The use of enteral formulas with immunonutrients in patients with gastrointestinal malignancies susceptible to surgery can reduce postoperative morbidity, at the expense of reduced infectious complications, with the consequent reduction in hospital stay and health care costs.
Material and methodsProspective randomised study. 84 patients operated on a scheduled basis for resectable colorectal cancer were recruited. In the group YES IN Impact © Oral was administered for 8 days (3 sachets a day), compared with the NOT IN group who did not receive it.
Results40.5% (17) patients without immunonutrition suffered infectious complications vs 33.3% (14) of YES IN. In patients with rectal cancer NOT IN, 50% (8) suffered minor infectious complications (p=0.028). In each group (YES IN, NOT IN, colon and rectal cancer) when infectious complications were observed, the variables total hospital stay and costs doubled, with significant differences. These variables showed higher values in the group NOT IN compared with those who received immunonutrition, although these differences were not statistically significant.
ConclusionsNOT IN patients suffered infectious complications more frequently than YES IN, with significant results in the subgroup of patients with rectal cancer. The total hospital stay and costs were slightly higher in the group not supplemented, doubling in each category significantly (YES IN, NOT IN, colon and rectal cancer), when infectious complications were observed.
La utilización de fórmulas enterales con inmunonutrientes en pacientes con neoplasias gastrointestinales susceptibles de cirugía puede atenuar la morbilidad postoperatoria, a expensas de la disminución de complicaciones infecciosas, con la consiguiente reducción en la estancia hospitalaria y gastos sanitarios.
Material y métodosEstudio prospectivo y randomizado. Se reclutaron 84 pacientes intervenidos de forma programada por cáncer colorrectal resecable. En el grupo SÍ IN se administró en el preoperatorio Impact© Oral durante 8 días (3 envases al día), con respecto al grupo NO IN que no lo recibió.
ResultadosUn 40.5% (17) de los pacientes no inmunonutridos sufrieron complicaciones infecciosas frente a un 33.3% (14) de los inmunonutridos. En los pacientes con cáncer rectal NO IN, un 50% (8) sufrió complicaciones infecciosas menores (p=0.028). En cada grupo (SÍ IN, NO IN, cáncer de colon y recto) cuando se observaron complicaciones infecciosas, las variables estancia hospitalaria total y gastos se duplicaron, siendo estas diferencias significativas. Estas variables presentaron valores superiores en el grupo no inmunonutrido, con respecto del que recibió inmunonutrición, aunque estas diferencias no alcanzaron la significación estadística.
ConclusionesLos pacientes no inmunonutridos sufrieron complicaciones infecciosas con mayor frecuencia que los inmunonutridos, con resultados significativos en el subgrupo de los pacientes con cáncer rectal. La estancia hospitalaria total y los gastos fueron levemente superiores en el grupo no suplementado, duplicándose en cada categoría de forma significativa (SÍ IN, NO IN, cáncer de colon y recto), cuando se observaron complicaciones infecciosas.
