Meningeal melanomatosis is an extra-axial well-encapsulated malignant tumour with diffuse meningeal growth and dark colouration (due to high melanin contents), while meningeal melanocytoma is the focalised benign variant. Melanocytic lesions may be secondary to melanoma or be histologically benign, however, their diffuse nature makes them impossible to cure.
Melanocytosis is a diffuse tumour that can form solitary extra-axial tumours, which invades the parenchyma and presents signs of malignancy with increased mitosis and Ki67, observed in 1 to 6% of immunopathological exams.
Melanoma of the leptomeninges, presents signs of malignancy with anaplastic cells, which cluster in fascicles of melanin in the cytoplasm, with more than 3 atypical mitoses per field and Ki67 presenting in more than 6% of the immunopathological fields analysed.
Clinical caseWe present the case of a patient with long-term meningeal melanomatosis, with progressive neurologic deficit and characteristic radiologic features, and another case of meningeal melanocytoma.
ConclusionsBenign melanocytic neoplasms of the central nervous system must be treated aggressively in the early phases with strict follow-up to avoid progression to advanced phases that do not respond to any treatment method. Unfortunately, the prognosis for malignant melanocytic lesions is very poor irrespective of the method of treatment given.
La melanomatosis meníngea es un tumor maligno que presenta crecimiento difuso en las meninges, caracterizado por ser una lesión extraaxial, bien encapsulada y de coloración oscura, debido al alto contenido de melanina. Su variante benigna es el melanocitoma meníngeo, sin embargo, esta lesión es focalizada. Las formas difusas de estas lesiones melanocíticas son la melanomatosis y la melanocitosis meníngea.
La melanocitosis es un tumor difuso que puede formar tumores solitarios extraxiales, que invade el parénquima y presenta datos de malignidad, con aumento en las mitosis y en el Ki67, el cual se observa en el 1-6% de los campos inmunopatológicos analizados.
Estas lesiones melanocíticas también pueden ser secundarias a un melanoma, las cuales presentan datos de malignidad con células anaplásicas, que se encuentran agregadas en fascículos de melanina en el citoplasma con más de 3 mitosis atípicas por campo y Ki67, el cual se presenta en más del 6% de los campos inmunopatológicos analizados.
Caso clínicosSe describen 2 casos clínicos: un paciente con melanomatosis meníngea de larga evolución, que presenta la historia natural de la enfermedad y lesiones asociadas, y un segundo caso de melanocitoma meníngeo, en el cual se observó la diferencia entre ambas enfermedades.
ConclusionesLas neoplasias melanocíticas benignas del sistema nervioso central son lesiones que se deben tratar de manera temprana y darles un seguimiento estricto para evitar que evolucionen a fases más avanzadas, cuando no se les pueda otorgar ningún manejo. Las lesiones melanocíticas malignas tienen un pronóstico malo a corto plazo, a pesar del tratamiento que se les pueda ofrecer.
Melanocytic lesions of the nervous system are very similar; however they have different clinical outcomes and different histopathological characteristics, with their either slow or accelerated growth and in their signs of malignancy.1–4 Focalised lesions can include from meningeal melanocytoma to the isolated lesion of a Schwannoma or meningioma.1 Leptomeningeal melanomatosis, melanocytosis or melanoma of the leptomeninges should be taken as differential diagnoses for these diffuse lesions that affect multiple areas of the leptomeninges, which can be differentiated histologically by their number of mitoses per field and their Ki67.5,6
We undertook a review of rare melanocytic lesions that can occur in the central nervous system. These should always be considered when confronting a melanocytic tumour.
Clinical casesClinical case 1A 43-year-old man who had undergone non-specified spinal surgery 12 years earlier, with sequelae of paraplegia. He was admitted to the hospital's neurosurgery department with progressive reduction of strength in his upper extremities, anaesthesia in the 4 extremities and sphincteric incontinence.
