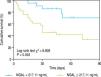
Introduction and aim. Acute-on-chronic liver failure (ACLF) is a syndrome with high short-term mortality, and predicting the prognosis is challenging. This study aimed to compare the performance of neutrophil gelatinase-associated lipocalin (NGAL) and cystatin C (CysC) in predicting the 90-day mortality in patients with hepatitis B virus (HBV)-associated ACLF (HBV-ACLF). Materials and methods. This prospective, observational study enrolled 54 patients with HBV-ACLF. The serum NGAL and CysC levels were determined. A multivariate logistic regression analysis was used to analyze the independent risk factors of mortality. Results. Serum NGAL, but not CysC, was found to significantly correlate with the total bilirubin, international normalized ratio, and model for end-stage liver disease (MELD). Serum NGAL [odds ratio (OR), 1.008; 95% confidence interval (CI), 1.004-1.012; P < 0.01], but not CysC, was an independent risk factor for developing hepatorenal syndrome. Moreover, NGAL (OR, 1.005; 95% CI, 1.001-1.010; P < 0.01) along with the MELD score was independently associated with the overall survival in patients with HBV-ACLF. Patients with HBV-ACLF were stratified into two groups according to the serum NGAL level at baseline (low risk: <217.11 ng/mL and high risk: ≥ 217.11 ng/mL). The 90-day mortality rate was 22.73% (5/22) in the low-risk group and 71.88% (23/32) in the high-risk group. Moreover, NGAL, but not CysC, significantly improved the MELD score in predicting the prognosis of HBV-ACLF. Conclusion. The serum NGAL might be superior to CysC in predicting the prognosis of HBV-ACLF with the normal creatinine level.
Acute-on-chronic liver failure (ACLF) is a syndrome of acute hepatic abnormalities resulting from insults in patients with underlying chronic hepatitis or liver cirrhosis (LC).1,2 Stratification of patients with poor prognosis and determining the emergency for liver transplantation (LT) are crucial because of the high short-term mortality of this syndrome. Specific organ dysfunction such as acute kidney injury (AKI) should be taken into consideration because the presence and numbers of organ failure are associated with prognosis.3
Serum creatinine concentration and urine output are commonly used to monitor AKI in clinical practice. However, creatinine, which could be affected by many factors associated with creatinine generation and excretion, is just a delayed and insensitive biomarker of renal function but not kidney injury.4 No reliable biomarker that can identify the incidence of AKI and predict the prognosis of endstage liver disease is yet available.4 5
Recently, the urinary neutrophil gelatinase-associated lipocalin (NGAL) was reported to serve as a biomarker to predict hepatorenal syndrome (HRS) in patients with advanced LC.6 NGAL independently predicted irreversibility of pre-LT kidney dysfunction in patients who underwent LT, but was not useful in patients with preserved pre-LT kidney function.7 Another study showed that NGAL had better accuracy for acute tubular necrosis diagnosis compared with osteopontin, albumin, and trefoil-factor-3 in patients with ACLF.8 Data from the EASLCLIF Acute-on-chronic Liver Failure (CANONIC) study showed that urinary NGAL was an independent predictive factor of 28-day mortality in patients with ACLF, and it significantly improved the accuracy of model for end-stage liver disease (MELD) in predicting the prognosis.9
Similar to NGAL, serum cystatin C (CysC) was a useful surrogate marker in predicting HRS and survival in patients with LC.10,11 Serum CysC could improve the accuracy of estimated glomerular filtration rate (eGFR) and predict the mortality in patients who underwent LT.12,13 Data from the CANONIC study showed that plasma CysC, but not NGAL, could predict the development of renal dysfunction, HRS, and ACLF, and both CysC and NGAL were independent predictors of mortality in patients with acutely decompensated LC.14
However, the etiology of underlying chronic liver disease, heterogeneity of triggering factors, and different definitions and criteria of ACLF between the East and the West, make the evaluation of the usefulness of CysC and NGAL difficult. Most of the patients in the CANONIC study suffered from acute decompensation of cirrhosis, and almost half of the patients had alcoholic cirrhosis.9 Different from the CANONIC study, hepatitis B virus (HBV) was the leading cause of ACLF in Asia-Pacific countries, and the underlying chronic liver diseases include chronic hepatitis B (CHB) and LC.15
The comparison of serum NGAL and CysC levels in patients with HBV-associated ACLF (HBV-ACLF) is limited, especially for those with a normal creatinine level. Therefore, this prospective study aimed to evaluate the performance of CysC and NGAL for predicting the 90-day mortality in patients with HBV-ACLF and normal creatinine levels at baseline.
