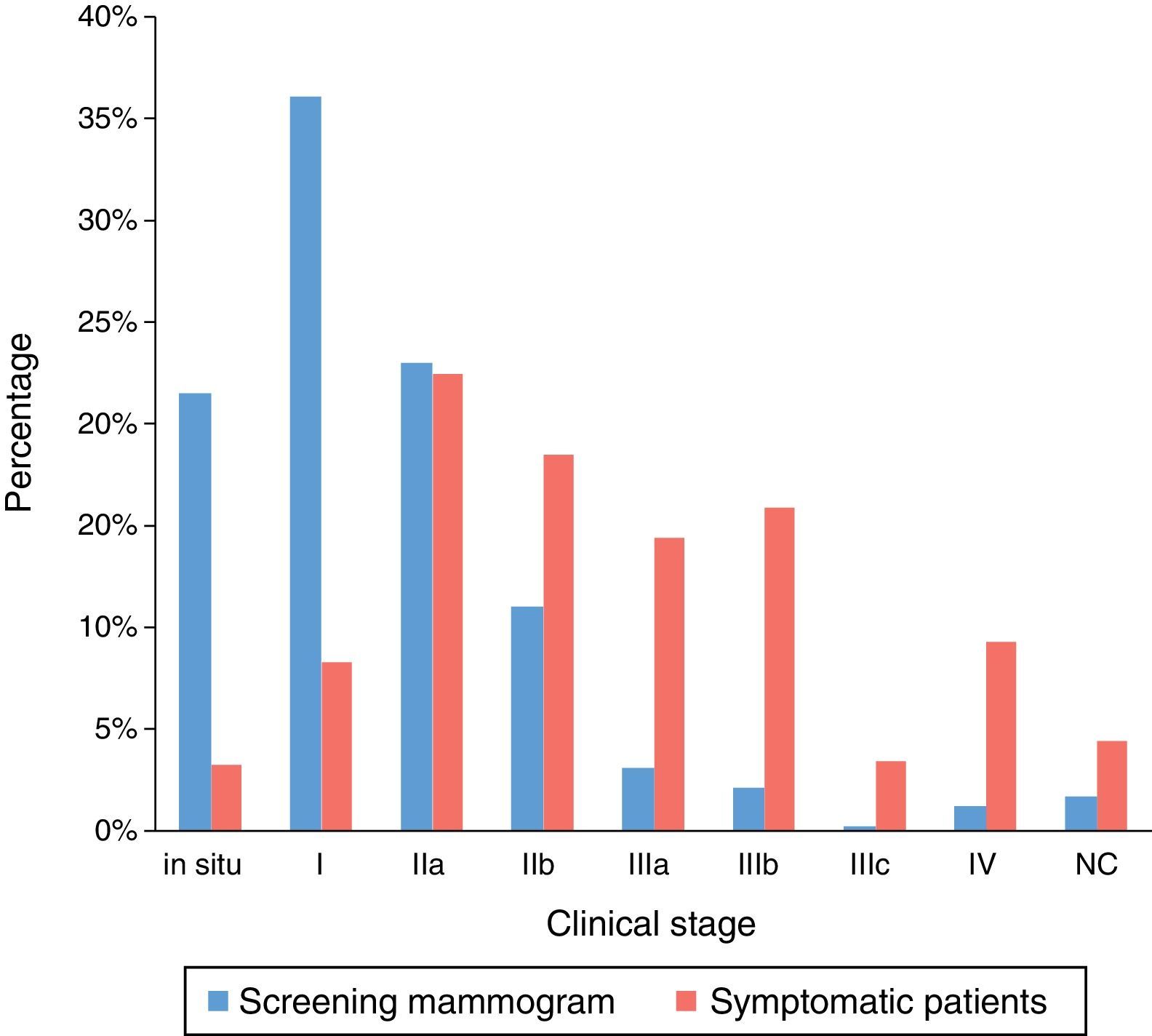
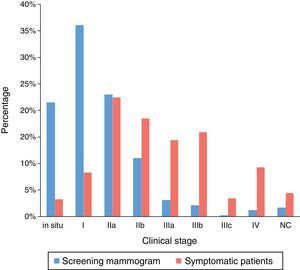
On analysing the clinical stage at time of diagnosis, making a subdivision of the patients who were diagnosed through the screening programme mammograms compared to those diagnosed after presenting with a sign or symptom of breast cancer, an obvious difference was found regarding the greater percentage of carcinoma in situ and early stage cancer diagnosed in the women from the screening programme. Fig. 3 makes a comparison of both groups by clinical stage at time of diagnosis.
