The hydatid disease, or echinococcosis, is endemic in Mediterranean countries, as well as in Australia, Asia, Africa, South America, and Canada. Among its complications is intraperitoneal rupture, a rare form of presentation, with highly variable symptoms. The treatment of choice is surgery plus adjuvant medical treatment in most patients.
ObjectiveA case is presented of a patient with disseminated peritoneal hydatidosis manifested as intestinal ischaemia.
Clinical caseA 50-year-old male was admitted to the emergency room with a history of chronic abdominal pain that worsened in the last 24h. He showed signs of sepsis in the physical examination and was subjected to surgery, in which intestinal ischaemia was found due to a disseminated peritoneal cystic disease, which had led to mesentery retraction. An intestinal resection with an end-ileostomy was performed. The results of the biopsy of the cystic lesions was disseminated peritoneal echinococcosis. Medical treatment was started with albendazole and praziquantel.
ConclusionThis case shows a rare presentation of disseminated peritoneal hydatidosis, which led to intestinal ischaemia.
La enfermedad hidatídica o equinococosis es una enfermedad endémica en los países del Mediterráneo, Australia, Asia, África, América del Sur y Canadá. Dentro de sus complicaciones, la ruptura intraperitoneal es una presentación rara, con síntomas altamente variables. El tratamiento de elección en la mayoría de los pacientes es la cirugía, agregando tratamiento médico adyuvante.
ObjetivoPresentar el caso de un paciente con hidatidosis peritoneal diseminada manifestada con isquemia intestinal.
Caso clínicoHombre de 50 años de edad que fue ingresado al servicio de Emergencias con historia de dolor abdominal crónico que empeoró en las últimas 24h. En la exploración física mostró signos de sepsis y fue sometido a cirugía, donde se encontró una isquemia intestinal condicionada por una hidatidosis peritoneal diseminada, la cual generó retracción del mesenterio. Se realizó una resección intestinal con una ileostomía terminal. Los resultados de la biopsia de las lesiones quísticas fueron de equinococosis peritoneal diseminada. Se comenzó con tratamiento médico a base de albendazol y praziquantel.
ConclusiónEste caso nos muestra una presentación rara de hidatidosis peritoneal diseminada la cual condicionó una isquemia intestinal.
Hydatid disease, or echinococcosis, is caused by the Echinococcus granulosus parasite and can present anywhere in the human body, but affects the liver most (50–60%), followed by the lungs (30%) and other rare locations.1 It is endemic in areas of the Mediterranean, South Africa, South America and Asia.2
Rupture of a cyst inside the peritoneal cavity is a rare and serious complication, about 2% in the primary form is reported.3 Anaphylaxis or sudden death have been reported.3–5 It can be silent, which is rare, and can be diagnosed years later.6,7
ObjectiveWe report the case of a peritoneal hyatidosis which manifested as intestinal ischaemia.
Clinical caseA 50-year-old male, living in poor, basic urbanisation conditions with pet dogs, presented with a 2-year history of chronic abdominal pain. The patient was admitted to the emergency department with an episode of intense abdominal pain in the right hypochondrium, deterioration in general health and fever.