Malnutrition in hospitals and its significant prevalence has been widely reported since the seventies and varies from 19% to 80%, according to the country and type of patients studied.1,2 It is 15–40% in cancer patients at time of diagnosis, and up to 80–90% in cases of advanced disease, depending on the type and spread of the tumours. In patients with colorectal cancer (CRC) the prevalence of malnutrition ranges from 45% to 60%.3,4 Malnourished patients have higher postoperative morbidity and mortality, which involves an increased hospital stay and associated health costs of up to 50%, and poorer perceived quality of life, compared to well-nourished patients.5–7 The perioperative nutritional management of patients undergoing scheduled colorectal surgery has changed in line with scientific evidence, and currently oral supplements with immunonutrients are a therapeutic option.8 These immunonutrients or pharmaco-nutrients (arginine, ω-3 fatty acids, and nucleotides), in addition to regulating the immune response of the host, maintain the functionality of the mucus barrier and help to modulate local or systemic inflammatory reaction, nitrogen balance and protein synthesis.9,10 In financial terms, nutritional supplements with immunonutrients are more costly than a normal diet (€144.4/patient vs €33.4/patient, respectively).11 However, the reduced postoperative complications and hospital stay observed in many meta-analyses show substantial health cost savings, and demonstrate that immunonutrition is more cost effective compared to standard nutrition(€5668/patient vs €7092/patient, respectively).11–14 Therefore, in surgical patients with gastrointestinal cancers, enteral formulas with arginine, ω-3 fatty acids, and ribonucleic acid lower the incidence of infectious complications, shorten hospital stay without affecting mortality, and constitute a cost-effective measure.15–17 On the other hand, these research studies present many limitations in terms of their application in the specific group of CRC patients namely, the methodological quality of the individual research studies, the heterogeneity of the disorder suffered by the patients recruited and their diverse nutritional statuses, the variety of nutritional regimens used and the amounts and time of their administration.18–20 Likewise, there are few studies that focus on CRC patients undergoing elective surgery in whom postoperative infectious complications have been observed after following an “immune diet”, stratified according to tumour location, and that analyse hospital stay and health costs. We consider, for these reasons, that it was necessary to undertake this study.
The main aim of our study was to evaluate the efficacy of perioperative oral supplements with immunonutrients compared to routine presurgical preparation for scheduled colorectal cancer surgery in the general and gastrointestinal surgery department of the General University Hospital of Ciudad Real, in terms of reducing the incidence of postoperative infectious complications, hospital stay and, as a consequence, health costs.
Material and methodsA prospective and randomised study, undertaken in the General University Hospital of Ciudad Real, over a period of 11 months (1 December 2010–31 October 2011), which included 84 patients. The randomisation sequence was established using a table of random numbers. The study was approved by the Clinical Research Ethics Committee of the General University Hospital of Cuidad Real, and complied with the standards of the Declaration of Helsinki.
Inclusion criteriaPatients aged over 18 years diagnosed with CRC, scheduled for CRC surgery with curative intent (including patients with resectable metastatic disease), who underwent a surgical procedure with intestinal resection, and who had signed their informed consent for the surgery, and to be included in the study.
Exclusion criteriaEmergency surgery or pregnancy, preoperative evidence of non-resectable metastatic disease, American Society of Anesthesiologists Grade V, respiratory, heart, liver or renal failure, active preoperative infection, requiring enteral or parenteral nutrition in the immediate preoperative period (15 days).
Variables analysed/protocolThe subjects were randomised into Group A (immunonutrition yes: YES IN) who received preoperative immunonutrition and followed a normal diet and Group B (immunonutrition no: NO IN), who did not receive immunonutrients (routine preoperative management) but did take a normal diet. The YES IN group were given Impact© Oral (Novartis©; Medical Nutrition, Spain) preoperatively, three 237ml bottles per day, over 8 days. Postsurgical infectious complications were recorded and classified as minor (surgical wound infection, phlebitis, bacteraemia, urinary tract infection) and major (anastomotic leak), up to 30 days after discharge from hospital. The results were stratified according to the intestinal segment affected by the cancer (colon and rectum). The overall hospital stay was recorded and the mean costs per patient, which were calculated according to the diagnosis-related group (DRG) to which each patient was assigned by our centre's codification department. Patients suffering any type of complication were assigned to DRG 148: major small and large bowel procedures with complications. The patients with no complications were assigned to DRG 149: major small and large bowel procedures with no complications. For each patient, the cost of the daily hospital stay according to their assigned DRG was multiplied by their total days of hospital stay, adding the cost of the preoperative oral supplements in the group following the “immune diet”.