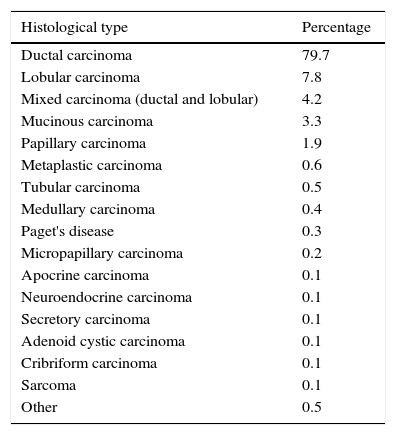
Histopathological characteristics. Of the 4411 cases with a diagnosis of breast cancer and according to the histopathological classification proposed by the WHO, the most common histological type was ductal carcinoma, at 78% of all the cases. Table 1 describes the histopathological types with their respective percentages.
Histopathological types and frequency.
| Histological type | Percentage |
|---|---|
| Ductal carcinoma | 79.7 |
| Lobular carcinoma | 7.8 |
| Mixed carcinoma (ductal and lobular) | 4.2 |
| Mucinous carcinoma | 3.3 |
| Papillary carcinoma | 1.9 |
| Metaplastic carcinoma | 0.6 |
| Tubular carcinoma | 0.5 |
| Medullary carcinoma | 0.4 |
| Paget's disease | 0.3 |
| Micropapillary carcinoma | 0.2 |
| Apocrine carcinoma | 0.1 |
| Neuroendocrine carcinoma | 0.1 |
| Secretory carcinoma | 0.1 |
| Adenoid cystic carcinoma | 0.1 |
| Cribriform carcinoma | 0.1 |
| Sarcoma | 0.1 |
| Other | 0.5 |
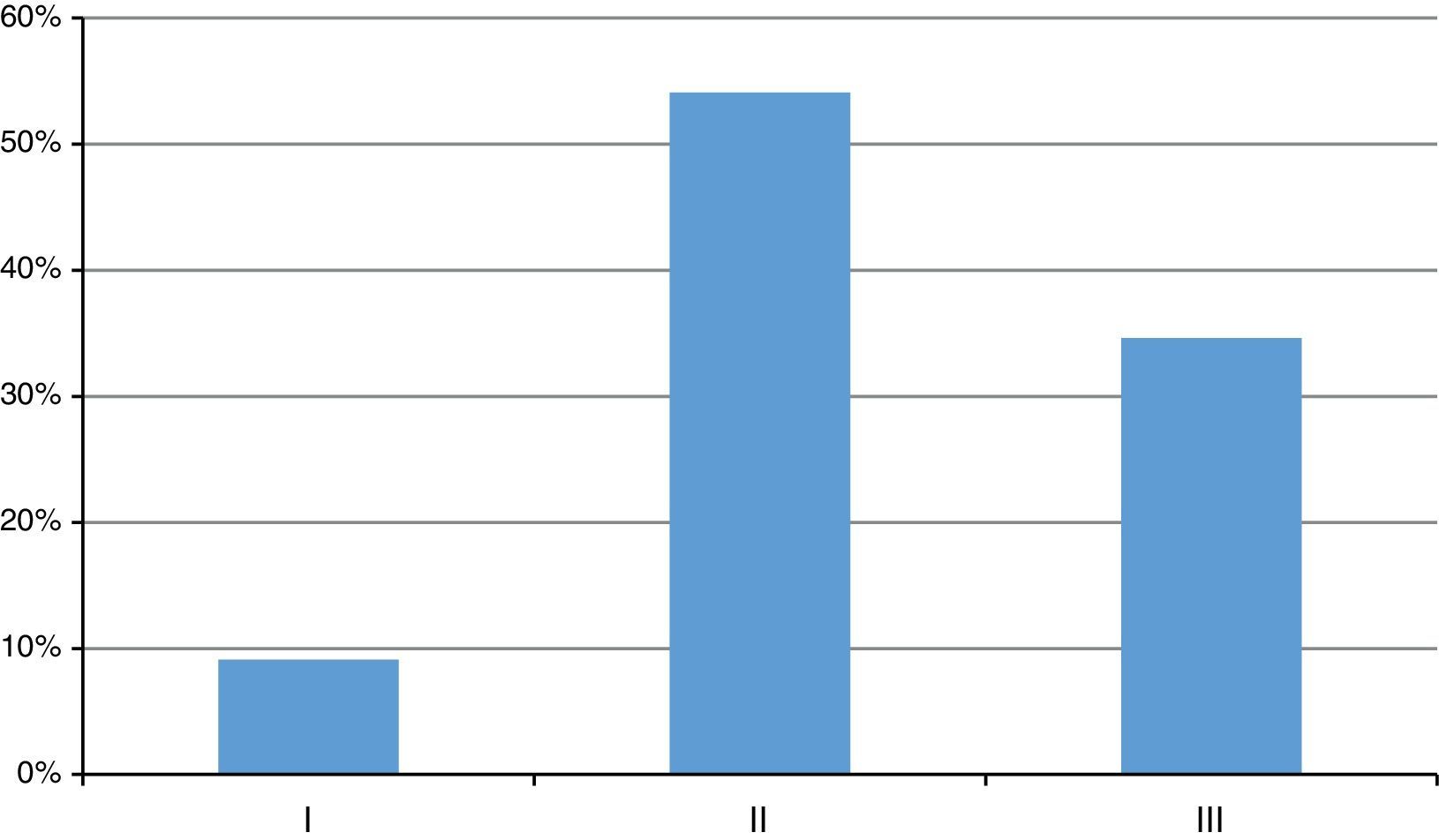
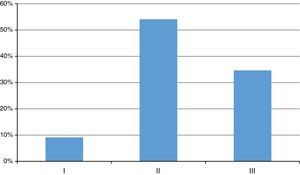
With regard to histological grade, of the total amount of invasive ductal carcinomas, 9.1% were well differentiated or grade I tumours, 54.1% moderately differentiated or grade II and 34.6% poorly differentiated or grade III (Fig. 4).
In the series of cases of invasive carcinoma that we show here, 41.2% presented lymphovascular invasion of the tumour and 58% did not.
Immunohistochemistry. Information on hormone receptors, Her2 over-expression and molecular phenotypes was calculated with 3738 cases, since the complete information was not available for some patients who had been diagnosed in our institution but had received treatment elsewhere.
Oestrogen receptors (OR). Of the population studied in this paper, 74.3% of the patients presented some OR expression, and the division below was made to determine the intensity of expression:
Expression from 1% to 10% OR in tumour cells: 6.83%.
Expression from 11% to 50% OR in tumour cells: 16.41%.
Expression from +50% OR in tumour cells: 76.74%.
Progesterone receptors (PR). In this series there was PR expression in 64.1% patients, and the division below was made to determine the intensity of this expression according to the St Gallen consensus for the early management of breast cancer7:
Expression from 1 to 19%: 25.27%.
Expression ≥20%: 74.72%.
Her 2-neu. In this study, Her 2-neu over-expression was found in 19.6% of our patients; most were diagnosed by immunohistochemical techniques, however, 6.4% reported as doubtful and required confirmation by in situ hybridisation (FISH or CISH).
Ki67. Based on the recommendation by the St Gallen consensus, 14% was confirmed as the cut-off value for qualifying a Ki67 as elevated.7 In our population with breast cancer:
43.6% presented a Ki67 ≤14%.