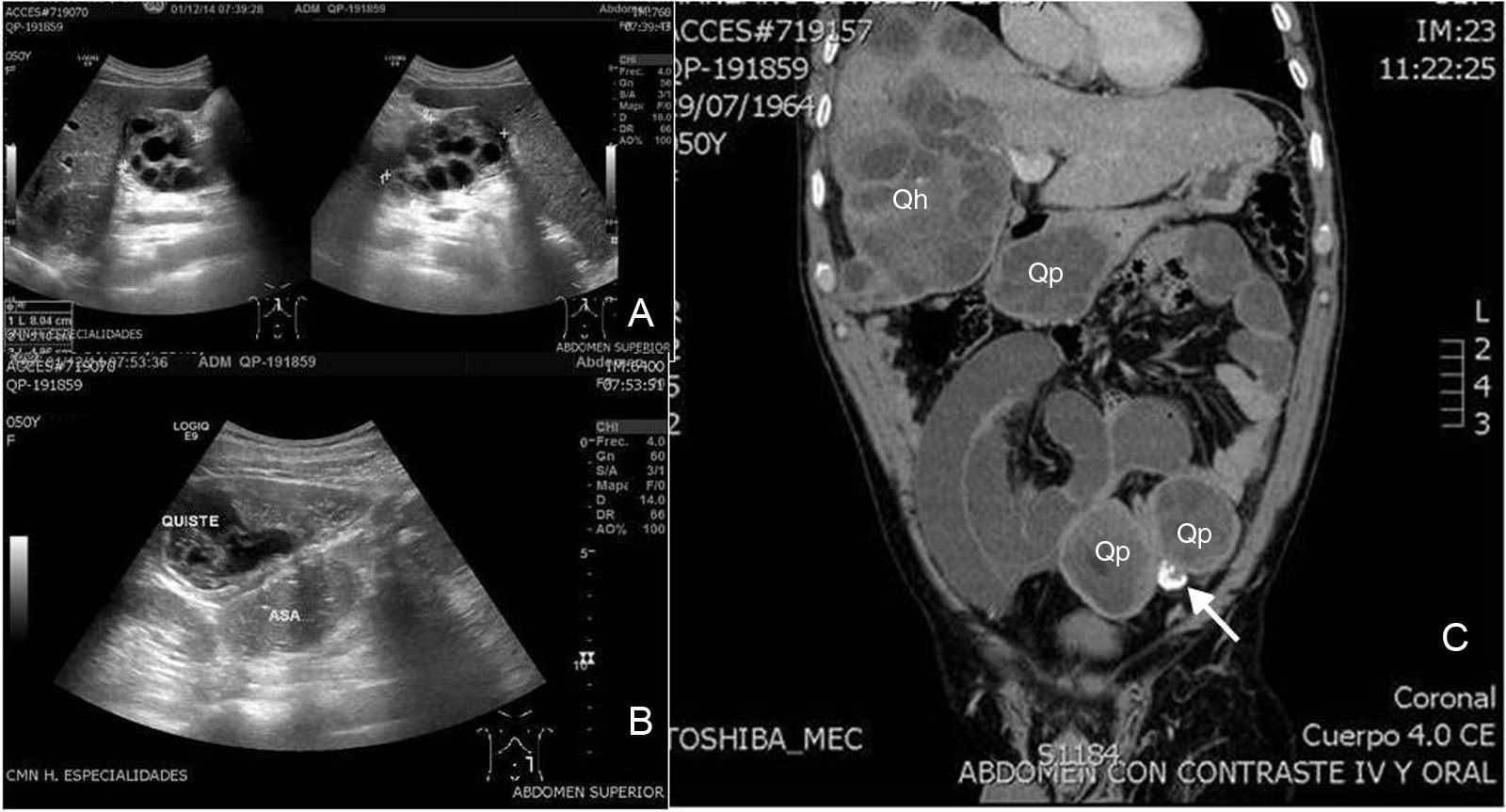
On examination the patient was stable, breathless, dehydrated, swollen, distended abdomen, reduced peristalsis, pain on medium and deep palpation of hypochondrium and right flank, with signs of peritoneal irritation, the remainder with no apparent changes. All the laboratory tests were normal except leukocytosis, at 12,000, with 85% neutrophilia. Ultrasound of the abdomen and pelvis showed multiple multicystic and cystic images in the abdominal cavity, some with central echogenic areas, and others that were hyperechogenic adhering to small bowel loops (Fig. 1A,B). Contrasted tomography of the abdomen and pelvis revealed multiple multicystic images in the liver, the largest was 10×8×3cm, of rosette appearance, predominating in the right lobe; another heterogeneous image in the pancreas of the same appearance, two heterogeneous images in the pelvic cavity, facing the left side, of 5×4×4cm and 5×4×3cm, with an intermediate calcified image of 2×2×1cm, inducing retraction of the mesentery at the level of the ileum, with ischaemia of the small bowel loops (Fig. 1C).
(A) Abdominal ultrasound showing multicystic heterogeneous images in the liver. (B) Image of cyst adhering to small bowel loop. (C) Coronal slice of abdominal computed tomography showing multiple cystic lesions in the liver (Qh), in the peritoneum (Qp) and a calcified cyst between them (arrow).