Statistical analysisThe Student's t-test was used to compare independent means, in the study of a quantitative dependent variable compared to a dichotomous qualitative variable, verifying independence and normality using the Rachas and Kolmogorov–Smirnov tests, respectively. When the qualitative variable had more than two classes, the ANOVA test was used, verifying the necessary assumptions for its use. The χ2 test, with its corresponding continuity correction, was used to compare the categorical variables as long as the validity conditions for this approach were met. Otherwise, Fisher's exact test was used. The statistical analysis was performed using SPSS©, version 17.0. p values of <0.05 were considered statistically significant.
ResultsBaseline characteristicsThe sample of 84 patients were randomised into the group that received preoperative immunonutrition, YES IN (n: 42) and the group that did not, NO IN (n: 42). The mean age was 69.9±11 years with a predominance of males at 69.05% (58). Neither group showed differences in their baseline characteristics, therefore they were comparable in this regard.
ImmunonutritionIn our study the nutritional supplement was Impact® Oral (Novartis©; Medical Nutrition, Spain), irrespective of the nutritional status of the subject. This high-protein supplement with immunonutrients was administered over 8 days in the immediate preoperative period (mean 7.3±0.8 days), following a guideline of 3 bottles (237ml ×3) per day (mean volume ingested 5180.1±618.4ml). Each 237ml bottle contained 341kcal, distributed into 18.1g proteins (4.2g l-arginine), 44.7g carbohydrates, 9.2g fats (ω-3 fatty acids 1.4g), 3.3g fibre, 0.43g nucleotides, vitamins and trace elements.
Baseline nutritional statusAt the first preoperative consultation, the overall prevalence of protein malnutrition (subjects with at least one altered parameter: retinol-binding protein, transferrin, albumin and prealbumin) was observed in 31% (26) in the patients studied, with a non-significant distribution in the groups studied [YES IN: 28.6% (12) and NO IN: 33.3% (14)]. Moreover, caloric malnutrition was 60.7% (51) (subjects with at least one altered parameter: percentage of weight loss, body mass index and total cholesterol). The prevalence in both subgroups was similar and was not significant, at 64.3% (27) in YES IN and 57.1% (24) in NO IN.
Likewise, we used Nutritional Risk Screening (NRS) to determine our patients’ risk of malnutrition at their first consultation. This test enables the patients’ nutritional status to be evaluated according to weight loss, reduced intake, body mass index and severity of disease. It classifies patients according to their nutritional risk with a total score: if the score is ¿3 it is considered that the patient is not at risk of malnutrition. If the score is ≥3 it is considered that the patient is at risk of malnutrition. In our analysis, 64.3% (27) of the patients taking immunonutrition (YES IN) and 64.3% (27) of those in the NO IN group presented a risk of malnutrition at their first consultation.
Another method of nutritional screening used was the nutritional risk index, which combines biochemical (albuminaemia) and anthropometric parameters (current weight, usual weight), considering a patient with ≤100 to be at nutritional risk. In our study, the percentages obtained of overall malnutrition risk in YES IN and NO IN were similar, at 16.6% (7) and 19% (8), respectively. These nutritional risk indices showed no statistically significant differences in either subgroup.
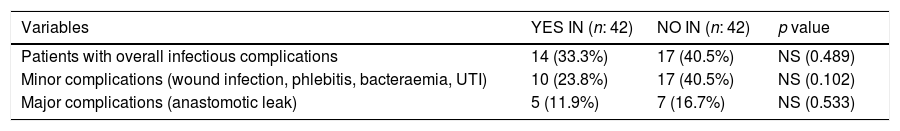
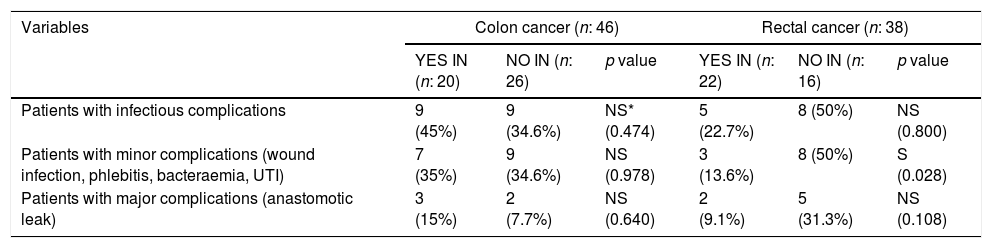
Infectious complicationsOverall, the postoperative infectious complications were most frequent in the NO IN group compared to the group receiving immunonutrition, although with no statistically significant results (Table 1). In the patients operated for rectal cancer, minor infectious complications (wound infection, phlebitis, bacteraemia and urinary tract infection) were more common in NO IN than in YES IN. These differences were statistically significant (p=0.028) (Table 2).