56.3% presented a Ki67 ≥15%.
Biological subtypes. With the information from the immunohistochemical panel result of 3738 patients, the phenotyping of the different subtypes was:
Luminal: 65.73%.
Luminal Her2 positive: 10.91%.
Pure Her2 positive: 8.72%.
Triple negative: 14.63%.
This study is a descriptive analysis of the clinical pathological characteristics of breast cancer in a population of more than 4000 cases in Mexico diagnosed in an institution that attends patients from Mexico City, Estado de México, Puebla, Hidalgo, Veracruz, Chiapas and Guerrero, in which it is clearly feasible to appreciate similarities and differences in relation to aspects described in previous publications. One of the most relevant features of our population, already published by Rodríguez-Cuevas et al., is the age of presentation at the time of the breast cancer diagnosis; in their study they report a mean age of 51 years and a higher incidence in the 40 to 49 year age group. In our study the average age was 53 years and again the 41 to 50 age group was most affected (30% of the total cases), while in other countries the average age of presentation is reported as 63 years.4
The mammography breast cancer screening programme is still being developed in our country and the entire target population has not been included. Villaseñor-Navarro reported a 7.2% coverage of the target population for screening mammography, 11.2% coverage for 2009, from Health Department figures for 2006, and an increase of 21.6% was estimated for 2012. However, this programme only included women over the age of 50 and the Mexican Official Standard for breast cancer was amended in 2012 to include women aged over 40 with “risk factors”.8 We have an “opportunistic” screening programme in our institution which is governed under the recommendations of the Breast Health Global Initiative.9 Using this programme, carried out on an individual basis and in conjunction with different public health institutions (INMujeres DF, Secretaría de Salud), it was possible to diagnose 867 patients (19.7% of the population of this study) and on comparing the clinical stages with those of the women who were diagnosed after the onset of a sign or symptom of breast cancer, we observed a considerable difference, identifying more cases of carcinoma in situ and in the initial clinical stages (Fig. 4) thus enabling better prognosis in terms of disease-free time and overall survival, and greater probability of receiving breast-conserving surgery.
There is very significant variation worldwide in the stages of breast cancer at time of diagnosis. The early stages predominate in industrialised countries that have public awareness-raising programmes, mammogram screening for the entire target population and high economic resources for the integral care of positive cases. In Mexico, most women who are diagnosed with breast cancer are in the advanced stages. This is due to the lack of education and awareness-raising of the disease, and the lack of access to healthcare institutions for care.10 Mohar et al. previously reported an estimated 80% of cases in locally advanced or metastatic stages at time of diagnosis in Mexico.11 In our series, the locally advanced and metastatic stages at time of diagnosis were in 52.9% of the patients, and this lower figure could equally be associated with our institution's screening programme. In a Mexican population, Flores-Luna et al. reported 67.5% locally advanced and metastatic stages at time of diagnosis and survival at 5 years was 73.6% for early stages compared to 44.2% at advanced stages, confirming the favourable impact on survival of prompt detection.12
The histological grade is one of the most important prognostic factors to determine biological behaviour and is a useful tool for establishing the need for adjuvant treatments.13,14 The Scarff-Bloom-Richardson scale as amended by Elston and Ellis,15,16 also known as the Nottingham scale, is used in the pathology department at the IEM-FUCAM. This is one of the most widely used scales and essentially takes 3 parameters into account for grading: tubule formation, nuclear grade and mitotic rate. In this study, more than 90% of the patients had grades II and III. According to information from the National Cancer Institute of the United States, through their Surveillance, Epidemiology, and End Results (SEER) database, which included more than 70,000 patients, it has been demonstrated that patients with grade III tumours were at more than double the risk of dying from the disease than those with grade I tumours.13
