Spontaneous rupture of a non parasitic hepatic cyst is an extremely rare occurrence. A 50 -year-old male, was admitted with typical clinical manifestations of acute surgical abdomen. At exploratory laparotomy, a giant ruptured non parasitic cyst occupying the entire left liver lobe was found, along with a large amount of free intraperitoneal fluid. The cyst was widely unroofed very close to the liver parenchyma. The patient had an uneventful postoperative course and was discharged six days later. The clinical presentation, diagnostic evaluation and surgical management of this extremely rare clinical entity are discussed, along with a review of the literature. This case, which according to our best knowledge is the fourth reported in the literature, highlights the considerable risk of serious complications associated with the presence of a large symptomatic nonparasitic hepatic cyst. Prophylactic treatment should be considered in all these cases.
Non parasitic hepatic cysts (NPHC) are detected in 4.65% of the population, as a result of the increasing use and refinement of abdominal imaging and ultrasonography.1 They are encountered more often in women by a 4-10:1 ratio, with an age range 50-60 years.2-4 The vast majority are asymptomatic being detected incidentally during abdominal imaging3 and are not associated with hepatic function abnormalities.4 Clinical symptoms occur in about 5% of the patients due to a progressive increase of cyst’s size, or the development of a complication.5 Complications of NPHC are unusual and may include intracystic hemorrhage, torsion, infection, malignant transformation or compression of adjacent structures resulting most commonly in obstructive jaundice.7,8 More rarely, spontaneous rupture,9,10 inferior vena cava thrombosis11 and acute pulmonary embolism,12 have all been reported. We herein describe the case of a spontaneous rupture of a giant non-parasitic hepatic cyst in a 50 year old male, who presented with acute surgical abdomen and was successfully treated with open wide unroofing. To our knowledge, this case appears to be the fourth reported in the literature.