Overall infectious complications.
| Variables | YES IN (n: 42) | NO IN (n: 42) | p value |
|---|---|---|---|
| Patients with overall infectious complications | 14 (33.3%) | 17 (40.5%) | NS (0.489) |
| Minor complications (wound infection, phlebitis, bacteraemia, UTI) | 10 (23.8%) | 17 (40.5%) | NS (0.102) |
| Major complications (anastomotic leak) | 5 (11.9%) | 7 (16.7%) | NS (0.533) |
UTI: urinary tract infection; NO IN: patients not receiving preoperative immunonutrition; NS: not significant; YES IN: patients receiving preoperative immunonutrition.
infectious complications according to the colorectal segment affected.
| Variables | Colon cancer (n: 46) | Rectal cancer (n: 38) | ||||
|---|---|---|---|---|---|---|
| YES IN (n: 20) | NO IN (n: 26) | p value | YES IN (n: 22) | NO IN (n: 16) | p value | |
| Patients with infectious complications | 9 (45%) | 9 (34.6%) | NS* (0.474) | 5 (22.7%) | 8 (50%) | NS (0.800) |
| Patients with minor complications (wound infection, phlebitis, bacteraemia, UTI) | 7 (35%) | 9 (34.6%) | NS (0.978) | 3 (13.6%) | 8 (50%) | S (0.028) |
| Patients with major complications (anastomotic leak) | 3 (15%) | 2 (7.7%) | NS (0.640) | 2 (9.1%) | 5 (31.3%) | NS (0.108) |
UTI: urinary tract infection; NO IN: patients not receiving preoperative immunonutrition; NS: not significant; S: significant; YES IN: patients receiving preoperative immunonutrition.
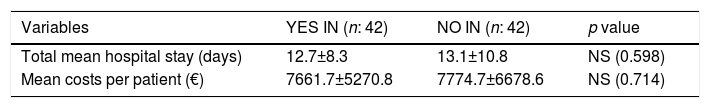
The mean hospital stay was similar in both groups (YES IN and NO IN), and these finding s were not statistically significant. The mean overall costs per patient were slightly higher in the NO IN group compared to YES IN, at €7774.7 and €7661.7, respectively. These differences were not statistically significant (Table 3). The overall costs were obtained from adding the costs of DRG 148 and 149 in each subgroup, so that they were €321,791.9 in NO IN and €326,536.9 in YES IN.
Hospital stay and overall health costs.
| Variables | YES IN (n: 42) | NO IN (n: 42) | p value |
|---|---|---|---|
| Total mean hospital stay (days) | 12.7±8.3 | 13.1±10.8 | NS (0.598) |
| Mean costs per patient (€) | 7661.7±5270.8 | 7774.7±6678.6 | NS (0.714) |
NO IN: patients not receiving preoperative immunonutrition; NS: not significant; YES IN: patients receiving preoperative immunonutrition.