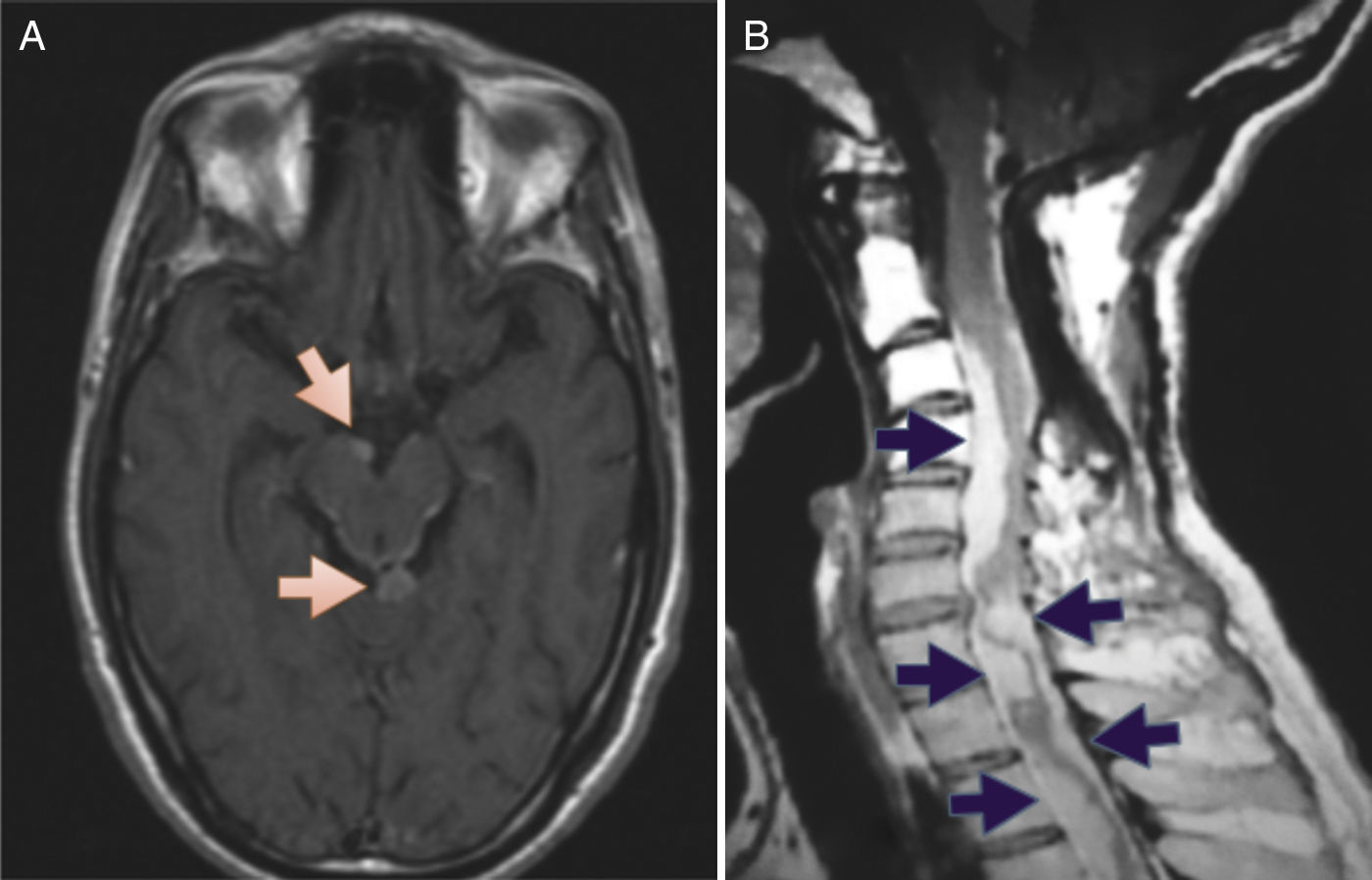
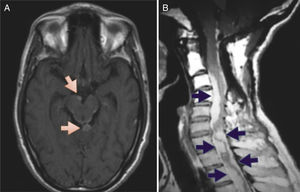
Physical examination revealed intact higher mental functions and cranial nerves, motor system assessment showed hypotrophy of the extremities from the deltoid region (C5, C6), with quadriplegia and upper motor neuron signs: epicritic and protopathic sensitivity below level C7 was absent. Contrast magnetic resonance imaging (MRI) of the skull revealed nodular lesions with calcification at the arachnoid borders (Fig. 1A and B).