An exploratory laparotomy was performed, which corroborated intestinal ischaemia of approximately 2m of small bowel from 1.20m from Treiz ligament to 20cm from the ileocaecal valve and multiple cystic lesions in the liver, the largest 10×8×3cm. In the peritoneal cavity there were 3 cystic lesions in the pelvic cavity, one calcified resulting in retraction of the mesentery.
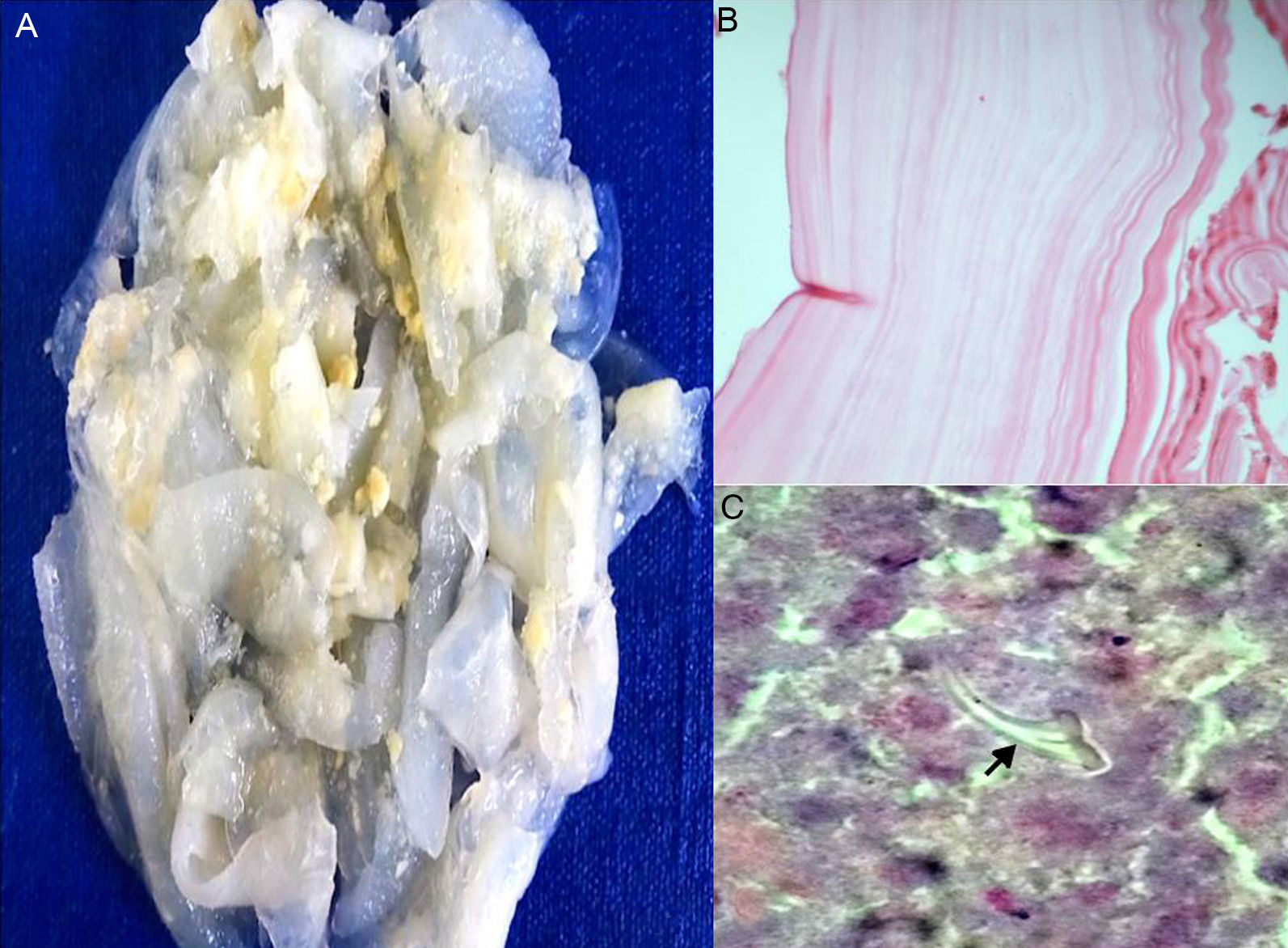
An intestinal resection was performed with terminal jejunostomy and biopsies were taken of the cystic lesions. The histopathological result of the biopsies reported multiple collapsed yellowish-white, translucent and friable vesicles, the cyst wall was greyish in appearance, an acellular laminated membrane together with a germinal membrane and presence of a scolex (Fig. 2A–C), with a final diagnosis of disseminated peritoneal hydatid disease.