Case presentationA 50-year-old male was admitted with a 4 hour history of a sudden onset of severe abdominal pain, associated with nausea and vomiting. Although the pain was initially epigastric, it progressively became generalized. He also complained of a dull epigastric pain and right upper guardant discomfort, which began to experience two months prior to the current admission. His past medical history included chronic obstructive pulmonary disease, diagnosed two years before.
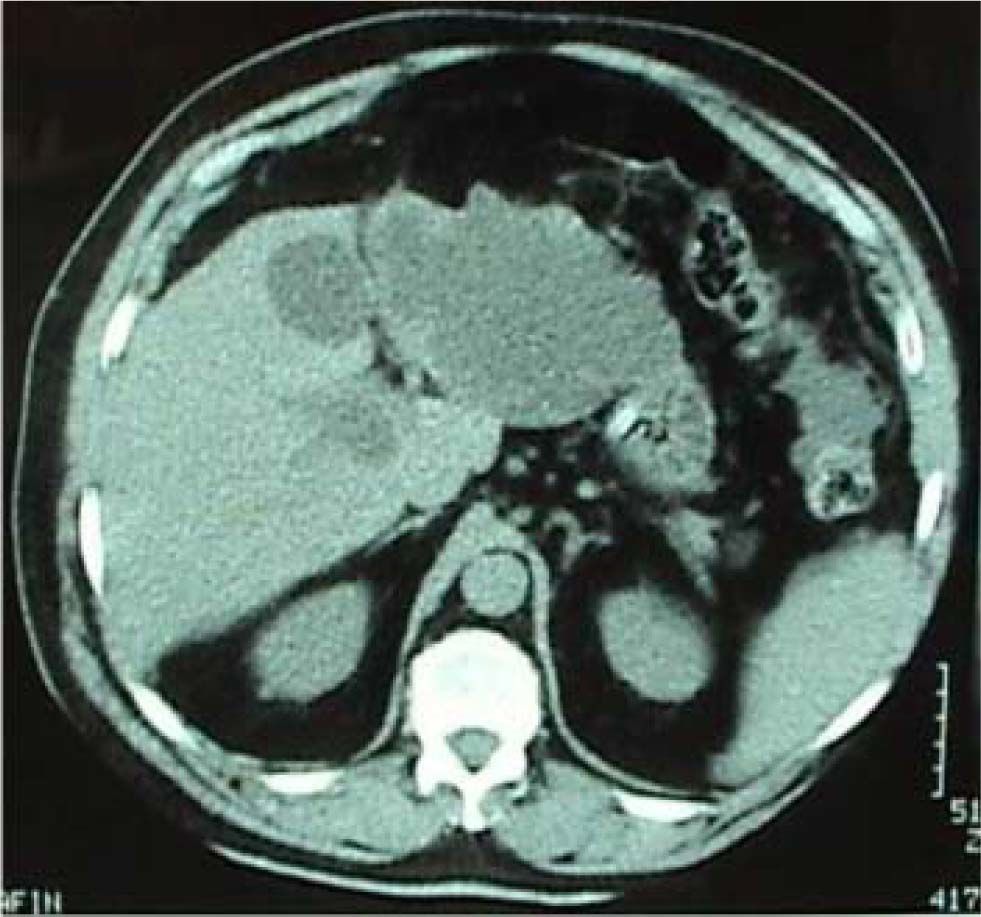
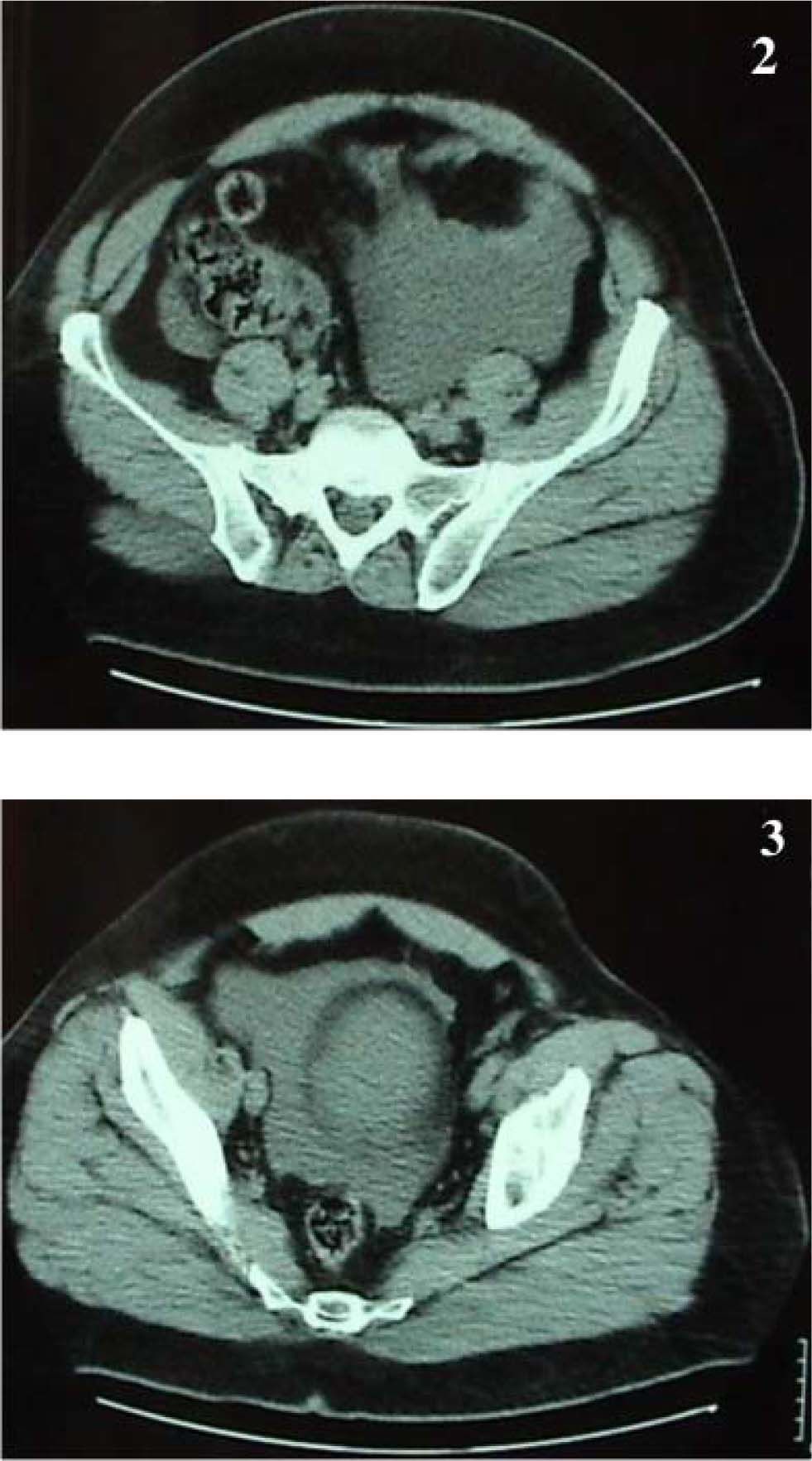
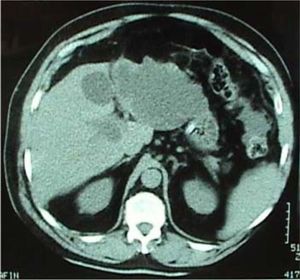
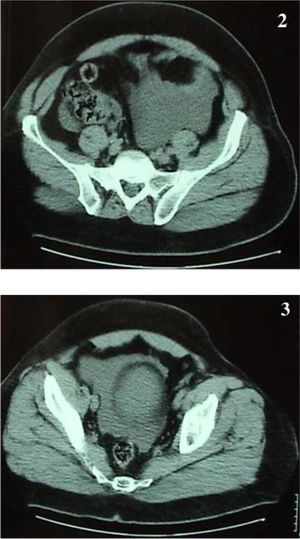
On clinical examination he was distressed, his abdomen was distended with marked diffuse tenderness, guarding and rebound tenderness. Bowel sounds were absent. His blood pressure was 160/100 mmHg, pulse rate 90 beats/minute and body temperature 37.6°C. The haemogram revealed a white cell count of 15,100 ×103/ML with 91.3% neutrophils, a haemoglobin level of 14.2 g/dL and a platelet count of 231 × 103/mL. Liver function tests were normal. Abdominal ultrasonography demonstrated echo patterns consistent with a large cystic lesion occupying almost the entire left liver lobe as well as fluid in the peritoneal cavity. Abdominal computerized tomographic (CT) scans confirmed the presence of a huge homogeneous cyst with irregular borders in the left live lobe measuring 17 × 12 cm (Figure 1) and free intraperitoneal fluid especially in the lower abdomen (Figures 2 and 3).