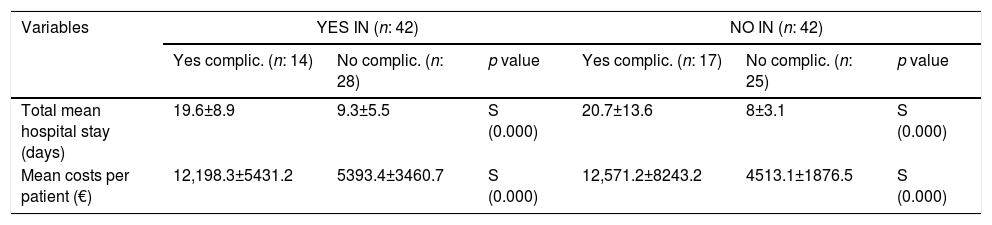
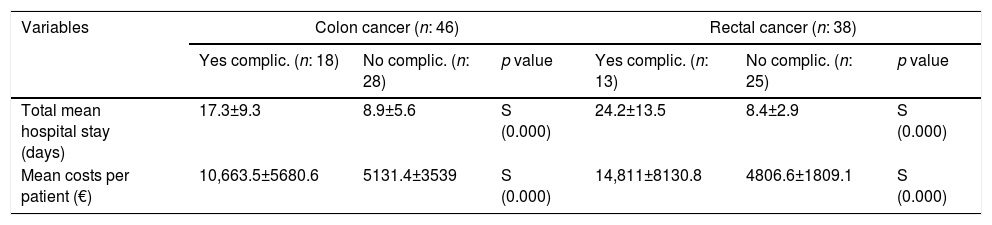
The total hospital stay and associated costs doubled in the group with infectious complications compared to those who had none, both in YES IN and in NO IN (Table 4), and also when they were stratified according to the location of the cancer (colon and rectal cancer) (Table 5). The results were statistically significant (p<0.001). The total hospital stay and costs associated with infectious complications were higher in the group that did not receive immunonutrition and in the patients who had rectal cancer, although these differences were not statistically significant.
Hospital stay and mean costs according to infectious complications.
| Variables | YES IN (n: 42) | NO IN (n: 42) | ||||
|---|---|---|---|---|---|---|
| Yes complic. (n: 14) | No complic. (n: 28) | p value | Yes complic. (n: 17) | No complic. (n: 25) | p value | |
| Total mean hospital stay (days) | 19.6±8.9 | 9.3±5.5 | S (0.000) | 20.7±13.6 | 8±3.1 | S (0.000) |
| Mean costs per patient (€) | 12,198.3±5431.2 | 5393.4±3460.7 | S (0.000) | 12,571.2±8243.2 | 4513.1±1876.5 | S (0.000) |
NO IN: patients not receiving preoperative immunonutrition; S: significant; YES IN: patients receiving preoperative immunonutrition.
Hospital stay and costs according to the colorectal segment affected depending on the presence of infectious complications.
| Variables | Colon cancer (n: 46) | Rectal cancer (n: 38) | ||||
|---|---|---|---|---|---|---|
| Yes complic. (n: 18) | No complic. (n: 28) | p value | Yes complic. (n: 13) | No complic. (n: 25) | p value | |
| Total mean hospital stay (days) | 17.3±9.3 | 8.9±5.6 | S (0.000) | 24.2±13.5 | 8.4±2.9 | S (0.000) |
| Mean costs per patient (€) | 10,663.5±5680.6 | 5131.4±3539 | S (0.000) | 14,811±8130.8 | 4806.6±1809.1 | S (0.000) |
S: significant.
Effectiveness in our study was defined as the percentage of patients who had no infectious complications. This was 66.7% (28) in YES IN and 59.5% (25) in NO IN. These results were not statistically significant.
DiscussionThere are many studies in the literature where a significant reduction has been achieved in postoperative complications in patients operated for gastrointestinal cancer who have received immunonutrition, either preoperatively or perioperatively, compared to those who have not received it. The greatest reduction occurs in the group with infectious complications, especially wound infection, intra-abdominal abscesses and pneumonia. This fact has been confirmed in many randomised studies,16,21–28 and in the current meta-analyses of Zhang,29 Marimuthu19 (both from 2012) and Osland in 2014,20 where a statistically significant reduction in non-infectious complications was observed between the groups receiving immunonutrients and the controls. Our results correlate with these findings, since the infectious complications were more frequent in the group that did not follow an “immune diet” compared to the group that did, although these results were not statistically significant, except in the subgroup of patients with rectal cancer who did not receive immunonutrition and suffered more minor infectious complications, which was significant (p=0.028).