Material and MethodsStudy design, inclusion and exclusion criteriaA total of 54 patients with HBV-ACLF and 49 patients with CHB were prospectively enrolled from January 2015 to July 2017 in the Department of Liver Diseases, the Third People’s Hospital of Changzhou, China. Moreover, healthy individuals were recruited as healthy controls. ACLF was diagnosed according to the following criteria:15
- •
Jaundice and coagulopathy resulting from insults in a patient with underlying CHB or LC.
- •
Complications including ascites and/or encephalopathy within 4 weeks.
- •
Serum total bilirubin (TBil) ≥ 5 mg/dL or 85 µ mol/L.
- •
Prothrombin activity < 40% or international normalized ratio (INR) > 1.5.
Liver-related complications, such as spontaneous bacterial peritonitis (SBP), HRS, and hepatic encephalopathy, were investigated. In short, SBP was diagnosed based on the clinical signs of infection and a neutrophil count > 250 mm3 in ascites or a positive ascitic fluid culture. HRS was diagnosed based on the serum creatinine level > 2.5 mg/dL during hospital admission.16,17 CHB was defined according to the Chinese guidelines for prevention and treatment of CHB.18 Patients were excluded if they had alcoholic cirrhosis, chronic kidney disease, autoimmune diseases, cancer, immune-compromised diseases, blood diseases, or co-infection with other hepatitis virus diseases. All the patients with HBV-ACLF were given antiviral therapy at admission, including Lamivudine, Telbivudine, Entecavir or Tenofovir. Serum samples were collected at the time of diagnosis of HBV-ACLF, and the sera were separated and stored at -80 ¯C. The endpoint of the study was the 90-day mortality after the established diagnosis of ACLF.
The study was approved by the ethics committee of the Third People’s Hospital of Changzhou according to the Declaration of Helsinki 1975. Written informed consents were obtained from all participants in the study.
Enzyme-linked Immunosorbent AssaySerum concentrations of CysC and NGAL were measured using the enzyme-linked immunosorbent assay kit (R&D Systems, Inc., MN, USA) according to the manufacturer’s instructions.
Score systemsThe MELD19 and MELD-Na20 scores were calculated using the formulas, of figure 1.
The estimated Glomerular Filtration Rate (eGFR) were calculated using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) creatinine equation (eGFR-Cr), CKD-EPI CysC equation (eGFR-CysC), and CKD-EPI creatinine-CysC equation (eGFR-Cr-CysC) as described in an earlier study.21
Statistical analysisAll data were analyzed using SPSS version 19.0 (IL, USA). Continuous variables were expressed as mean ± standard deviation, and the categorical values were expressed as frequencies. Differences in variables were analyzed using the Student t test or one-way analysis of variation (for normally distributed data). Comparisons of frequencies were performed using the χ2. The Pearson correlation analysis was used to evaluate the correlation between CysC, NGAL, and other clinical parameters. The independent risk factors were analyzed using a multivariate logistic regression analysis. The best cutoff value of NGAL for predicting the 90-day mortality was determined using SPSS Modeler 14.2 software (IBM, NY, USA), and the accuracy of prediction was compared using the area under the curve of the receiver operating characteristics (AUROC). The Kaplan-Meier curve was used for survival analysis. A two-sided P < 0.05 was considered statistically significant.
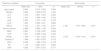
ResultsCharacteristics of subjectsThe baseline characteristics of the 54 patients with ACLF are shown in table 1. Of these patients, 48 (88.89%) were males and 6 (11.11%) were females, with an average age of 46.72 (±12.26) years. Viral cirrhosis was diagnosed in 32 (59.26%) patients. The CysC level was significantly higher in patients with ACLF and CHB compared with the healthy controls (Figure 2A). The NGAL level was significantly elevated in patients with HBV-ACLF compared with those with CHB and healthy controls (Figure 1B). The CysC and NGAL showed no significant difference between patients with ACLF having LC and not having LC (Figure 2C and Figure 2D). Data from the 90-day follow-up showed that 11 (20.37%) patients developed HRS and ultimately 28 (51.85%) patients died. Moreover, the baseline CysC and NGAL levels were significantly higher in patients who developed HRS compared with those who did not (Figure 2E and Figure 2F).