The histological subtypes coincide with those reported in other series in which infiltrating ductal carcinoma with no specific pattern constitutes the majority of cases. Data from the National Cancer Institute of the United States indicates that of 135,157 cases, infiltrating ductal carcinoma comprises 76%, lobular carcinoma 8%, mixed carcinoma (ductal/lobular) 7%, mucinous carcinoma 2.4%, tubular carcinoma 1.5%, medullary carcinoma 1.2%, papillary carcinoma 1% and other histologies total 5% of cases, and these are very similar results to those of our study. Some histological types of breast cancer are associated with a particularly favourable clinical outcome. The histological variety is a prognostic factor to be considered as well when deciding breast cancer management. Tumours of special types that have been shown to have an excellent prognosis include tubular carcinoma, cribriform carcinoma, mucinous carcinoma, adenoid cystic carcinoma, tubulolobular carcinoma and papillary carcinoma; in these, the use of systemic chemotherapy management is limited to higher stages of the disease.17,18
Lymphovascular invasion is also a biological factor which, together with the histological grade, is closely related to the aggressivity of the tumour, and is principally linked to the decision for adjuvant treatment (chemotherapy or radiotherapy) post-mastectomy.19 A meta-analysis published by San-Di et al. demonstrated a clear association of the presence of lymphovascular invasion as an adverse factor intimately related to tumour size, lymph node involvement and tumour grade.20 In a series of more than 2000 patients, García-Fernández et al. reported in the multivariate analysis that lymphovascular invasion was a prognostic factor majorly associated with breast cancer mortality.21
Phenotyping of breast cancer has very relevant prognostic impact and plays a crucial role in therapeutic decision-making. From the studies by Perou et al. various breast cancer “subtypes” have been established, determined by the variation in gene expression, thus enabling at least 4 biological subtypes to be identified which, with the current available data, we can “substitute” genetic information for the histopathological study results of the tumours and determine 4 biological markers using immunohistochemistry techniques; these are OR, PR, Her 2/neu proto-oncogene and cell proliferation index Ki67.22
OR belong to a nuclear hormone receptor family and act as transcription factors when they bond to their respective ligands. OR expression is a determinant of response to endocrine treatment, the greater the expression the better the response to this management. Gene amplification or Her 2/neu proto-oncogene over-expression is a prognostic marker of a poor outcome in the absence of targeted treatment, manifested by an increased rate of metastasis, shorter time to relapse and poorer overall survival. However, complete disease response rates of up to 51% of patients that over express Her2/neu and receive targeted therapy in combination with chemotherapy have been demonstrated recently, which offers this group of patients a good prognosis.23 Ki67 is a specific monoclonal antibody against a nuclear antigen that expresses in the cells under proliferation. Elevated Ki67 is an independent adverse prognostic factor in breast cancer.
Luminal phenotypes express a percentage of OR or PR through immunohistochemical determination; the Her-2 pure phenotype does not express either OR or PR, but does have Her-2 neu over-expression, the triple negative phenotype corresponds to tumours that express neither hormone receptors nor Her 2-neu.7
In relation to the biological subtypes, similar results have been reported to those of this study. In a study of more than 60,000 patients, Parise et al., reported an 80% incidence of the luminal subtype, 23% of patients over-expressed Her-2 (of whom 67% also had hormone receptor expression) and 13% corresponded to triple negative.24
Overall survival tends to be more favourable in patients that have hormone receptor expression, followed by those with Her-2 overexpression (who receive specific anti-her 2 treatment), while those with triple negative tumours have the poorest prognosis.25,26
ConclusionsThis study provides relevant information with regard to the clinical and pathological characteristics of breast cancer in a group of Mexican women. It demonstrates again that the age of presentation is younger than that of the developed countries, and the clinical stages at the time of diagnosis are higher than in other countries with screening programmes. Furthermore, on comparing other factors, principally histopathological and immunochemical factors, with those reported in other series, we can appreciate very similar results.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Maffuz-Aziz A, Labastida-Almendaro S, Espejo-Fonseca A, Rodriguez-Cuevas S. Características clinicopatológicas del cáncer de mama en una población de mujeres en México. Cir Cir. 2017;85:201–207.