There are a great many meta-analyses in the literature that have observed a reduction in the hospital stay of patients operated for gastrointestinal cancers who have received immunonutrition.18,25,30–36 Cerantola et al.18 and Waitzberg et al.35 analysed the differences between the mean stays of patients receiving immunonutrition and those who did not and found a mean difference of 2.12 and 2.18 days, respectively, with regard to reduced hospital stay, in favour of the patients who followed an immune diet. Our analysis showed mean hospital stays in both YES IN and NO IN, generally lower than the means stays of the abovementioned meta-analyses. This might be because, unlike our study which only included patients with CRC, these meta-analyses studied patients with different digestive tract cancers, whose stays tend to be longer (especially patients with oesophago-gastric and pancreatic cancers).
The financial analysis that details the cost to society of a disease is described in the literature by means of tangible (direct and indirect) and intangible (psychological) cost concepts. Direct costs are the resources used for prevention, treatment, etc., such as hospitalisation costs, outpatient consultations, home care, artificial nutrition and other therapies, which are easy to record and are covered in most studies. Indirect costs are resources that are lost due to inability to work and are relevant in diseases that affect people early and before retirement age. These costs include those of productivity due to temporary absence from work, permanent disability and death before the age of 65. There are practically no nutritional studies that include these costs due to the difficulty of assigning monetary values to these parameters. The intangible or psychological costs tend to be underestimated because it is difficult to assign costs to factors such as pain or lifestyle changes that affect quality of life. The study by Mauskopf et al.37 on patients undergoing elective gastrointestinal surgery due to cancer who were given preoperative immunonutrition used the results of the study by Waitzberg et al.37 and the Healthcare Cost and Utilization Project's 2008 Nationwide Inpatient Sample38,39 to calculate costs in relation to hospital stay and complications. Overall, the mean hospital stay of patients with complications was almost 2.5 times that of those who had none (18.4 vs 7.4 days), and the costs of the total hospital stay ($53,361 vs $20,406). In the specific group of patients with CRC who developed infectious complications, the results were similar. The hospital stay and the costs of the total hospital stay was (16.5 vs 7.1 days) and ($46,320 vs $18,690) in the group with complications and in the group without complications, respectively. The study by Braga et al.11 on 305 patients with gastrointestinal cancer, where one group received preoperative immunonutrition compared to the control group which did not, analysed the costs associated with complications and hospital stay. Overall, the mean costs of the patients who received immunonutrition and the control group who developed complications were more than double (€8793 and €10,494) the costs of those who did not (€3581 and €3622), due to an increased hospital stay and greater consumption of resources. These results were statistically significant (p<0.05). The mean costs of the group who received immunonutrition and suffered infectious complications were €3891, compared to the €5518 of the control group. These results were statistically significant (p<0.001). In our analysis, as in the abovementioned studies, we refer to the direct costs and observed that the hospital stay of the patients with complications was longer, and therefore the costs increased. To be specific, in the group that did not receive immunonutrition, the total hospital stay and costs for those who developed infectious complications were similar to those of the group who received supplements, and no significant differences were observed. The costs we refer to in our study, compared to the literature, were higher in the patients who developed infectious complications, but we must bear in mind that we based our calculation on an assigned DRG which is not specific to CRC and that our health system is different to that of these studies (United States and Italy), therefore they are less comparable in this regard. However, both our analysis and the aforementioned studies only partially estimate the costs, because neither the indirect costs nor the intangible costs were calculated.