(A) Magnetic resonance of the skull, axial slice, T1 sequence with gadolinium, showing a nodular lesion (indicated by arrows) in the interpeduncular cistern and quadrigeminal cistern, with arachnoid enhancement around the midbrain. (B) Magnetic resonance of the cervical spine, sagittal slice, T1 sequence with gadolinium, showing perimedullary lesions (indicated with arrows) that enhance with contrast, irregular and generating compression of the ventral and dorsal face of the cord.
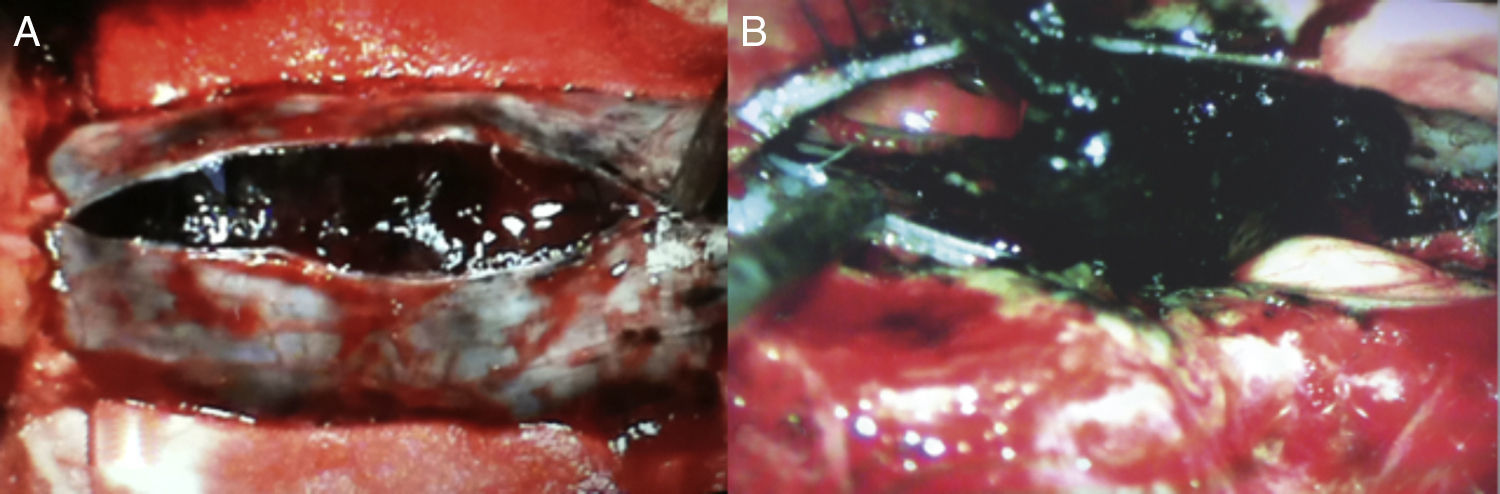
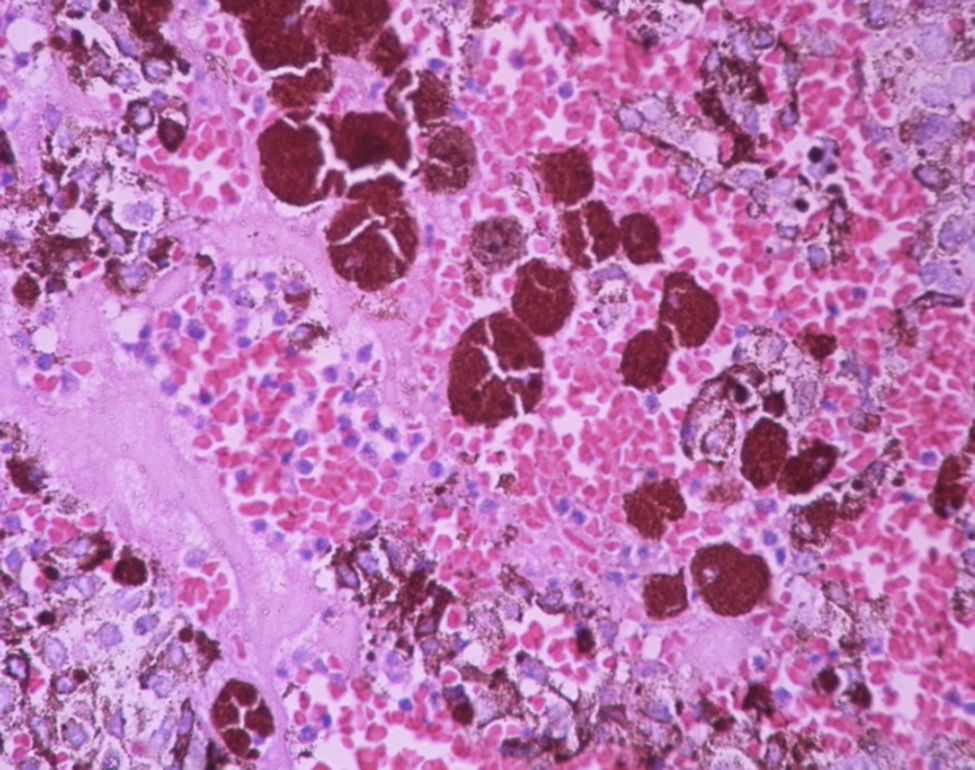
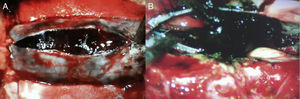
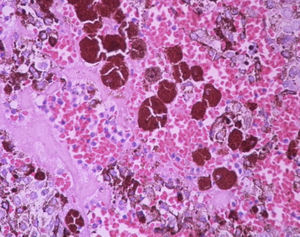
Surgical treatment by laminoplasty of C5 and C7 was performed, and a tense dural sac was observed, with well-delimited arachoid plane, but infiltrated by dark lesion infiltrating the pia mater and the spinal cord and nerve roots (Fig. 2A and B). A sample was taken from these nodular lesions during the operation. The pathology laboratory reported: leptomeningeal melanomatosis with diffuse leptomeningeal dissemination (Fig. 3). Post-operatively the patient continued with his pre-established neurological deficit and there was no clinical improvement.
A 22-year-old female patient, with no relevant history, and whose current disorder had started a year prior to her admission to the hospital's neurosurgical department, with low, non-specific back pain in the morning which had increased in intensity over the subsequent 6 months, radiating to both lower extremities. After 7 months since the lumbar pain had started she presented paraparesis that developed until she was no longer able to walk. Physical examination of the upper extremities found them to be intact with preserved