At emergency exploratory laparotomy, a giant ruptured cyst that occupied the left liver lobe was found and approximately 1,000 mL of intraperitoneal fluid were aspirated. A wide excision of the cyst was undertaken very close to the liver parenchyma. A running locking suture was used along the edge of the resected cyst wall, in order to prevent bleeding and bile leakage. Intraoperative frozen section of multiple specimens from the cystic wall showed no evidence of malignancy, while cytology and cultures of the cystic fluid were negative. Serological tests for echinococcus as well as tumor markers including CEA and CA 19/9 were negative. Histological examination of the entire resected specimen measuring 27 × 12 cm confirmed the diagnosis of a benign non hydatid, non neoplastic simple liver cyst. The patient had an uneventful postoperative course and was discharged six days later. Follow-up examinations performed six and twelve months after surgery showed no findings of recurrence.
DiscussionBenign nonparasitic hepatic cysts are rare congenital lesions that arise from the development of aberrant intrahepatic bile ducts in utero and are lined with cuboidal epithelium.13 They can be classified as congenital or acquired. Congenital cysts can be further divided into solitary benign nonparasitic cysts, polycystic liver disease, or Caroli’s disease. The acquired type includes neoplastic, traumatic and infectious cysts.14 The majority of hepatic cysts remain asymptomatic and managed conservatively,2,15 due to the risk of complications in therapy and the possibility of spontaneous regression.16 The most common presenting features in symptomatic patients are epigastric pain, nausea, vomiting, a feeling of fullness or of early satiety.2,6,17
To our knowledge, only 14 cases of spontaneous rupture of NPHC have been reported in the English literature.9,15 Sudden abdominal pain was the most frequent symptom in 13 cases, while one patient was asymptomatic. We were able to find only three cases of patients who developed acute abdomen following spontaneous rupture of a NPHC.18-20 Our case appears to be the fourth reported.