Our study's effectiveness was 66.7% (28) in YES IN and 59.5% (25) in NO IN. These results were not statistically significant. This parameter shows the probable capacity of preoperative immunonutrition in patients with colon and rectal cancers to prevent the onset of infectious complications. In the studies by Gianotti et al.12 and Braga et al.,11 the effectiveness in the group that received immunonutrition was 83.3% and 62.8% respectively, in comparison with the group that did not, which was 68.3 and 50%, respectively. The effectiveness of the latter analysis is closer to the results of our study, although it also included patients with gastro-oesophageal and pancreatic cancers. The cost-effectiveness analysis applied to immunonutrition is a financial assessment technique that seeks to compare the cost and clinical effect of this intervention and its alternative (conventional treatment, i.e., no immunonutrition), to determine which is better from a financial and clinical perspective.40 This is the most used technique in pharmacoeconomics and meets the criteria of the National Institute for Health and Care Excellence41 for a treatment to be recommended. In their cost-effectiveness analysis, Gianotti et al.12 observed a net saving of €2386 per complication-free patient in the immunonutrition group. Similarly, Braga et al.,11 obtained an average cost-effectiveness of €3260 per immunonutrition group patient compared to the control group. Likewise, Mauskopf et al.37 estimated that the savings for patients with CRC receiving immunonutrition in terms of reduced hospital stay and infectious complications were $2800 and $1200, respectively. In their calculation of the costs of preoperative oral supplements, Stratton et al.42 observed a saving due to a reduction in daily hospitalisation costs by £688/patient and by £359/patient due to less prolongation of hospital stay, from reduced complications in patients receiving oral supplements. Along the same lines, Russell et al.43 found a saving of €1000 per patient treated with preoperative oral supplements. Therefore, using preoperative immunonutrition such as oral supplements seems to be cost-effective in these patients, since it reduces hospital stay and infectious complications,20,44,45 and this involves a saving in hospital costs.
We can flag up as a limitation of our study that the hospital stay and costs found between the group that received immunonutrition and the group that did not were similar. They doubled in both cases when there were postoperative complications. These results were obtained according to the costs assigned to certain DRGs. In other words, they constitute approximate data for the patients analysed with CRC, which might be compared with other centres where the DRG had the same significance. However, to obtain better adjusted costs and probably significant results, another option would be to undertake a financial study with a larger sample size, focussing on tangible costs (direct and indirect) in patients with CRC stratified as receiving immunonutrition and as not receiving immunonutrition.
To conclude, given that the patients with rectal cancer who did not receive immunonutrition had a significantly higher percentage of minor infectious complications than those who received preoperative immunonutrition, we can deduce that these are the patients who would benefit most from this nutritional intervention, perhaps because most of them undergo neoadjuvant chemotherapy and radiotherapy, which are additional risk factors for these postoperative infectious complications. It is necessary to increase the sample size to delve deeper into this line of research and pursue this study. This would enable us to better confirm this deduction, among other possible objectives. The reduced postoperative complications, hospital stay and, as a consequence, associated hospital costs, observed in the patients with rectal cancer who received immunonutrition and who did not develop complications is another factor in favour of implementing this intervention for these patients. At present, this measure has a major impact on health management. Therefore more correctly designed cost-effectiveness studies are necessary on immunonutrition in CRC patients that encompass all the costs of the process, both tangible and intangible in our health system.
ConclusionsThe patients who did not receive immunonutrition suffered infectious complications more often than those who did, with significant results in the subgroup of patients with rectal cancer (p=0.028). The total hospital stay and the costs were slightly higher in the group who did not receive supplements, and significantly doubled in each category (YES IN, NO IN, colon and rectal cancer), when infectious complications were observed.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Manzanares Campillo MdC, Martín Fernández J, Amo Salas M, Casanova Rituerto D. Estudio prospectivo y randomizado sobre inmunonutrición oral preoperatoria en pacientes intervenidos por cáncer colorrectal: estancia hospitalaria y costos sanitarios. Cir Cir. 2017;85:393–400.