strength; strength in the lower limbs, according to the visual analogue scale was 3/5 in the lower right limb and 4/5 in the left limb, with a lower motor neuron lesion and decreased superficial sensitivity below bilateral L3, with no other neurological disturbance. MRI of the lumbar spine revealed an intradural lesion on L1.
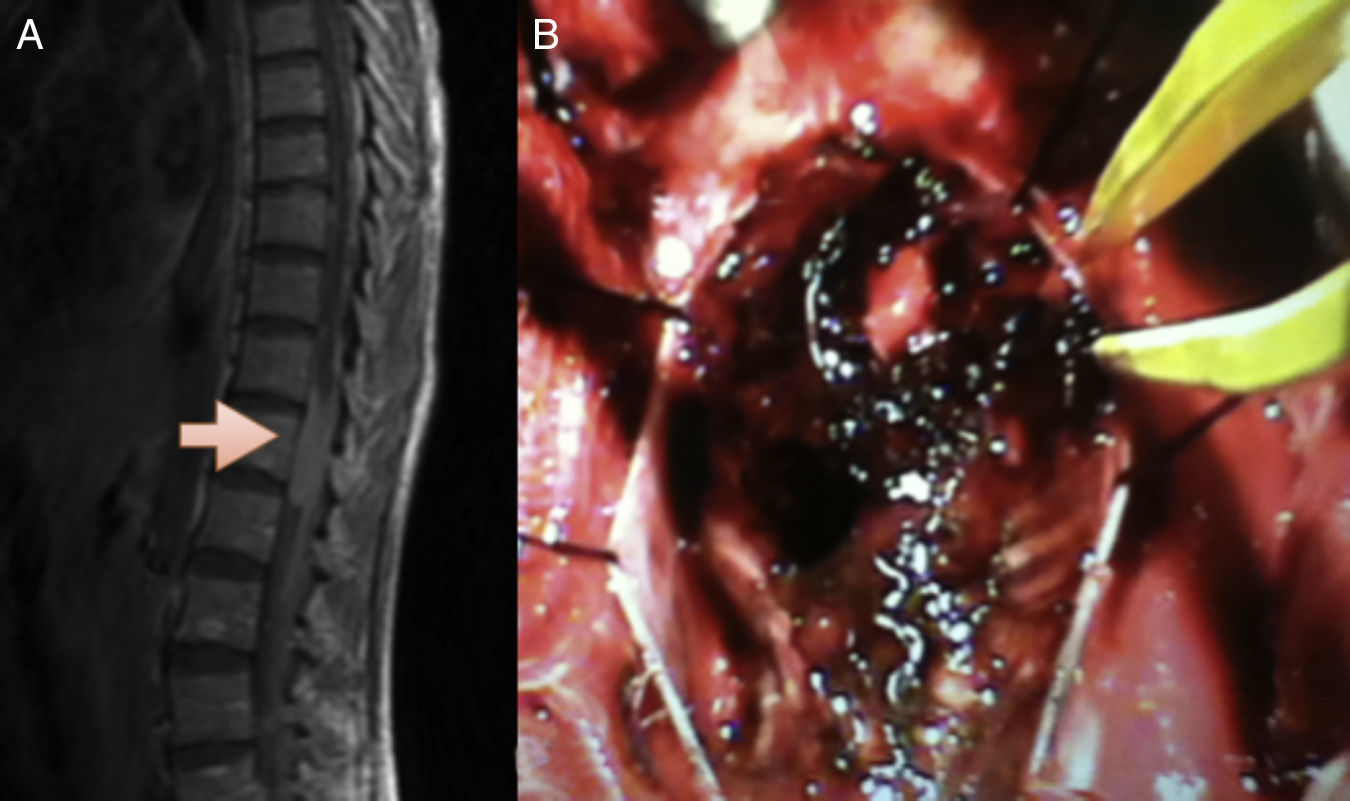
Surgical resection was the treatment established. A dark-coloured lesion was found around the nerve roots, of solid consistency, with delimited arachnoid plane, not infiltrated and bleeding, this was resected and sent to the pathology laboratory, which reported it as a meningeal melanocytoma (Fig. 4A and B). After surgery, the patient made good progress, with improvement in both muscle strength and lower limb sensitivity. At present the patient is neurologically intact, and has recovered muscle strength in the lower extremities, after the appropriate rehabilitation.
(A) Magnetic resonance imaging of the thoracolumbar spine, sagittal slice, T1 sequence, showing an iso-intense, intradural lesion, compressing the spinal canal. (B) Trans-operative image with blackish lesion with no arachnoid infiltration, with nerve routes observed below the arachnoid plane.
Melanocytes originate in the basal layer of the epidermis and the leptomeninges, which share the neural crest as their source.1,7
Primary melanocytic neoplasms are rare lesions that originate from melanocytes. The main areas that are affected by this neoplasm are: the pons, cerebellum, cerebral peduncles, interpeduncular fossa, base of the brain, spinal cord, principally in the cervical region, since these areas are the most abundant in leptomeninges.7–10