Several therapeutic approaches have been described for the management of NPHC, including guided aspiration with or without injection of a sclerosant, open unroofing, laparoscopic unroofing, radical excision, cyst enterostomy, hepatic resection and liver transplantation.4,13,21 Prior to any kind of intervention, a thorough diagnostic evaluation is mandatory. Ecchinococcal serology should be obtained in all patients with cystic liver lesions and rare cases of cystic tumors need to be excluded.6,14
Ultrasonography or CT-guided cyst aspiration can be easily performed in cysts larger than 5 cm in diameter,17 but is associated with recurrence in 100% of the cases21-23 and additionally carries a considerable risk of complications. The only indications of the procedure are either patients with high operative risk or the need to perform a cytologic diagnosis.17 Additionally, it is a good therapeutic test to ascertain whether abdominal symptoms are related to the liver cyst14 in order to avoid an unnecessary intervention.3 In order to destroy the secretory epithelial layer of the cyst, aspiration can be combined with the injection of a sclerosing agent such as ethanol, minocycline chloride, or tetracycline chloride. This procedure results to a much lower recurrence rate which may still be as high as 20%13 but should be considered only after a malignant or infectious etiology and a biliary communication have all been ruled out.2,21 However, series of this technique involve small number of patients and insufficient follow-up do not allow adequate evaluation of its efficacy.14
Laparoscopic unroofing has been increasingly used in the management of NPHC. Various studies have shown that it is associated with reduced morbidity, shorter hospital stay and more rapid return to normal activity, when compared with open unroofing.24 Laparoscopic treatment has been also been reported in the emergency setting, with good results.15 The two methods appear to have almost similar recurrence rates.2,4,17,21,22 These findings are however influenced by case selection and should be treated with some caution.2,4 Additionally larger periods of follow-up are also necessary.4 Gigot et al,3 in a series of 26 patients found that laparoscopic fenestration was technically feasible in 94% of the cases. Various factors that may affect recurrence have been identified, including inadequate extent of deroofing, deep cysts and cysts in posteriors segments of the liver, the use of an argon beam coagulator for the remaining cystic wall epithelium, omentoplasty for the residual cavity and previous laparoscopic treatment or open fenestration which has resulted in dense adhesions formation.3 Consequently, adequate patient selection and type of cystic disease are crucial before considering any intervention.3,4
In order to improve the recurrence rate, Emmerman et al6 combined laparoscopic radical deroofing with an omental transposition flap. Omentum placement keeps the cavity open and has the ability to absorb fluid produced by the cystic epithelium. This operative technique was applied in 13 out of 18 patients of the study and resulted in 0% recurrence rate, whereas in the group of patients where no omental flap was used the relative rate was 11%.
In cases where the cystic fluid is bile stained and a communication with the biliary tree is suspected, a cystoenteric anastomosis using a Roux-en-Y jejunal loop is indicated.2,14,17 Intraperitoneal drainage in the above mentioned cases is unadvisable and usually results in the formation of a postoperative biloma.14,21 However the construction of a Roux-en-Y cystoenterostomy carries a considerable risk of infectious complications and additional demanding surgery. Tocchi et al,21 reported that all three patients who underwent a cystojejunostomy, developed relapsing cholangitis requiring repeated antibiotic treatment, while in one patient hepatic resection due to septic complications was performed one year later. More radical procedures like hepatic resection and cystectomy have also been advocated in the management of NPHC. Although these procedures obtain the best results in terms of recurrence rate,4,17,21 they are however associated with increased morbidity, which may not be acceptable for a benign disease. Martin et al,4 reported a morbidity rate of 50% among 16 patients who underwent hepatic resection for NPHC. Hepatic resections may be better reserved for patients with multiple recurrences or when a possibility of a cystic tumor can not be ruled out.2,25 Radical cystectomy is indicated in symptomatic cysts that can not be adequately unroofed due to a small superficial component,14 while liver transplantation may be indicated in polycystic liver patients with symptoms refractory to other therapeutic approaches or with combined renal failure.2
In conclusion, we describe an extremely rare case of a spontaneous rupture of a huge nonparasitic hepatic cyst in a male patient who presented with clinical manifestations of acute surgical abdomen. Prophylactic treatment should be considered in symptomatic large non parasitic hepatic, cysts as they carry a considerable risk of serious complications. Adequate patient selection is of great importance for achieving acceptable long term results.