Demographic and clinical charactericts of study subjects (mean ± SD).
| Variables | ACLF (n = 54) | CHB (n = 49) | HC (n = 20) |
|---|---|---|---|
| Age (years) | 46.72 ± 12.26* # | 41.74 ± 11.51$ | 34.49 ± 10.11 |
| Male (%) | 48 (88.89%)*,# | 35 (71.43%) | 13 (65%) |
| HBeAg (positive rate, %) | 10 (18.52%) | 14 (28.57) | 0 |
| Viral cirrhosis (%) | 32 (59.26%)*,# | 0 | 0 |
| ALT (U/L) | 480.81 ± 604.13*# | 203.22 ± 57.31$ | 22.17 ± 5.29 |
| TBil (umol/L9 | 305.06 ± 154.82*# | 18.11 ± 10.01 | 12.19 ± 4.51 |
| Creatinine (umol/L) | 75.76 ± 21.88*# | 69.10 ± 18.37 | 62.78 ±11.39 |
| INR | 2.33 ± 0.95*,# | 1.32 ± 0.21 | N.D. |
| AFP (ng/mL) | 348.31 ± 641.87 | N.D. | N.D |
| WBC (E + 09/L) | 8.28 ± 4.60*,# | 4.89 ± 1.24 | 4.26 ± 1.63 |
| Neutrophil (E + 09/L) | 6.01 ± 4.19*# | 3.01 ± 0.60 | 2.99 ± 0.71 |
| MELD | 23.07 ± 5.79*,# | 6.21 ± 3.19 | N.D. |
| MELD-Na | 21.65 ± 11.24*,# | N.D. | N.D. |
| eGFR-Cr | 51.03 ± 22.07*,# | 65.31 ± 32.78$ | 71.22 ± 19.39 |
| eGFR-CysC | 24.82 ± 20.08*,# | 26.09 ± 15.11$ | 32.02 ± 22.36 |
| Cystatin C (mg/L) | 1.52 ± 0.38*,# | 145 ± 0.20$ | 1.01 ± 0.35 |
| NGAL (ng/mL) | 334.57 ± 217.20*,# | 200.86 ± 126.98 | 228.49 ±53.76 |
| HRS (%) | 11 (20.37)*,# | NO | NO |
| HE (%) | 8 (14.81)*,# | NO | NO |
| SBP (%) | 10 (18.52)*,# | NO | NO |
The baseline NGAL, but not CysC, level was significantly higher in nonsurvivors compared with survivors (Figure 1G and Figure 1H). Significant differences existed between survivors and nonsurvivors in terms of TBil (P = 0.000), INR (P = 0.001), platelet counts (P = 0.032), and MELD (P = 0.001) and MELD-Na scores (P = 0.003). No significant differences were found among baseline eGFR-Cr, eGFR-CysC, and eGFRCr-CysC levels between survivors and nonsurvivors (P > 0.05).
NGAL, but not CysC, was an independent risk factor for the development of HRSData from the logistic regression analysis showed that only NGAL and white blood cells (WBCs) were predictors of HRS [odds ratio (OR), 1.008 and 0.646, 95% confidence interval (CI), 1.004-1.012 and 0.467-0.894, respectively] (Table 2).
Risck factor for hepatorenal syndrome in patients with ACLF.*
| Baseline variables | Odds ratio | Univariate 95% | P | Odds ratio | Multivariate 95%CI | P |
|---|---|---|---|---|---|---|
| Age (years) | 0.860 | 0.703-1.052 | 0.142 | |||
| ALT | 1.003 | 0.999-1.006 | 0.152 | |||
| AST | 1.004 | 0.999-1.009 | 0.144 | |||
| ALB | 0.772 | 0.567-1.052 | 0.102 | |||
| CHE | 0.999 | 0.997-1.001 | 0.187 | |||
| MELD | 1.672 | 1.038-2.693 | 0.035 | |||
| Serum sodium | 0.688 | 0.636.1.348 | 0.688 | |||
| WBC | 0.277 | 0.091-0.848 | 0.024 | 0.648 | 0.467-0.894 | 0.008 |
| AFP | 1.000 | 0.997-1.002 | 0.764 | |||
| NGAL | 1.022 | 1.005-1.038 | 0.010 | 1.008 | 1.004-1.012 | 0.000 |
| Cystatin C | 1.172 | 0.778-6.099 | 0.069 | |||
| SBP | 0.791 | 0.221-1.996 | 0.866 |
The following parameters were tested in the univariate and multivariate logistic regression analyses to determine the potential of serum NGAL and CysC to predict the prognosis of HBV-ACLF. TBil, INR, and creatinine were not used in the logistic regression, as the MELD score was calculated using the three values. The multivariate analysis demonstrated that NGAL, along with the MELD score, was independently associated with overall survival (OR, 1.005; 95% CI, 1.001-1.010, P = 0.001) (Table 3). Then, another multivariate analysis was performed in which TBil, INR, and creatinine were included, instead of the MELD score. Data showed that serum NGAL (OR, 1.003; 95% CI, 1.001-1.005, P = 0.007), TBil (OR, 1.004; 95% CI, 1.0011.007, P = 0.020) and creatinine (OR, 0.973; 95% CI, 0.9540.993, P = 0.008) were independent risk factors associated with the mortality in patients with ACLF.