According to the World Health Organization (WHO) classification, these central nervous system neoplasms are divided into 3 types: diffuse melanosis, meningeal melanocytoma and malignant melanoma.1,2,10
Meningeal melanocytoma is the benign variety,4,6 described as focalised and very often confused with isolated schwannoma, meningioma, amongst other lesions. Leptomeningeal melanomatosis is the malignant variety, described as diffuse, with at least one mitosis per field with Ki67, which presents in <1% of the fields analysed by the immunopathology department. However, this variety is diffuse and generalised principally in the leptomeninges of the skull base and has a poor prognosis.5,11 Both lesions are extra-axial, with a mean age of 44 years (range 9–75), and the duration of symptoms ranges from 4 weeks to 14 years, according to the literature.2,5
Melanocytosis is a diffuse tumour involving the leptomeninges that can form solitary, extra-axial, tumours, bluish black in colour, that invade the parenchyma and present signs of malignancy with increased mitoses and Ki67. These are present in between 1% and 6% of the fields analysed by the immunopathology department.6
Melanoma of the leptomeninges presents signs of malignancy with aggregates of spindle or anaplastic epithelioid cells in cytoplasmic melanin fascicles, with more than 3 atypical mitoses per field, numerous eosinophilic central nucleoli5,12,13 and Ki67, which presents in >6% of the fields analysed by the immunopathology department.5 Clinically, these are tumours that are well encapsulated, dark in colour (due to the high content of melanin in the tumour)3: the bluish colour of the meninges appears to relate to diffuse melanomatosis0,14 and they have a predilection for the cervical region of the spinal cord.