The post-operative period was event-free and the patient was discharged 2 weeks after surgery and followed-up as an outpatient, during which time he remained symptom-free. The patient was treated medically with albendazol 400mg twice daily and praziquantel 600mg once a day, for 6 months. His general condition improved and he adapted well to the stoma.
DiscussionIntraperitoneal rupture of a hydatid cyst is a rare clinical presentation, even in endemic regions, with an incidence ranging from 1% to 8%. It usually occurs secondary to liver or splenic cysts that rupture spontaneously or accidentally during surgery.8,9
Although this complication can be completely silent, abdominal pain, nausea, vomiting and urticaria are the most common symptoms. Abdominal signs such as rebound tenderness and pain also usually present.
The release of cystic fluid inside the peritoneal cavity results in the development of multiple disseminated cysts leading to abdominal distension, ascites and bowel obstruction. Diagnosis is confirmed by the presence of hydatid material on histology or cytology testing or scolices in the cyst fluid.
As part of the diagnostic protocol, laboratory tests can show a change in hepatic enzymes such as gamma-glutamyl-transpeptidase, alkaline phosphatase and bilirubins, particularly when there is any degree of cysto-biliary communication. There might be leukocytosis; eosinophilia is found in 25–45% of patients with hydatid cysts in western countries, but it is not specific in endemic areas.10 Serum immunoglobulin levels are elevated in 31% of patients.
Abdominal ultrasound is generally the first radiological investigation undertaken to identify the organ of origin and the characteristics of the cyst. Its sensitivity is approximately 90–95%.11 Abdominal tomography is highly sensitive (95–100%), since it provides a more sensitive characterisation of the lesions.12
According to the WHO Informal Working Group Classification on Echinococcosis that details the most recent standard classification based on ultrasound and tomography, our patient presented multiple types (CL, CE1, CE2, C4 and C5).13
Other studies include immunoelectrophoresis, with a diagnostic accuracy of 91–94% for hydatid cysts of the liver, and of 69–70% for cysts of the lung.
Sensitivity of the ELISA system varies from 64% to 100%, depending on the antigens used.14
Medical management with albendazol/praziquantel, alone or adjuvant to surgery, is used depending on the size, location and dissemination of the cysts.
Surgery remains the treatment of choice, especially for large cysts and in the case of hydatidosis. The type of surgical intervention should be individual to each patient. Complete excision of the cyst that has not disseminated or ruptures is the ideal, but is not always feasible. In such cases, partial excision (if the cyst is close to vital structures) with unroofing and omentoplasty should be performed. The newest methods, such as puncture, aspiration, injection and reaspiration (PAIR) have good success rates.
In this particular case, our patient had intestinal ischaemia, which had to be resolved first in order to then proceed to diagnose the cystic lesions. Presenting as ischaemia as on this occasion is very rare, and has not been documented in the literature. The patient was given adjuvant medical therapy and showed significant improvement at subsequent consultations.
ConclusionsAlthough it is documented in endemic areas, this case report shows how important it is to make this disease known and how it should be considered as part of the general approach for patients with low socioeconomic status or those in close contact with transmitting animals, since our country is susceptible to the disease.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors have no conflict of interest to declare.
Please cite this article as: Rosales-Castañeda E, Estrada-Castellanos A, Goméz-Jiménez LM. Hidatidosis peritoneal diseminada manifestada como isquemia intestinal. Cir Cir. 2017;85:269–272