Risck factor for 90-day mortalityin patients with ACLF.*
| Baseline variables | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|
| Odds ratio | 95% | P | Odds ratio | 95%CI | P | |
| Age (years) | 0.984 | 0.916-1.058 | 0.666 | |||
| Gender | 0.509 | 0.095-2.742 | 0.433 | |||
| ALT | 1.000 | 0.997-1.003 | 0.980 | |||
| AST | 1.001 | 0.998-1.005 | 0.443 | |||
| ALB | 0.932 | 0.767-1.132 | 0.478 | |||
| CHE | 1.000 | 0.999-1.001 | 0.862 | |||
| MELD | 1.402 | 1.007-1.706 | 0.001 | 1.332 | 1.047-1.696 | 0.001 |
| Serum sodium | 0.983 | 0.808-1.195 | 0.084 | |||
| WBC | 0.981 | 0.789-1.220 | 0.864 | |||
| AFP | 1.001 | 0.999-1.002 | 0.335 | |||
| NGAL | 1.004 | 1.001-1.023 | 0.001 | 1.005 | 1.000-1.010 | 0.001 |
| Cystatin C | 1.894 | 0.481-6.235 | 0.075 | |||
| HRS | 0.468 | 1.666-1.324 | 0.153 | |||
| HE | 1.143 | 0.287-4.551 | 0.850 | |||
| SBP | 0.832 | 0.241-2.873 | 0.771 | |||
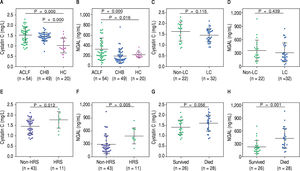
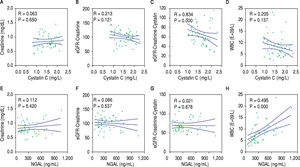
The correlations of the two biomarkers with liver injury parameters including TBil, INR, and MELD and MELD-Na scores were analyzed to further explore the clinical value of NGAL and CysC in developing HBVACLF. NGAL, but not CysC, correlated positively with TBil (P < 0.001), INR (p < 0.05), and MELD (P < 0.001) and MELD-Na scores (P < 0.001) (Figure 3). NGAL and CysC showed no significant correlation with creatinine and eGFR-cr. Reverse correlation for eGFR-Cr-CysC was found with CysC (P < 0.01), but not with NGAL (P > 0.05). Moreover, NGAL, but not CysC, significantly correlated with WBCs (P < 0.001) (Figure 4).
Three patients in the survivor group and eight patients in the nonsurvivor group developed HRS (χ2 = 2.411, P = 0.179). The multivariate logistic regression analysis showed that HRS was not an independent risk factor for the mortality in patients with ACLF (OR, 0.468; 95% CI, 0.166-1.324, P = 0.153).