Most of these tumours have a close relationship with the spinal nerve roots. They adhere and simulate a neurinoma,1,7,15 with a tendency to compress rather than infiltrate. They are slow-growing with progressive root symptoms.8,9
On computed axial tomography they appear as extra axial, well-defined, isodense or slightly hyperdense tumours, with homogeneous contrast uptake, that resemble meningiomas.10,13,16
On T1 MRI they can be iso-intense, although they are generally hyperintense. They are distinguished from mengingiomas that are iso-intense, and schwannoma, which are generally hypointense. On T2 they are hypointense. The behaviour of the tumours on MRI relates to the amount of melanin, and thus, the more abundant the melanin, the shorter the relaxation times on T1 and T2.12,13
Histologically they comprise bundles and nests of spindle or epithelioid cells, with round or oval vesicular nuclei, variable and occasionally prominent nucleoli, with abundant melanin in the cytoplasm and in the melanophages; they have fibrovascular stroma and the cells tend to form whirls. An important characteristic is that they have very low mitotic activity or proliferation rate, and cellular atypias, necrosis, bleeding and invasion of the nerve parenchyma must be absent.2,17
Immunohistochemical analysis is necessary to differentiate meningeal melanocytoma from other similar pigmented lesions.16 Meningeal melanocytoma is characterised by its positive reaction to S-100 protein and vimentin and to antimelanoma antibodies (HMB-45), MITF and Melan-A, and is epithelial membrane antigen negative.16,18
It is even more difficult to differentiate melanocytoma from melanoma, since both test positive for HMB-45, Melan-A, MITF and S-100 protein, and occasionally also express vimentin. The main difference is a lack of signs of histological malignancy such as cellular pleomorphism and nuclear atypia, the presence of abundant mitoses, less than 2% Ki-67, necrosis and bleeding.5,19
Electronic microscopy of the tumour cells demonstrates their melanocytic differentiation with the presence of cytoplasmic dendritic processes and melanosomes in various stages of maturity.5
The malignant transformation of melanocytoma has been demonstrated in local recurrence and leptomeningeal dissemination, in the form of distant metastasis inside the neural axis, which is termed meningeal melanomatosis.11,18 There have even been cases published of metastasis outside the central nervous system.9
Pigmented ependymomas, pigmented schwannomas, neuroectodermic tumours, pigmented paragangliomas and pigmented meningiomas are non-melanocytic pigmented lesions.1
The histopathological features of melanocytomas are Ki67, which presents in <2% of the fields analysed by the immunopathology department, with one mitosis or less per 10 fields and recurrences at 36 months with radiotherapy. Intermediate melanocytic neoplastic lesions present Ki67 that appears in <6% of the fields analysed by the immunopathology department, with mitosis of 1 to 3 per 10 fields and with recurrence after radiotherapy at 17 months. And melanomas present Ki67, which appears in <6% of the fields analysed by the immunopathology department, with mitosis from 2 to 5 per 10 fields and invasion of nervous system tissue and coagulative necrosis.11,20
Rades and Schild15 observed 46 patients over 4 years. They encountered recurrence in 31% of complete excisions and 45% of partial excisions followed by radiotherapy. Seventy-eight percent of their patients underwent complete excision with survival at 5 years of 83% and the remainder (22%) presented a 5 year survival rate of 40% after partial excision.
ConclusionMelanomatosis behaves aberrantly: despite being benign it behaves like a malignant lesion, because of the lesion it generates in the vital structures, principally the brain stem, cranial nerves and spinal cord, which therefore results in major disability.
Effective histopathological testing is essential for these types of lesions, as the principal indicator for this disorder.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that they have followed the protocols of their work center on the publication of patient data.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
Conflict of interestsThe authors have no conflict of interests to declare.
Please cite this article as: Padilla-Vázquez F, Escobar-de la Garma VH, Ayala-Arcipreste A, Mendizábal-Guerra R, Cuesta-Mejía T. Melanocitoma y melanomatosis meníngea, lesiones similares pero diferentes. Cir Cir. 2017;85:273–278.