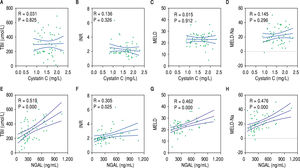
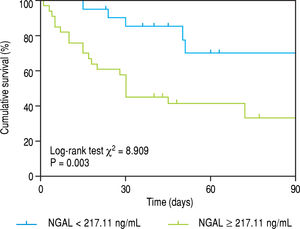
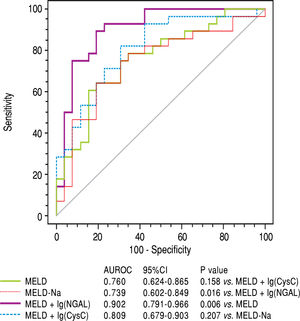
NGAL, but not CysC, significantly improved the MELD score in predicting the prognosis of HBV-ACLFBiomarkers that could stratify patients with poor prognosis or improve the accuracy of MELD score in predicting the prognosis of HBV-ACLF would be valuable in clinical practice. The patients with HBV-ACLF were stratified into two groups according to the cutoff value of NGAL level at baseline, which were identified using the SPSS Modeler 14.2 software (low risk: < 217.11 ng/mL and high risk: ≥ 217.11 ng/mL). The 90-day mortality was 22.73% (5/22) in the low-risk group and 71.88% (23/32) in the high-risk group, and those with NGAL ≥ 217.11 ng/ mL had a poor prognosis (Figure 5). The prognosis of 90 day mortality was predicted with 82.14% sensitivity, 65.38% specificity, 87.50% positive predictive value, and 77.27% negative predictive value, with 217.11 ng/mL as the cutoff value. Moreover, a novel prognostic model, combining MELD and lg (NGAL), showed significant superiority in the accuracy of prognostic prediction compared with MELD and MELD-Na scores (AUROC: 0.902, 0.760, and 0.739, respectively, P = 0.006 and 0.015) (Figure 6). In contrast, another prognostic model, which combined MELD and lg (CysC), showed no significant superiority compared with MELD and MELD-Na scores (AUROC: 0.809, 0.760, and 0.739, respectively, P = 0.158 and 0.207) (Figure 6).
At present, precisely predicting the prognosis in patients with HBV-ACLF is still challenging. Plasma CysC and NGAL, which are predictors of renal dysfunction, predicted the prognosis of patients with decompensated LC more accurately.14 However, a few data are available regarding the accuracy of serum CysC and NGAL in predicting the prognosis of HBV-ACLF. The present study demonstrated that serum NGAL, but not CysC, significantly correlated with TBil, INR, and MELD and MELDNa scores, and helped differentiate between nonsurvivors and survivors. Furthermore, this study showed that serum NGAL, but not CysC, is an independent risk factor for the development of HRS, and NGAL along with the MELD score, was independently associated with the overall survival in patients with HBV-ACLF.
Data from the CANONIC study, which is a multicenter research concerning the prognosis of ACLF in European countries, showed that both NGAL and CysC were significant predictors of mortality;9,14 several reasons might contribute to the distinction from the present study. First, the definitions of ACLF remained different for the East and the West, resulting in ambiguity and heterogeneity in defining patients with ACLF. Second, the patients’ background and etiologies of liver diseases were different, and the exact pathogenesis remained unclear. Patients in the CANONIC study were enrolled from European countries, and most of them suffered from acute decompensation of cirrhosis. The criteria of ACLF were based on the presence of organ failure(s) as defined according to the CLIF-SOFA score, and almost half of the patients had alcoholic cirrhosis. Different from the CANONIC study, HBV was the cause of ACLF in the present study, and the underlying chronic liver diseases included CHB and LC with the normal creatinine level at baseline. Third, the kidneys were the most commonly affected organs (55.8% of patients) in the CANONIC study, followed by the liver (43.6% of patients), coagulation (27.7% of patients), and other organs, while in the present study, liver and coagulation failures were present in every patient, and the creatinine level was normal at inclusion. Thus, the findings of the present study were more valuable for patients from the Asian-Pacific regions.
Previous studies showed that NGAL was produced mainly by neutrophils, and could protect against bacterial infection.22 Its expression was upregulated and the urinary level of NGAL was increased in AKI, and it might play a protective role in kidney cells.23 The expression of NGAL increased mainly in hepatocytes, as demonstrated in the liver tissue of patients with ACLF.9,24 The systemic inflammatory response parallels renal injury in patients with ACLF, and NGAL could reflect the comprehensive effect of both aspects.1,25 Consistent with a previous study,9 the present study showed that the serum NGAL level was significantly higher in patients with ACLF, and it positively correlated with TBil, INR, and MELD and MELD-Na scores. In contrast, CysC, a predictor of renal dysfunction, showed no significant correlation with the severity parameters of liver injury in the present study. Thus, for patients with ACLF with the normal serum creatinine at baseline, NGAL might predict the prognosis of ACLF more accurately. These observations provide an understanding of the predictive value of NGAL in HBV-ACLF.
Although the NGAL level was valuable in predicting renal dysfunction and mortality in patients with ACLF and normal creatinine levels, whether NGAL level is directly implicated in ACLF or indirectly through the development of HRS needs further clarification. The multivariate logistic regression analysis showed that HRS was not an independent risk factor for the mortality in patients with ACLF. Moreover, NGAL showed no significant correlation with creatinine, eGFR-Cr, and eGFR-Cr-CysC. These suggested that NGAL might be indirectly implicated in ACLF and not only through the development of HRS.
Considering that renal failure is an important complication of ACLF, predictors for the development of HRS were increasingly recognized as important. The present study evaluated the parameters of renal functions in the prognosis of HBV-ACLF. CysC and eGFRCysC were reported to be superior to creatinine and eGFR-Cr in diagnosing secondary kidney injury, and eGFR-Cr-CysC, which combined creatinine and CysC, had a better diagnostic performance.21,26-28 Furthermore, Mindikoglu, et al. reported that eGFR-Cr-CysC was superior to conventional equations in patients with LC, but it was not superior for patients without LC.29 Data in the present study showed that baseline CysC, eGFR-CysC, and eGFR-Cr-CysC were disappointing in predicting the prognosis of HBV-ACLF with normal serum creatinine. Additionally, Wan, et al.30 reported that serum CysC and TBil were independent risk factors for mortality in patients with ACLF; however, TBil, INR, and MELD and MELD-Na scores were all included in the univariate and multivariate logistic analyses in their study. Considering that both MELD and MELD-Na scores were calculated using TBil, INR, and creatinine, it would be rigorous to analyze TBil, INR, and MELD (or MELD-Na), rather than putting them together in the logistic regression analysis.
This study had several limitations. First, although the baseline NGAL level clearly correlated with the prognosis of ACLF, the sources of NGAL and the mechanisms underlying the role of NGAL were not explored. Second, the number of patients with ACLF was comparatively limited, and a multicenter study with a large sample size is required to confirm the current findings. Moreover, urinary levels of NGAL and CysC were not compared in the present study.
In conclusion, serum NGAL, but not CysC, significantly correlated with liver injury in patients with HBVACLF, and it is an independent risk factor associated with the prognosis of HBV-ACLF. Together, these findings suggested that serum NGAL might be superior to CysC in predicting the prognosis of HBV-ACLF in patients with a normal creatinine level.
Abbreviations- •
95% CI: 95% confidence interval.
- •
ACLF: acute-on-chronic liver failure.
- •
AFP: alpha fetoprotein.
- •
AKI: acute kidney injury.
- •
ALB: albumin.
- •
ALT: alanine aminotransferase.
- •
AST: aspartate aminotransferase.
- •
AUROC: the area under the receiver operating characteristic curve.
- •
CHB. chronic hepatitis B.
- •
CHE: cholinesterase.
- •
CysC: cystatin C.
- •
eGFR: estimated glomerular filtration rate.
- •
HBeAg: hepatitis B e antigen.
- •
HBsAg: hepatitis B surface antigen.
- •
HBV: hepatitis B virus.
- •
HC: healthy control.
- •
>HE; hepatic encephalopathy.
- •
HRS: hepatorenal syndrome.
- •
INR: international normalized ratio.
- •
LC: liver cirrhosis.
- •
LT: liver transplantation.
- •
MELD: model for end-stage liver disease.
- •
NGAL: Neutrophil Gelatinase-associated Lipocalin.
- •
SBP: spontaneous bacterial peritonitis.
- •
TBil: total bilirubin.
- •
WBC: white blood cells.
The authors declares that there is no conflict of interest regarding the publication of this article.
Financial SupportThis work was supported by grants from the Chinese Foundation for Hepatitis Prevention and Control-Tianqing Liver Disease Research Fund Subject, (TQGB201700139), the Major Projects of Changzhou Municipal Healthy and Family Planning Commission (ZD2011002), and the Projects of Changzhou Science and Technology Commission (CJ20160024).
AUTHORS’ ContributionsYuan Xue conceived and designed the study. Jianchun Lu, Lin Lin, Chunyan Ye, Qian Tao, Manman Cui, Shuqin Zheng, Dongmei Zhu and Longgen Liu collected and confirmed the data. Jianchun Lu and Lin Lin performed the experiments, analyzed the data and drafted the manuscript. All authors read and approved the final manuscript. Jianchun Lu and Lin Lin contributed equally to this work.